When you're starting on 5-fluorouracil, you'll likely hear about a few common side effects, like fatigue, nausea, diarrhea, and mouth sores. Some people also experience more specific issues, such as Hand-Foot Syndrome or a dip in their blood cell counts. The side effects you experience really depend on your specific dose and how the drug is given.
Your Guide to Navigating 5-FU Treatment

Starting chemotherapy with 5-fluorouracil (5-FU) can feel overwhelming, almost like you're heading into uncharted territory. Knowing what might be around the corner is the first, most important step toward feeling prepared and in control.
It helps to think of 5-FU as a powerful medication designed to find and stop cancer cells, which are known for dividing very quickly. The catch is that 5-FU can’t always tell the difference between a cancer cell and other healthy cells in your body that also happen to divide rapidly. This is the root cause of the most common 5-fluorouracil side effects, and this guide is here to be your roadmap through it all.
What to Expect on Your Treatment Path
We'll walk through the most common bumps in the road you might face, from that all-too-familiar feeling of fatigue and digestive upset to more specific issues like Hand-Foot Syndrome. But it’s so important to remember that everyone's journey with 5-FU is different.
What you experience will be influenced by a few key things:
- Your overall health and even your genetics: Your body's unique makeup plays a huge role in how you respond.
- The specific dose you're given: It stands to reason that higher doses can sometimes lead to more noticeable side effects.
- How the drug is administered: This is a big one. Whether you get a quick injection (a "bolus") or a slow, continuous drip ("infusion") can dramatically change the side effect picture.
For example, we often see that a rapid bolus injection is more likely to cause a drop in blood counts. On the other hand, a slow, steady infusion is more frequently linked to skin reactions on the hands and feet. Understanding these tendencies helps you and your oncology team know what to watch for.
Our goal here is simple: to pull back the curtain on the treatment process. We want to give you practical, real-world advice that empowers you to be an active partner in your own care. Never forget that open communication with your healthcare team is your best tool.
Proactive Preparation is Key
When you understand what might happen, you can start taking steps to manage it before it becomes a major problem. This means knowing which symptoms you can handle at home and, just as importantly, which ones mean you need to pick up the phone and call your doctor.
For more on getting set for your first day of treatment, check out our in-depth guide on how to prepare for chemotherapy. It’s packed with helpful checklists and advice.
We built this guide to give you a sense of clarity and confidence. By understanding the "why" behind 5-fluorouracil side effects, you can navigate your treatment more smoothly, speak up for your needs, and keep your focus where it belongs: on getting better.
What to Expect From Common 5-FU Side Effects
Knowing what to expect from 5-fluorouracil side effects is the first step in feeling more in control of your treatment. Because 5-FU is designed to stop rapidly dividing cells, it can’t always tell the difference between a cancer cell and a healthy, fast-growing cell. This is why you’ll often see side effects pop up in areas like your digestive tract, your bone marrow, and your skin.
Think of it this way: your body is a bustling city, and cancer cells are construction projects that are growing out of control. 5-FU is sent in to halt all the frantic building. While it's great at stopping those rogue projects, it might also temporarily slow down some normal, essential city services that also work on a fast schedule—like road repair (your gut lining) or emergency services (your immune cells).
The good news is that we know what to look for. These effects are usually predictable, temporary, and very manageable with a bit of proactive care.
Digestive System Discomfort
Your entire gastrointestinal (GI) tract, from your mouth all the way down, is lined with cells that replace themselves every few days. Since 5-FU targets anything that grows quickly, it’s no surprise that your digestive system is often one of the first places to feel the impact.
Here are the most common digestive issues we see:
- Nausea and Vomiting: This isn't as severe as with some other chemotherapy drugs, but mild to moderate nausea can certainly happen. It usually starts a few hours to a day after your infusion, which is why your oncology team will give you anti-nausea medications right from the start to get ahead of it.
- Diarrhea: This is a very common one, especially for patients on a continuous 5-FU infusion pump. The drug can irritate the lining of your intestines, making them push waste through much too quickly.
- Mucositis (Mouth Sores): Painful little sores can develop on your tongue, gums, and the inside of your cheeks. They tend to show up about 5 to 10 days after treatment begins and can make eating and drinking a real challenge.
Studies show that GI issues are quite common, with nausea, vomiting, and diarrhea affecting up to 70% of patients. Similarly, mucositis can occur in up to 40% of people. You can read more about the toxicity rates of 5-fluorouracil on cancernetwork.com.
Proactive Tip: Start a gentle mouth care routine on day one. Don't wait for sores to appear. Use a soft-bristle toothbrush and rinse your mouth several times a day with a non-alcoholic wash, like a simple mix of baking soda and salt in warm water. This keeps your mouth clean and can dramatically reduce how severe the sores get.
Common 5-FU Side Effects Timeline and Management
To help you anticipate and manage these effects, here’s a quick look at what to expect and when. This table summarizes some of the most common issues, their typical timing within a treatment cycle, and some simple first steps you can take.
Remember, these are just initial tips. It is crucial to report any and all side effects to your oncology team, as they can provide targeted medications and more specific guidance to keep you comfortable.
Changes in Your Blood Counts
Deep inside your bones is the bone marrow, a busy factory that’s constantly making red blood cells, white blood cells, and platelets. Because these cells are also produced rapidly, 5-FU can temporarily slow the factory down. We call this myelosuppression.
This is one of the most important things we monitor during your treatment. Myelosuppression happens in up to 50% of patients who get 5-FU as a rapid "bolus" injection. Your team will check your blood work regularly, looking for three key changes:
- Neutropenia (Low White Blood Cells): Neutrophils are your immune system's frontline soldiers against infection. When their numbers drop, you’re more vulnerable to getting sick.
- Anemia (Low Red Blood Cells): These cells carry oxygen around your body. When they're low, you can feel incredibly tired, breathless, and weak. This is often the "chemo fatigue" people talk about.
- Thrombocytopenia (Low Platelets): Platelets are what help your blood clot. Low levels mean you might bruise more easily or notice bleeding from small cuts takes longer to stop.
The timing of this dip is predictable. Your blood counts typically hit their lowest point, which we call the nadir, about 7 to 14 days after a treatment cycle starts. For more helpful advice, see our comprehensive guide on managing side effects of cancer treatment.
Skin Reactions and Hand-Foot Syndrome
Your skin also has a high rate of cell turnover, making it another area that can be affected by 5-FU. Some people might just notice a mild rash, become more sensitive to the sun, or see some skin darkening along the veins where the IV was placed. But the most well-known skin reaction is Hand-Foot Syndrome (HFS).
Also called palmar-plantar erythrodysesthesia, HFS is especially common with continuous infusions of 5-FU. It happens when tiny amounts of the drug leak out of the small blood vessels in your palms and the soles of your feet, causing an inflammatory reaction.
Symptoms of Hand-Foot Syndrome often progress in stages:
- Early Stage: You might first notice some numbness, tingling, or redness on your palms and soles. It might not be painful yet, just… different.
- Developing Stage: This can progress to uncomfortable swelling, tenderness, and pain that makes it hard to hold things or stand for long periods.
- Advanced Stage: If it isn't managed, the skin can blister, peel, or form painful cracks. This can make simple daily tasks, like buttoning a shirt or walking, very difficult.
The best way to deal with HFS is to get ahead of it with prevention and early action. Protecting your hands and feet from friction, pressure, and heat is absolutely essential, right from the very beginning of your treatment.
Recognizing Urgent Symptoms That Need Attention
While most side effects from 5-fluorouracil are manageable, some can be red flags for a serious problem that needs immediate medical care. Think of it like this: most symptoms are like a "check engine" light—important to address, but not an emergency. This section is about spotting the flashing, pull-over-now warning signs.
Knowing what to look for isn't about causing anxiety; it's about empowerment. When you can identify a critical symptom, you can act fast to protect your health. We’ll walk through the signs you should never ignore and give you clear steps on when to call your oncology team versus when to head straight to an emergency room.
It’s also helpful to know that how you receive 5-FU—as a quick injection (bolus) or a slow infusion—changes the side effects you're most likely to see.
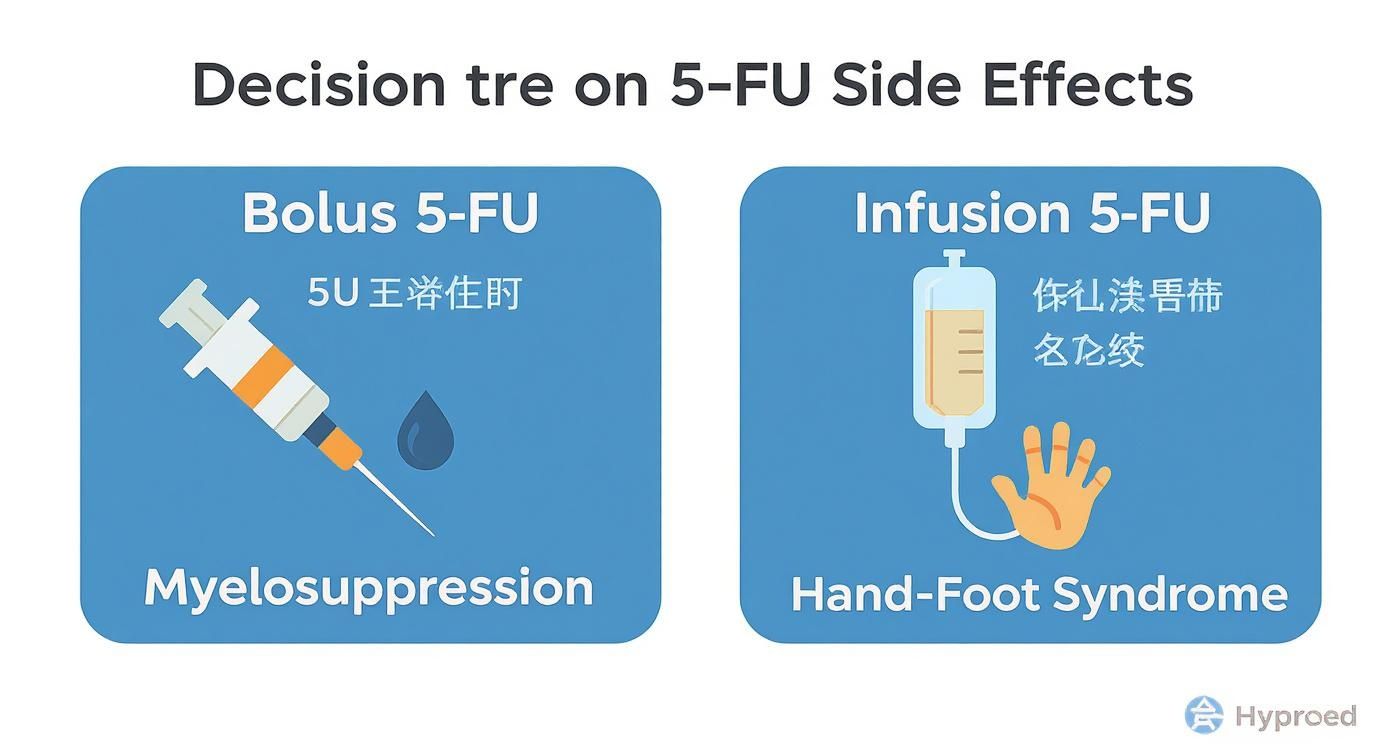
This distinction helps you and your care team focus on the most relevant risks for your specific treatment plan.
Signs of a Serious Infection
One of 5-FU's main jobs is to stop fast-growing cells, but that unfortunately includes your white blood cells. When these cell counts drop (a condition called neutropenia), your body's ability to fight germs plummets. A simple cold or minor infection can suddenly become a medical emergency.
That’s why a fever during chemotherapy is always taken so seriously. It’s often the first and only clue that a dangerous infection is brewing.
Contact your medical team immediately if you experience:
- A fever of 100.4°F (38°C) or higher.
- Shaking chills, even if you don’t have a fever.
- A new cough, sore throat, or feeling short of breath.
- Any signs of localized infection, like redness, swelling, or pus around a cut or IV site.
- A burning sensation or pain when you urinate.
Never try to "wait out" a fever. Your oncology team has a strict protocol for this. They will want to evaluate you right away, even if you feel fine otherwise, because an infection can become life-threatening very quickly when your immune system is down.
Potential Heart-Related Issues
Though it’s not common, 5-fluorouracil can sometimes irritate or damage the heart muscle, a side effect known as cardiotoxicity. The symptoms can feel very much like a heart attack and should always be treated as an emergency.
While rare, cardiotoxicity is a serious risk. Global data suggests about 0.55% of patients experience severe cardiac events. The most frequent symptom is chest pain (angina), which has been reported in 2-18% of patients. These issues can pop up even during the very first infusion, which is why close monitoring is so important. You can find more detail on these cardiac side effects and their management on pmc.ncbi.nlm.nih.gov.
Go to the nearest emergency room if you have:
- Chest pain, pressure, or a squeezing sensation, especially if it spreads to your arm, jaw, or back.
- Shortness of breath or difficulty breathing that comes on suddenly.
- A racing, pounding, or fluttering heartbeat (palpitations).
- Sudden dizziness, lightheadedness, or fainting.
These symptoms demand an immediate medical workup to rule out a serious heart issue.
Severe Digestive Problems
Mild diarrhea and mouth sores are unfortunately common with 5-fluorouracil, but they can escalate. If they become severe, they can quickly lead to dangerous complications like dehydration, malnutrition, and widespread infection.
It's crucial to let your team know when these manageable side effects cross a certain line.
Call your doctor or nurse if you experience:
- Severe Diarrhea: Generally defined as six or more loose stools in 24 hours, or any diarrhea that lasts more than two days.
- Signs of Dehydration: Feeling dizzy when you stand up, having a very dry mouth, passing dark-colored urine, or not being able to urinate for more than eight hours.
- Uncontrollable Vomiting: Not being able to keep any liquids down for more than 12-24 hours.
- Inability to Eat or Drink: This is often caused by painful mouth sores that make it impossible to get the nutrition and fluids your body needs.
- Blood in Your Stool or Vomit: This might look like bright red blood, or it could make your stool look black and tarry.
Your team can step in with stronger medications, IV fluids, and other support to stop the problem from getting worse. Staying vigilant and speaking up is your best line of defense.
Understanding DPD Deficiency and Neurological Risks
https://www.youtube.com/embed/wugBCAEnzD8
While most side effects from 5-fluorouracil are manageable, some people carry a hidden genetic risk that can make the drug far more toxic. It all comes down to a single enzyme, and it’s a perfect example of why personalized medicine is so important for keeping chemotherapy safe and effective.
Sometimes, patients on 5-FU develop neurological symptoms that seem to come out of nowhere—sudden confusion, dizziness, poor coordination, or trouble with balance. These aren't your typical side effects and can be a red flag for a rare but very serious toxic reaction in the central nervous system. When this happens, it often points to an underlying genetic condition.
That condition is called Dihydropyrimidine Dehydrogenase (DPD) deficiency. Getting a handle on what this means is key to understanding why your unique genetic makeup plays such a big role in your cancer treatment.
What Is The DPD Enzyme?
Think of the DPD enzyme as your body’s dedicated cleanup crew for 5-fluorouracil. After the chemo has done its work attacking cancer cells, this enzyme gets to work breaking it down and clearing it safely from your system. It’s a natural, efficient process that keeps the drug from hanging around too long and damaging healthy cells.
When this system is working as it should, your body handles the 5-FU dose just fine. But if there’s a problem with the cleanup crew, the drug can build up to dangerous levels.
A DPD deficiency is like having a slow-draining sink. When you pour in the 5-FU, the enzyme system just can't clear it out fast enough. The drug level rises, becoming toxic and leading to severe, and sometimes life-threatening, side effects.
This is an inherited genetic variation, meaning your body produces a DPD enzyme that’s either less effective than it should be or completely non-functional. Because of this, even a standard dose of 5-FU can feel like a massive overdose to your system.
The Connection Between DPD and Severe Side Effects
For people with a partial or complete DPD deficiency, the risk of severe toxicity is much, much higher. This isn't just about the neurological issues I mentioned earlier. It can also mean extreme versions of more common side effects, like life-threatening diarrhea, severe mouth sores (mucositis), and dangerously low blood counts.
The link to neurotoxicity is especially concerning. Although it’s uncommon, a condition called acute cerebellar syndrome—marked by symptoms like poor muscle control (ataxia), involuntary eye movements, and trouble with coordinated movements—can pop up in 1-2% of all patients getting 5-FU. That risk is significantly higher for those with DPD deficiency, a condition that affects about 3-5% of the population and is strongly tied to severe neurotoxicity. If you're interested in the science, you can read the full research about these genetic risks.
Recognizing this risk has fundamentally changed how many of us approach 5-FU treatment.
Why Your Doctor May Recommend Genetic Testing
Because a DPD deficiency can lead to such serious problems, many oncologists now recommend screening for it before a patient gets their first dose of 5-FU. This is personalized medicine in its purest form—using your genetic information to make your treatment safer.
The screening is a simple blood test that checks for specific variations in the DPYD gene, which is the gene that provides the instructions for making the DPD enzyme.
The results from this test give your doctor crucial information to:
- Identify Your Risk Level: The test will show whether you have a normal, partially deficient, or completely deficient DPD enzyme.
- Adjust Your Dose Accordingly: If a partial deficiency is found, your oncologist will likely start you on a much lower dose of 5-FU to avoid severe side effects.
- Choose a Different Treatment: For patients with a complete DPD deficiency, 5-FU is generally considered too dangerous. Your doctor will almost certainly recommend a different chemotherapy drug.
This proactive step helps prevent a severe toxic reaction before it has a chance to happen. Understanding your own genetic blueprint is a powerful tool in modern cancer care. You can learn more by reading our article on the role of genomic testing in developing personalized treatment plans. This simple test can truly make a world of difference in your treatment journey.
How Your Medical Team Keeps You Safe

Going through 5-FU treatment isn’t something you do alone—it's a true partnership with your oncology team. We have a game plan designed to watch over your health, get ahead of any challenges, and step in with support long before a small issue becomes a big problem. Think of us as your personal safety crew, always checking the gauges to make your treatment as manageable as it can be.
This whole process is built on careful monitoring, personalized adjustments, and, most importantly, open communication. You are the most critical member of this team because how you feel and what you report guides every decision we make.
Proactive Monitoring Through Blood Work
Before every treatment cycle, you'll start with a blood draw. This isn't just a box to check; it’s a crucial safety measure that gives your doctor a real-time snapshot of how your body is handling the chemotherapy. These tests, typically a Complete Blood Count (CBC), are our early warning system.
We look very closely at a few key numbers:
- White Blood Cells: Specifically your neutrophils, which are your body's frontline soldiers against infection.
- Red Blood Cells: These are the oxygen-carriers, and when they're low, you feel that deep, draining chemotherapy fatigue.
- Platelets: These little cells are vital for clotting blood and preventing bleeding.
If any of these counts fall too low, giving you the next dose of 5-FU could do more harm than good. These regular blood tests are how we confirm your body is ready and resilient enough for the next round.
The Strategy of Dose Modification
If side effects start to feel overwhelming or your blood counts drop significantly, your oncologist might suggest a dose modification. This is an incredibly common and standard part of cancer care. It absolutely does not mean your treatment is failing. It means your doctor is expertly fine-tuning the therapy to fit your body's unique response.
A dose modification could mean one of two things:
- Reducing the Dose: We might lower the amount of 5-FU you receive in your next cycle.
- Delaying a Treatment: Sometimes, we'll simply push your next infusion back by a week or so, giving your body extra time to bounce back.
This kind of personalized adjustment is at the heart of good oncology care. Changing the dose is a strategic move to keep the treatment working against the cancer while dialing back the toxicity, helping you stay on therapy safely for as long as it's needed.
Supportive Medications and Care
Your medical team also comes prepared with a whole toolkit of supportive medications to prevent and manage 5-fluorouracil side effects. These aren't just an afterthought; they're built right into your treatment plan from the very beginning.
This could include powerful anti-nausea medications given right before your infusion, prescriptions to get diarrhea under control, or special mouthwashes to soothe or prevent painful mouth sores. For patients whose white blood cell counts drop quite a bit, we can even prescribe injections that tell your bone marrow to ramp up production of those infection-fighting neutrophils.
In the end, your safety hinges on that open dialogue we talked about. By telling us about every symptom—no matter how small it might seem—you give your team the information we need to use these tools effectively. It's this partnership that allows us to manage side effects proactively, keeping you safe and improving your quality of life all the way through treatment.
Your Questions About 5-FU Side Effects Answered
When you're navigating cancer treatment, questions are going to pop up. It's completely normal. You'll wonder about the big picture, of course, but also about the day-to-day things—what to expect and how you'll feel. This section is here to tackle some of the most common and pressing questions we hear from patients about 5-fluorouracil side effects. Our goal is to give you clear, practical answers so you can feel more prepared and in control.
Will I Lose My Hair on 5-Fluorouracil?
This is often one of the very first things people ask, and it's a valid concern. While we often associate chemotherapy with significant hair loss, that classic image isn't the typical experience with 5-FU. When 5-FU is given by itself, complete baldness is actually quite rare.
What most patients see is some degree of hair thinning. The amount can depend on your specific treatment plan. If your regimen combines 5-FU with other drugs, like in the FOLFOX combination, those other agents can increase the chances and severity of hair loss.
This thinning usually starts to show up about two or three weeks after your first treatment cycle. The best news? It's almost always temporary. Your hair will start its journey back a few weeks after your treatment course is finished.
How Can I Prevent Hand-Foot Syndrome?
There's no surefire way to prevent Hand-Foot Syndrome (HFS) entirely, but you can absolutely take proactive steps to lessen its impact. The whole strategy boils down to one key idea: minimize heat, friction, and pressure on your hands and feet, especially during that first week after your infusion.
Think of it as giving these sensitive areas a bit of a vacation from stress. Here are a few practical tips that really help:
- Stay Cool: Avoid taking long, hot showers or soaking in a hot tub. Stick to lukewarm water. Many patients also find that gently applying cool packs to their hands and feet for 15-20 minutes at a time brings real relief.
- Go Easy on Friction: After washing your hands or feet, gently pat them dry instead of rubbing them with a towel. For the first few days after treatment, try to avoid activities that cause a lot of rubbing, like gardening, using hand tools, or even jogging.
- Lighten the Pressure: Opt for loose, comfortable shoes with good cushioning inside. If you can, try to avoid standing or walking for long stretches at a time.
- Moisturize, Moisturize, Moisturize: Apply a thick, alcohol-free cream or ointment to your hands and feet several times a day. This keeps your skin’s natural barrier strong and resilient.
The single most important thing you can do is tell your oncology team at the very first sign of HFS—even if it's just a little tingling, redness, or tenderness. Catching it early is the key to stopping it from becoming more severe and painful.
How Long Do Side Effects from 5-FU Last?
The timeline for 5-fluorouracil side effects can vary, but the good news is that most are temporary and follow a fairly predictable pattern tied to your treatment schedule.
Acute side effects—things like nausea, fatigue, diarrhea, and mouth sores—usually kick in a few days after your infusion. They tend to be at their worst within that first week and then gradually get better as you get closer to your next cycle. For most people, these issues clear up completely within a few weeks of their final treatment.
Some effects, however, can stick around a bit longer. Nerve changes like numbness or tingling, which often come from other chemo drugs given alongside 5-FU, might take several months to fully improve. Skin discoloration from HFS can also take a while to fade. It's crucial to keep your medical team in the loop about any symptoms that linger so they can help you manage your long-term recovery.
Is There a Difference Between Bolus and Infusion 5-FU Side Effects?
Yes, absolutely. The way 5-FU is given—as a quick "push" injection (bolus) or over a longer period through a drip (continuous infusion)—makes a big difference in the types of side effects you're most likely to see. Your oncologist chooses the method that will be most effective against your specific cancer, always weighing the benefits against these potential side effects.
Here’s a simple way to think about the differences:
Knowing which type of 5-FU you're receiving helps you and your care team anticipate what to look for. It allows everyone to be more proactive about managing symptoms, empowering you to be an active and knowledgeable partner in your own care.
At Hirschfeld Oncology, we believe that a well-informed patient is an empowered patient. Dr. Hirschfeld and our team are dedicated to providing personalized care that includes open communication and thorough education about your treatment. If you are exploring options for advanced cancer care, we invite you to request a consultation to discuss a path forward. Learn more about our approach at https://honcology.com/blog.





.png)


.png)
.png)




