Waking up after breast cancer surgery can be a disorienting, emotional experience. It's completely normal to feel a bit lost. But knowing what’s coming down the pike—from the recovery room to your first few weeks back home—can make a world of difference. Your journey back to yourself is a marathon, not a sprint, and this first leg is all about rest, proper wound care, and listening to your body.
Your First Days and Weeks After Surgery
The time right after your procedure is foundational. Think of it as laying the groundwork for a smooth and successful recovery. Your only job is to heal, manage your comfort level, and follow the game plan your surgical team has laid out for you. When you understand what each day is meant to accomplish, you can trade anxiety for a sense of purpose.
Your immediate post-op experience starts in the post-anesthesia care unit (PACU). Here, dedicated nurses will keep a close eye on you as the anesthesia wears off. Once you're stable, you'll be moved to a regular hospital room. Most patients stay for one to three days, though this can be a bit longer if you had breast reconstruction done at the same time as your mastectomy.
Navigating Your Hospital Stay
During your hospital stay, the focus is squarely on three things: keeping pain manageable, watching over your incision site, and getting you prepped to head home. Pain medication will be given on a regular schedule to stay ahead of discomfort, and your nursing team will walk you through the basics of caring for your incision and any surgical drains.
You can expect a whole range of new physical feelings. Don't be alarmed; they're all part of the process.
- Tiredness: You'll likely feel a deep, bone-weary fatigue. That's just your body responding to the anesthesia and the stress of a major operation.
- Soreness: It’s normal to feel sore and tender around your chest, armpit, and even your shoulder.
- Numbness or Tingling: As nerves in the area begin to heal and wake up, you might notice some strange tingling or numb patches. This is very common.
"You should never be on bed rest after a mastectomy. Patients should be up and walking, with supervision, on the same day as surgery. Patients should ideally walk 3-4 times per day to get moving again and to help decrease the risk of blood clots and pneumonia."
It might seem like the last thing you want to do, but getting up and moving around a little is one of the best things for your recovery. This early, gentle activity is a game-changer. Below is a quick look at what you can generally expect.
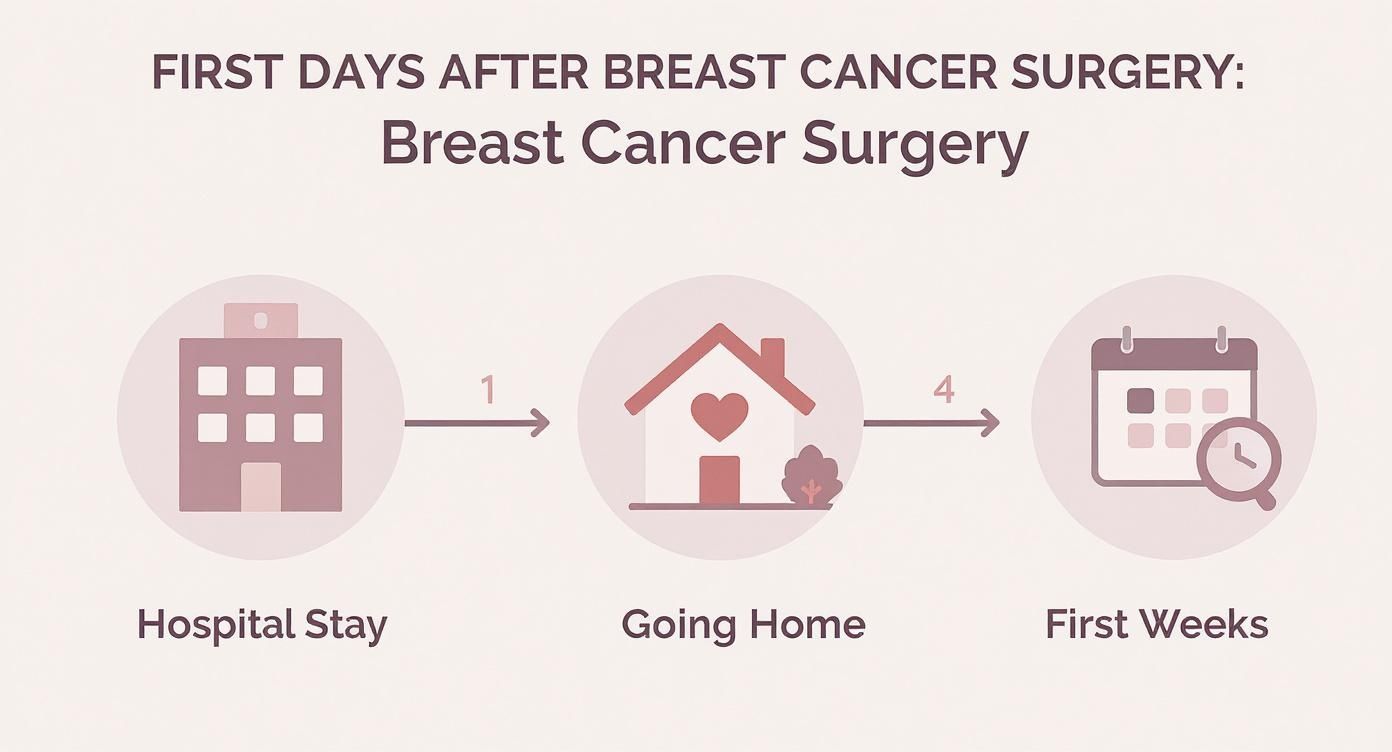
This simple roadmap helps visualize the key stages of early healing, showing that each phase has its own specific goals and priorities.
To give you a clearer picture of the initial recovery arc, here’s a quick-glance table of what to anticipate.
Post-Surgery Recovery Timeline At a Glance
This table breaks down the typical milestones you'll encounter during the first six weeks.
Remember, this is just a general guide. Everyone's healing journey is unique, so listen to your body and your care team.
The Transition to Home Care
Going home is a huge step! It’s exciting, but it also means you’re now the one in the driver's seat. Your main tasks will be managing surgical drains, keeping an eye on your incision, and watching for any red flags that could signal an infection. Your team will give you a full rundown before discharge, but it's a great idea to keep a small notebook to log drain output and jot down any questions that pop up.
It’s also helpful to see this surgery in the context of your overall cancer treatment. The stage of the cancer at diagnosis plays a huge role in what comes next. In the U.S., about 66% of breast cancer cases are found when the cancer is still localized (contained to the breast). For these women, surgery is incredibly effective, and the 5-year relative survival rate is over 99%.
This is why your post-surgical care is so crucial. A strong recovery paves the way for you to start any follow-up (adjuvant) therapies your oncologist might recommend, like chemotherapy or radiation. These next steps are designed to wipe out any remaining cancer cells and give you the best possible long-term outcome. For a deeper dive into these options, you may find our comprehensive overview of breast cancer treatment helpful.
Managing Pain and Discomfort After Surgery

Let's talk about what to expect in terms of pain and discomfort after your surgery. Your body has just been through a major event, and feeling some pain is a completely normal part of the healing process. Getting a handle on what you might feel can make the entire experience feel much more manageable.
You'll likely notice a few different kinds of sensations. The pain won't be just one-note; it can feel like a sharp, specific pain right at your incision, or it might be a broader, dull ache across your chest. It's also very common to feel tingling or "pins-and-needles" as the nerves in the area begin to wake up and heal.
A Two-Pronged Approach to Pain Relief
Your care team will set you up with a solid plan for managing pain, which almost always combines medication with other non-medical comfort strategies. The real key here is to stay ahead of the pain—not to wait until it's overwhelming and then try to chase it down. This proactive approach will make your recovery feel so much smoother and allow you to do the gentle movements that are so important for healing.
Most women are sent home with a prescription for pain medication, which might be an opioid for the first few days, along with instructions on using over-the-counter options like Tylenol or Advil.
- Stick to the Schedule: For the first 48-72 hours, it's crucial to take your medication exactly as prescribed. Don't wait until you're in severe pain to take it.
- Keep a Log: It sounds simple, but jotting down when you take each dose in a notebook or phone app is a lifesaver. It helps you avoid accidentally taking too much and keeps your pain relief consistent.
- Taper Off Slowly: As you start feeling better, your team will guide you on how to gradually reduce the stronger prescription drugs and switch over to over-the-counter relief.
Think of your body as your guide. Pain is its way of telling you to slow down, rest, or change your position. Listening to those signals isn't a sign of weakness—it's the smartest thing you can do for a strong recovery.
Non-Medical Comfort Measures That Really Work
Medication is essential, but it’s only half the story. Bringing in a few simple, non-medical techniques can make a world of difference in your comfort and help you feel more in control of your own healing.
A cold pack can be your best friend. Applying a gel pack (wrapped in a light towel) to swollen spots for 15-20 minutes can work wonders to reduce inflammation and numb the area. Just be sure never to put ice directly on your skin, especially near the incision where your skin's sensitivity might be a bit off.
The way you position your body is another game-changer.
- Embrace Pillows: Use plenty of pillows to prop up your upper body and support your arm on the surgery side. This simple trick helps drain fluid, reduce swelling, and take the strain off your chest.
- Try a Recliner: Many patients swear by sleeping in a recliner for the first week or two. It’s often far more comfortable than lying flat and makes getting in and out of a resting position much easier.
- Practice Relaxation: Don't underestimate the power of simple deep breathing, listening to quiet music, or trying a guided meditation app. These techniques help your muscles release tension and can actually lower your brain's perception of pain.
Pain is just one of the things you'll navigate during your cancer treatment. For a broader look at what to expect, check out our helpful guide on managing the side effects of cancer treatment, which is full of practical tips.
Gentle Movement for Mobility and Lymphedema Prevention
While plenty of rest is on the agenda, I can't stress enough how important gentle, purposeful movement is to your recovery. Think of it as waking your body up slowly and carefully after a major event. Once your surgeon gives you the green light, starting a simple exercise routine is one of the best things you can do to get your arm and shoulder mobility back.
More than that, it’s your number one defense against a long-term condition called lymphedema. This isn't about pushing through pain or "getting back to the gym." It’s about listening to your body, gently encouraging circulation, and taking an active role in your own healing.
What Is Lymphedema, Anyway?
To get why movement is so crucial, it helps to understand a little about your lymphatic system. Imagine it as your body’s sophisticated plumbing and filtration network. It’s a series of vessels that move a clear fluid called lymph, which is full of infection-fighting white blood cells. This system is constantly working to clear out waste and toxins from your tissues.
During breast cancer surgery, particularly if lymph nodes were removed from under your arm (an axillary dissection), this drainage system gets disrupted. Removing nodes is like closing a few lanes on a major highway—it can cause a serious traffic jam.
When that lymph fluid can’t flow freely, it backs up into the surrounding tissues of your arm, hand, chest, or back, causing swelling. That chronic swelling is lymphedema. The good news is that while it’s a serious condition, it's manageable, and being proactive is your best strategy to prevent it.
Gentle Exercises to Get You Moving Again
Your surgeon or a physical therapist will be your best guide here, giving you a specific list of exercises that are safe for you. The whole point is to gradually reclaim your full range of motion without putting any stress on your incision.
Here are a few of the classics you'll likely be introduced to:
- Wall Climbs: Stand facing a wall, about an arm's length away. Gently "walk" the fingertips of your affected arm up the wall, going only as high as feels comfortable. Don't push into pain. Hold for a moment, then slowly walk your fingers back down.
- Pendulum Swings: Find a table or the back of a sturdy chair to lean on with your good arm. Let your affected arm hang down loose and relaxed. Gently swing it forward and back, then side to side, and finally in small, slow circles. The movement should come from your shoulder, like a pendulum.
- Shoulder Rolls: Whether you're sitting or standing, let your arms hang at your sides. Slowly roll your shoulders up toward your ears, then squeeze them back, and let them fall. Repeat a few times, then reverse the circle.
These should feel like a mild, pleasant stretch. If you feel any sharp pain, stop. It’s far better to do a few repetitions several times throughout the day than to try and do one long, tiring session.
Building Proactive Habits to Lower Your Risk
Beyond those specific exercises, a few simple daily habits can make a huge difference in lowering your lymphedema risk. It really boils down to protecting your affected arm from injury, infection, and unnecessary strain.
Essential Lymphedema Prevention Habits:
Taking these steps is a vital part of modern post-surgical care. It’s worth remembering how fortunate we are to have this level of guidance. Globally, outcomes after breast cancer surgery vary dramatically. In high-income countries like the U.S., where over 4 million breast cancer survivors live, the 5-year survival rate is often above 85%. That figure is tragically lower in places like sub-Saharan Africa, a stark reminder of how critical access to comprehensive care really is. You can learn more about these global disparities in breast cancer survival from the Global Surgery Foundation.
Your Guide to Scar Care and Reconstruction

The physical changes from breast cancer surgery are a huge part of your recovery. Learning to care for your scars and thinking about your body's new silhouette are deeply personal decisions, and it's so important to have clear, kind information to guide you. This part of the journey is all about helping you feel comfortable and whole in your own skin again.
Let's start with your surgical scars. In the beginning, your only job is to follow your surgeon's instructions to the letter, which usually means keeping the area clean and dry. Think of it like protecting a very delicate piece of fabric while it mends.
Once your team gives you the green light—usually around 3-4 weeks post-op—you can start playing a more active role. This is when your attention can really make a difference in how the scar heals, improving its flexibility and appearance over the long run.
Nurturing Your Scars as They Heal
Good scar care can make a world of difference, reducing tightness and helping to minimize the scar’s final look. The best approach combines gentle massage, good hydration, and smart protection to create the perfect environment for your skin to remodel itself.
Gentle scar massage is one of the most powerful tools you have. Using a simple, fragrance-free lotion or oil, use your fingertips to apply firm yet gentle pressure. Move the skin over the tissue underneath in small circles and lines. This simple action helps break down dense collagen, which is what makes scars feel tough, and encourages them to become softer and flatter.
Sun protection is also an absolute must. New scar tissue is incredibly vulnerable to UV rays and burns easily, which can cause it to darken permanently.
- Stay Covered: For the first year, try to keep your scar covered with clothing or a bandage when you’re out in the sun.
- Sunscreen is Your Friend: After the incision is fully healed, get into the habit of applying a broad-spectrum sunscreen of at least SPF 30 every day.
Your path to physical recovery is yours alone. Whether you opt for reconstruction, embrace a flat closure, or just need time to think it over, the best decision is always the one that honors your body, your comfort, and your sense of self.
Exploring Your Reconstruction Choices
For many women and men, breast reconstruction is a vital step in moving forward after surgery. It’s a very personal process with several different avenues, and the "right" choice is simply the one that fits your body, your life, and what you want for yourself. The conversation generally breaks down into two main types: implant-based and autologous (or "flap") reconstruction.
Implant-based reconstruction is a very common route. It's often a two-step procedure. First, a surgeon places a tissue expander under the skin and muscle, which is gradually filled to create a pocket. A second surgery then swaps the expander for a permanent saline or silicone implant.
Autologous reconstruction, on the other hand, uses your own body tissue to build a new breast. Surgeons can take skin, fat, and sometimes a small amount of muscle from another area—like your belly, back, or thighs—and reshape it. While it's a more involved surgery with a longer recovery, the results often look and feel more natural and won't require future implant maintenance.
Comparing Reconstruction Approaches at a Glance
It's also so important to know that aesthetic flat closure is a wonderful and empowering surgical choice. This isn't just "not having reconstruction"—it's a deliberate surgical procedure designed to create a smooth, clean chest wall. For many people, choosing to "go flat" is a powerful decision that helps them feel like themselves again without more surgeries.
Preparing for Your Next Steps in Treatment
Think of your breast cancer surgery as the critical first mission in a larger campaign for your long-term health. It was a targeted strike designed to remove the primary tumor—the cancer's main stronghold. But to ensure lasting peace, your oncology team often needs to follow up with specialized forces to patrol the area and eliminate any microscopic cancer cells that might be hiding out. These follow-up treatments are what we call adjuvant therapies.
This next phase is entirely guided by the information we gathered during your surgery. The tissue that was removed is sent to a lab for careful analysis, creating a detailed pathology report. This report is essentially a blueprint of the cancer, revealing its size, type, and specific characteristics, like its hormone receptor status. This information is precisely what your oncologist needs to design a treatment plan that’s built just for you.
Decoding Your Personalized Treatment Plan
The idea of more treatment right after surgery can feel daunting, I know. But understanding the why behind each recommendation can make the path forward feel much clearer and a lot less frightening. Each type of adjuvant therapy has a very specific job to do, working in different ways to lower the risk of the cancer ever coming back.
Your plan might include one or a combination of the following therapies, depending on what your pathology report tells us. It's a strategic approach aimed at giving you the best possible protection for the future.
Radiation Therapy: This is like a highly focused cleanup crew sent to the exact area where the surgery took place. It uses high-energy rays to destroy any rogue cancer cells that might have been left behind in the breast, chest wall, or nearby lymph nodes.
Chemotherapy: Think of chemotherapy as a systemic patrol that travels throughout your entire body via the bloodstream. Its mission is to seek and destroy any cancer cells that may have escaped the original tumor and started to travel elsewhere.
Hormone Therapy: This approach is only for hormone receptor-positive (HR+) breast cancers. If the cancer cells use estrogen or progesterone to grow, this therapy acts like a roadblock. It either lowers your body's hormone levels or blocks the hormones from reaching and fueling any lingering cancer cells.
Targeted Therapy: This is a more modern, precise form of treatment. It’s designed to identify and attack specific features on cancer cells, like a key fitting into a particular lock. A common example is for HER2-positive breast cancers, where drugs specifically target the HER2 protein that makes the cancer grow.
The goal of adjuvant therapy is not just to treat the cancer you had, but to proactively protect your future. It's an investment in your long-term wellness, designed to significantly reduce the chances of recurrence so you can move forward with confidence.
What to Expect From Adjuvant Therapies
Each of these treatments has its own timeline and comes with its own set of potential side effects. Your care team will, of course, walk you through every single detail, but here is a general overview to help you prepare for that conversation.
Radiation is typically a daily treatment (Monday through Friday) that lasts for several weeks. Chemotherapy is usually given in cycles—a treatment day followed by a period of rest and recovery. Hormone and targeted therapies are often longer-term treatments, sometimes taken as a daily pill for five, or even ten, years.
Knowing what’s coming allows you to plan your life around treatment, arrange for support from loved ones, and mentally prepare for the next step in your healing journey.
To make things a bit clearer, here's a simple table outlining the core purpose of each main therapy type.
Common Adjuvant Therapies After Breast Cancer Surgery
This roadmap of potential next steps after breast cancer surgery is meant to empower you with knowledge. Our goal is to turn the unknown into a manageable, well-defined plan, and we'll be with you every step of the way.
Nurturing Your Emotional Health and Finding Support
While so much of the focus is on your physical healing, the emotional journey you're on after breast cancer surgery is just as real and just as important. It’s completely normal to feel a tangle of emotions—relief, grief, anxiety, gratitude—sometimes all in the same day. This experience is life-altering, and giving yourself space to process it all is a huge part of your recovery.
Many women and men grapple with changes to their body image or a new sense of vulnerability. It's helpful to think of your emotional health like a garden that needs tending. It won't bloom overnight. It needs patience, gentle care, and the right kind of support to thrive again.
Practical Tools for Emotional Wellness
You don't have to make grand gestures to care for your mental health. Often, it's the small, consistent actions that build a foundation of calm and stability, giving you moments of peace to process everything on your own terms.
Here are a few gentle places to start:
- Journaling: You don't need to be a great writer. Just scribbling down a few thoughts or feelings each day can be a powerful release and help you make sense of your emotional landscape.
- Mindful Moments: Take just 60 seconds to focus on your breath. Feel it come in, feel it go out. This simple exercise can be a powerful anchor, pulling you out of a spiral of anxious thoughts and back into the present moment.
- Gentle Movement: Once your doctor gives you the green light, a slow walk, some simple stretches, or even just sitting in the fresh air can do wonders for reconnecting your mind and body and lifting your spirits.
Your emotional recovery doesn't have a deadline. Be kind and patient with yourself. Simply acknowledging your feelings without judgment is one of the most powerful forms of self-care you can practice.
Building Your Circle of Support
You don’t have to walk this path alone. In fact, you shouldn’t. Leaning on your support system is a sign of strength, and it's okay to ask for what you need—whether that's a home-cooked meal, a listening ear, or just some quiet company.
Sometimes, our loved ones want to help but just don't know how. For friends and family looking for ways to be there for you, our guide on how to support someone with cancer can be a great starting point.
It can also be incredibly validating to connect with people who just get it.
- Professional Counselors: A therapist who specializes in oncology can offer you concrete coping strategies in a safe, confidential space.
- Peer Support Groups: There's a unique comfort in sharing your story with other breast cancer survivors. This shared understanding can make you feel far less isolated on your journey.
Your hospital’s patient navigator or social worker is a fantastic resource for connecting you with local groups and therapists. Building this network is just as crucial as any other part of your healing.
Common Questions About Breast Cancer Recovery

Once you're home and settling into your recovery, the big-picture plans fade away and the small, practical questions start to surface. That's completely normal. Having straightforward answers to these everyday concerns can make a world of difference, helping you feel less anxious and more in command of your own healing.
Think of this as your go-to guide for those "what do I do now?" moments. Knowing the general timeline for simple things like showering or driving helps you set realistic expectations for the coming weeks.
When Can I Shower After My Breast Cancer Surgery?
This is almost always one of the very first questions we hear. The answer really hinges on your specific surgery and whether you have drains. Most surgeons will give you the green light to shower 24 to 48 hours after your procedure, but they'll give you very specific instructions on how to keep your incision area protected and dry.
If you have surgical drains in place, you’ll likely be on sponge-bath duty until they come out. To keep your recovery on track and avoid any risk of infection, it's crucial to follow your surgical team's advice to the letter.
How Long Will the Surgical Drains Stay In?
Surgical drains are a temporary, but very important, part of your initial recovery. Their job is to prevent fluid from building up around the surgical site. They’re usually taken out once the fluid they collect drops to a consistently low level—the magic number is typically less than 30ml over a 24-hour period.
For most people, this happens within one to three weeks after the operation. Your team will ask you to track the fluid output in a log, and they’ll use that information to decide when it's the right time to remove the drains during a follow-up visit.
What Warning Signs Should I Watch For?
Knowing when to pick up the phone and call your doctor is a key part of a safe recovery. It's helpful to think of these as red flags that need prompt attention from your medical team.
Don't hesitate to contact your care team if you experience any of the following: a fever over 101°F (38.3°C), new or worsening redness or warmth around the incision, any foul-smelling drainage, pain that isn't managed by your prescribed medication, or sudden, unusual swelling in your arm or hand on the side of your surgery. These could be signs of an infection or another complication that needs to be addressed.
When Is It Safe to Drive Again?
Getting back behind the wheel is a big step toward independence, but it can't be rushed. You should not drive until you are completely off all narcotic pain medications and have regained your full, comfortable range of motion in your arm and shoulder. You have to be able to turn the wheel or brake suddenly without pain or hesitation.
This timeline is often between two to four weeks, but this is a non-negotiable rule: you must get clearance from your surgeon first before you start driving again.
At Hirschfeld Oncology, we know that your recovery journey continues long after you leave the operating room. If you have questions about what comes next or are looking at treatment options here in the NYC area, our dedicated team is here to offer guidance and support. To learn more from our experts and patient community, please visit our blog at https://honcology.com/blog.





.png)


.png)
.png)




