When you first hear the words "bile duct cancer," it can feel like everything stops. But the first step in moving forward is getting a clear picture of what the diagnosis really means. Two words you'll hear a lot are stage and prognosis. These aren't just medical jargon; they're the coordinates that help map out your treatment journey.
Understanding these concepts is key. It empowers you to participate in conversations with your oncology team, ask the right questions, and feel more in control of the path ahead.
Navigating Your Bile Duct Cancer Diagnosis
A cancer diagnosis comes with a flood of new information. Let's break down two of the most important pieces: staging and prognosis.
Think of the stage as a detailed map showing your doctors exactly where the cancer is and how far it has spread from where it started. This map is absolutely essential for plotting the most effective treatment course. Prognosis, on the other hand, is the medical team's best forecast of the likely outcome of the disease. It’s based on data from thousands of other patients, but it’s an estimate—not a script for your personal story.
What Is Cancer Staging?
Staging creates a common language for doctors to describe the cancer's extent. For bile duct cancer, it's generally broken down into three main categories based on how far the cancer has traveled:
- Localized: The cancer is contained only in the bile duct where it began.
- Regional: The cancer has grown into nearby tissues or lymph nodes.
- Distant (Metastatic): The cancer has spread to faraway parts of the body, like the lungs or bones.
Pinpointing the stage is the foundation of your treatment plan. A localized cancer might be a candidate for surgery, whereas a distant cancer will likely need treatments that can travel throughout the body, like chemotherapy.
Understanding Prognosis and Survival Rates
Prognosis is often explained using 5-year relative survival rates. This statistic simply compares people with the same type and stage of cancer to people in the general population. It shows the percentage of patients who are still alive five years after their diagnosis.
It's so important to see these numbers for what they are: historical averages. They don't predict your individual outcome or account for your unique health, the very latest treatments, or your personal response to therapy. Your journey is your own.
Bile duct cancer survival rates show just how critical early detection is. We've compiled the data into a simple table to illustrate this.
Bile Duct Cancer Stages and 5-Year Survival Rates
This table summarizes the different stages of bile duct cancer and the corresponding 5-year relative survival rates, illustrating the importance of early diagnosis.
As you can see, the survival rate is significantly higher when the cancer is found before it has a chance to spread. This underscores why catching it early makes such a difference.
This bar chart provides a clear visual of just how much the stage at diagnosis impacts the outlook.
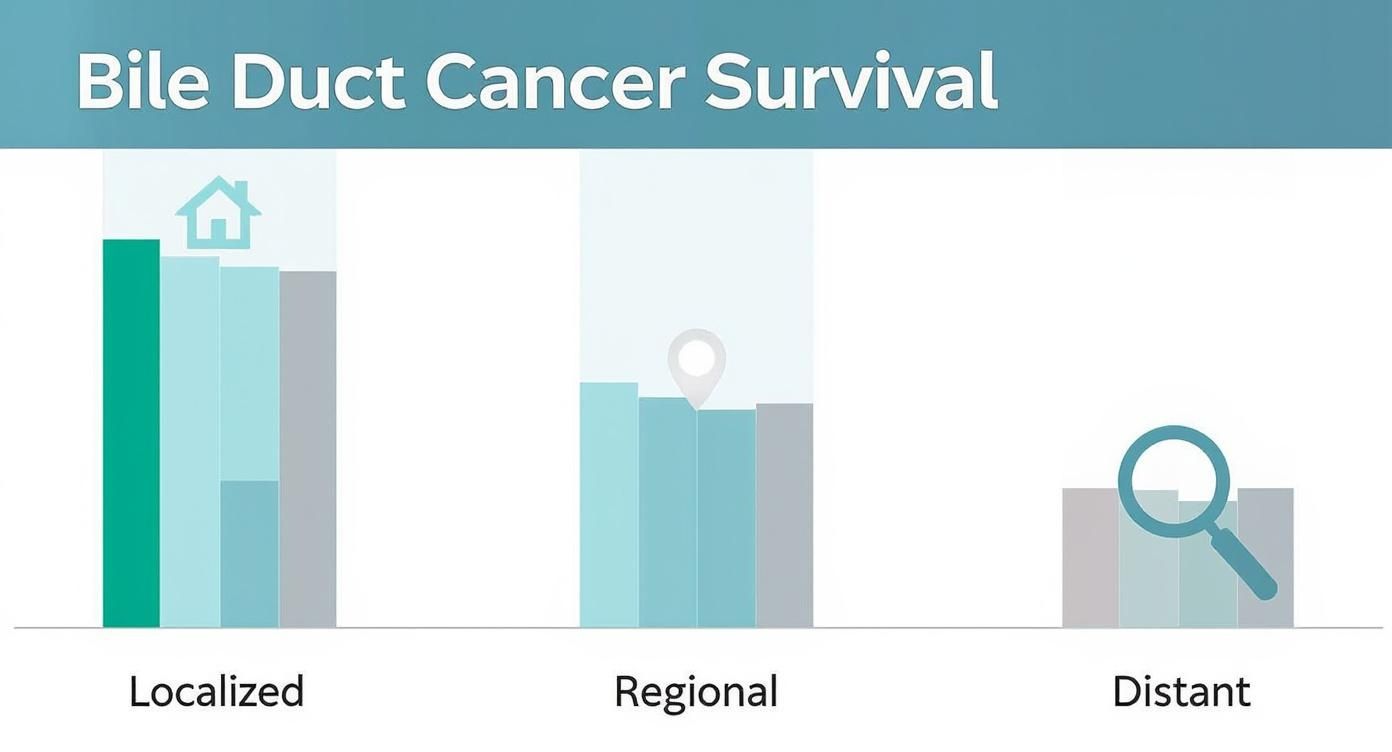
The chart drives home a crucial point: the earlier the cancer is found and treated, the better the chances for a positive outcome. To learn more, you can get a deeper understanding of bile duct cancer and its complexities on our main resource page.
The Core Strategies for Treating Bile Duct Cancer
When we develop a battle plan against bile duct cancer, we rely on three foundational pillars: surgery, chemotherapy, and radiation therapy. These aren't just separate options; they are powerful tools that form the backbone of most treatment plans. Often, we use them in combination to give our patients the best possible chance of success.
I often explain it to my patients with a gardening analogy. Imagine the cancer is a stubborn weed. Surgery is like digging the entire weed out by the roots—the most direct way to get rid of it. Chemotherapy is like a systemic treatment you put in the soil, designed to kill off any stray seeds that may have already spread. And radiation? That's like a highly focused spray, zeroing in on a specific patch to eliminate any last traces.
Understanding how these three approaches work—both on their own and together—is the first and most important step in making sense of your personalized treatment plan.
Surgery: The Primary Path to a Cure
When we catch bile duct cancer in its early, localized stages, surgery is almost always our go-to. It offers the best shot at a cure, and the goal is straightforward: remove the entire tumor, along with a small, clean margin of healthy tissue around it. This is how we ensure no cancer cells are left behind.
Unfortunately, because this cancer (also known as cholangiocarcinoma) is often diagnosed late, surgery isn't always on the table. In reality, only about 20–30% of patients are eligible for this kind of curative surgery at the time of their diagnosis. Even after a successful operation, the risk of recurrence can be high. These tough statistics underscore just how critical early detection is and why we're constantly pushing for better diagnostic tools. You can read more about the challenges of bile duct cancer on oncodaily.com.
The type of surgery we recommend depends entirely on where the tumor is and how big it's grown.
- Bile Duct Resection: If the tumor is small and contained right in the bile duct, a surgeon can often remove just that affected section.
- Partial Hepatectomy: For tumors that have started to grow into the liver, a portion of the liver has to come out as well.
- Whipple Procedure: This is a much more complex operation for tumors near the pancreas. It involves removing the head of the pancreas, the gallbladder, and parts of the small intestine.
In a few, very specific cases, a liver transplant might be considered for patients with early-stage tumors that can't be removed through other surgical means.
Chemotherapy: A Systemic Approach
While surgery is a local fix, chemotherapy works systemically. Powerful cancer-fighting drugs travel through the bloodstream to reach and destroy cancer cells no matter where they are in the body. This makes it a vital tool, especially when the cancer has already spread or when we're worried about it coming back.
We can use chemotherapy in a few different ways:
- Adjuvant Therapy: This is chemo given after surgery. The goal is to hunt down and kill any microscopic cancer cells that might have been left behind.
- Neoadjuvant Therapy: Sometimes, we give chemo before surgery to shrink a tumor, which can make the operation safer and more effective.
- Primary Treatment: When the cancer has spread and can't be removed with surgery, chemotherapy becomes the main treatment.
For a long time, the standard chemotherapy combination for bile duct cancer has been gemcitabine and cisplatin. This pairing has a solid track record, but we are always exploring newer, more effective combinations. Of course, these powerful drugs come with side effects, which is why close monitoring and proactive management are a huge part of the process.
Radiation Therapy: A Focused Attack
Radiation therapy uses high-energy beams, like X-rays, to precisely target and kill cancer cells. It’s a very localized treatment. We can focus the beams directly on the tumor and the immediate area around it, which helps minimize damage to nearby healthy tissue.
Radiation works by scrambling the DNA inside cancer cells. This damage stops them from being able to divide and grow. Over the course of treatment, these damaged cells die off and the body naturally clears them away.
We often combine radiation with chemotherapy—a strategy called chemoradiation—because the chemo can make the cancer cells more sensitive to the radiation's effects. While surgery and chemo are central to many plans, it is important to know about other options as well. You can learn more about how targeted therapy works in our detailed guide on the subject.
The Next Wave of Cancer Therapies
Beyond the foundational treatments of surgery, chemo, and radiation, a much more personalized era of medicine is opening new doors for patients with bile duct cancer. This means we now have powerful options that fight the disease in entirely new ways. Two of the most important advances are targeted therapy and immunotherapy.
These approaches are a world away from the broad-stroke methods of traditional chemotherapy. Instead of a sledgehammer, think of them as a scalpel, designed to work with the unique biology of your specific cancer or even your own immune system to fight the disease on a molecular level.
Targeted Therapy: A Precision Approach
Think of traditional chemotherapy as a general weed killer—it gets the job done, but it often damages the healthy flowers and grass around the weeds. Targeted therapy is completely different. It’s like a specialized treatment engineered to attack only the weeds by exploiting something unique about their biology. This is the core idea behind this advanced form of bile duct cancer treatment.
These are "smart" drugs that hone in on specific genetic mutations or proteins that are literally driving the cancer cells to grow and divide. For bile duct cancer, a few specific mutations are especially important:
- FGFR2 Fusions: The FGFR2 gene is like a switch that controls cell growth. In some bile duct cancers, this switch gets fused with another gene and becomes stuck in the "on" position, causing endless growth. Targeted drugs can block this signal, effectively flipping the switch off.
- IDH1 Mutations: The IDH1 gene is involved in a cell's metabolism. When it mutates, it starts producing a substance that fuels cancer growth. Targeted inhibitors can step in and shut down this abnormal production line.
So, how do we know if you're a candidate? Your oncologist will run genomic tests on a sample of your tumor tissue. This molecular profiling acts as a roadmap, giving us the exact information needed to match you with the right targeted drug.
These therapies show just how far we've come. We're no longer treating all bile duct cancers as one disease. Instead, we're identifying the specific drivers in each patient's tumor and choosing a drug designed to shut them down.
The FDA’s approval of drugs like infigratinib in 2021 for advanced cholangiocarcinoma was a massive step forward in personalized care. Still, not everyone has equal access to these treatments; as you can discover more about these global health challenges on pmc.ncbi.nlm.nih.gov, disparities persist, especially in lower-income countries where the disease is more common.
Immunotherapy: Unleashing Your Own Immune System
While targeted therapy focuses on the cancer cell's internal wiring, immunotherapy takes a different route altogether. It doesn't attack the cancer directly. Instead, it essentially rips off the "invisibility cloak" that cancer cells use to hide from your body's immune system. It unleashes your natural defenses to do the job they were built for.
Your immune system has natural brakes, called checkpoints, that keep it from going haywire and attacking healthy cells. Cancer cells are devious—they’ve learned how to exploit these checkpoints to trick immune cells into leaving them alone.
This is where checkpoint inhibitors come into play. These drugs block the "don't attack me" signal that cancer cells send to your immune cells. By doing this, they take the brakes off your immune system. This frees up your T-cells—the soldiers of your immune system—to finally recognize and destroy the cancer cells they were previously ignoring. You can learn more about how immunotherapy works at Hirschfeld Oncology.
Both targeted therapy and immunotherapy represent a fundamental shift in how we approach advanced bile duct cancer treatment. By moving beyond one-size-fits-all strategies, we can offer more precise, effective, and often less toxic options, creating new avenues of hope for patients.
Expanding Your Treatment and Support Options

While surgery, chemotherapy, and radiation are the cornerstones of care, a truly comprehensive bile duct cancer treatment plan often means looking at the bigger picture. Two of the most powerful—and most misunderstood—options are clinical trials and palliative care. Getting these right is key to creating a plan that fights the cancer while supporting you as a whole person.
Many people hear "clinical trial" and think it's a last-ditch effort. In reality, it’s a direct line to the next wave of advanced therapies. Likewise, "palliative care" is too often confused with hospice, when its real job is to improve your quality of life from day one, at any stage of the illness. Let's break down what these options really mean.
Clinical Trials: Access to Tomorrow's Treatments Today
Clinical trials are simply research studies designed to test new treatments and strategies before they become available to everyone. When you participate, you get access to therapies that are often years ahead of the current standard of care—all while helping move cancer research forward for others.
It’s the engine of medical progress. Every single treatment we have today, from basic chemotherapy to advanced immunotherapy, exists because of a clinical trial. For a less common cancer like cholangiocarcinoma, these studies are especially vital for finding new and better ways to fight the disease.
Participating in a clinical trial is a deeply personal decision made with your oncology team. It offers access to new drugs and approaches, but it’s vital to weigh the potential benefits against the risks and unknowns of any new therapy.
These trials are constantly exploring new territory, pushing the boundaries of what's possible.
- New Targeted Therapies: As we uncover more specific genetic drivers in bile duct cancer, like HER2 mutations, new drugs are always in development to attack those exact targets.
- Novel Immunotherapy Combinations: Researchers are constantly testing new pairings, like combining checkpoint inhibitors with other drugs to wake up the immune system more effectively.
- Innovative Drug Delivery: Some trials focus on finding smarter ways to get chemotherapy or radiation right to the tumor, maximizing their power while sparing healthy tissue.
Palliative Care: Supporting Your Quality of Life
Let's clear up one of the biggest myths in cancer care: palliative care is not hospice. Palliative care is a specialized field focused entirely on managing the symptoms, pain, and stress that come with a serious illness. It can—and should—be started at any point after diagnosis, right alongside your primary cancer treatments.
The goal is simple: improve your quality of life. A dedicated team of specialists works hand-in-hand with your oncologist to tackle the physical and emotional burdens of a bile duct cancer treatment plan.
This support is tailored completely to you and what you’re going through.
- Symptom Management: These experts are masters at controlling treatment side effects like nausea, fatigue, and pain, making your day-to-day life more manageable.
- Emotional and Spiritual Support: They provide counseling and resources for both you and your family to navigate the anxiety and stress of a cancer diagnosis.
- Clear Communication: They can act as a bridge, helping you understand complex medical information and make treatment decisions that truly reflect your personal values and goals.
Bringing palliative care into your plan early on consistently leads to better symptom control and an improved sense of well-being. Think of it as an essential layer of support, designed to help you feel as good as you can, for as long as you can, while you fight the disease.
Finding Your Treatment Partner in NYC
Figuring out the world of bile duct cancer treatments is one thing. Finding the right team in New York City to turn that information into a plan that works for you is a whole other challenge. When you're facing a serious diagnosis, the last thing you want is to feel like just another patient in a massive system. The goal is to find a practice where you're seen as a person and treated as a partner in your own care.
That partnership is exactly what we build at Hirschfeld Oncology. We specialize in taking the complex science of oncology and creating a practical, personalized treatment regimen. It’s a plan that considers your tumor's specific genetics, your overall health, and just as importantly, what you want your life to look like during and after treatment. This is where knowledge becomes a real strategy.
How We Build Your Personalized Plan
Your first step with us is a real conversation. We sit down for a detailed consultation where our main job is to listen—to your questions, your fears, and what you hope to achieve. We firmly believe that the most effective bile duct cancer treatment plans are built on a foundation of trust and shared understanding. Every decision we make together has to feel right for you.
Our process is straightforward and collaborative right from the start.
- Getting the Full Picture: We begin by carefully reviewing your entire medical history, all your scans, and any treatments you've had before. This deep dive ensures we don't miss a single detail.
- Unlocking Your Tumor's Blueprint: We use advanced genomic testing to get to know the cancer on a molecular level. This analysis can pinpoint the specific mutations driving its growth, opening the door for highly specific targeted therapies or immunotherapy.
- Designing Your Strategy, Together: With all the information in hand, we map out your treatment plan. We’ll walk you through the "why" behind every recommendation, discussing the potential benefits and side effects so you feel completely informed and in control.
- Managing Your Well-being: Our job doesn't stop once treatment begins. We are proactive and aggressive when it comes to managing side effects, helping you stay as strong and comfortable as possible throughout the process.
The most powerful tool in oncology isn't a single drug; it's a personalized strategy. It's about combining the right therapies, at the right time, for the right person—always with the dual goals of extending life and protecting its quality.
Care and Comfort at Our Infusion Center
Going through treatment is tough enough without it being in a cold, clinical setting. Our modern infusion center right here in NYC was designed to be a calm, quiet, and supportive space. Whether you're coming in for chemotherapy, targeted therapy, or immunotherapy, you can expect expert, attentive care in a peaceful environment. Our experienced oncology nurses are there to ensure you're safe and comfortable every step of the way.
We know that navigating advanced cancer takes more than just medicine. It takes a team that sees you as a whole person, not just a diagnosis. From the first time you call us to your regular infusion appointments, our focus remains on providing compassionate care that supports you both physically and emotionally. At Hirschfeld Oncology, we're here to be your dedicated ally, helping you face every part of this journey with clarity and confidence.
Common Questions About Treatment

When you're navigating a new diagnosis, the medical information can feel overwhelming. But alongside the big clinical questions, a lot of practical, day-to-day concerns pop up. Getting clear, straightforward answers to these questions can bring a real sense of peace and help you feel more in control.
This is where we tackle some of the most common things patients and their families ask. Think of this as filling in the gaps—empowering you with the knowledge to be an active partner in your own care.
What Are the Common Side Effects of Treatment?
Let's be direct: every effective bile duct cancer treatment has potential side effects. The key thing to remember, though, is that they are almost always manageable. Your oncology team is trained to stay ahead of them, working to prevent and treat issues so you can stay as comfortable as possible.
The side effects you might run into depend entirely on the kind of therapy you’re getting. Each one works on the body in a different way.
- Chemotherapy: Since chemo travels through your bloodstream, it can affect healthy cells that divide quickly, not just cancer cells. This is why you might experience fatigue, nausea, a dip in appetite, or a higher risk of getting sick.
- Radiation Therapy: This is a much more localized treatment, so side effects usually stick to the area being targeted. You might see some skin irritation (like a sunburn), feel tired, or have some nausea if the radiation is aimed at your abdomen.
- Targeted Therapy and Immunotherapy: These modern treatments come with their own set of potential issues. Targeted drugs can sometimes cause things like skin rashes, diarrhea, or high blood pressure. Immunotherapy can occasionally rev up the immune system a bit too much, leading to inflammation in different parts of the body.
Modern oncology is just as focused on supportive care as it is on fighting cancer. We have fantastic medications to handle nausea, proven strategies to push back against fatigue, and therapies to soothe skin reactions. The most important thing is to speak up. Never hesitate to tell your team about a new or worsening symptom.
How Is the Right Treatment Plan Chosen for Me?
There’s no "one-size-fits-all" recipe for treating bile duct cancer. Your treatment plan is a highly personalized strategy, carefully crafted by your oncology team after looking at a whole host of factors unique to you.
It's like assembling a custom toolkit for a very specific job. For one person, surgery might be the main tool. For another, it might be a precise combination of targeted therapy and chemotherapy.
The core principle of modern cancer care is personalization. Your treatment plan isn't just based on the name of your cancer, but on its specific molecular blueprint, its stage, and your personal health and life goals.
So, what goes into this decision-making process? Several key pieces of information:
- Cancer Stage and Location: Is the tumor contained and removable with surgery? Or has it spread, meaning we need a treatment that can travel throughout the body?
- Tumor Genetics: We can run molecular tests on the tumor to look for specific genetic markers, like FGFR2 or IDH1. Finding one of these can open the door to highly specific targeted drugs.
- Your Overall Health: Your general fitness level, age, and any other medical conditions you have play a big role in determining which treatments your body can handle.
- Your Personal Priorities: Your goals are at the center of the conversation. We need to know what matters most to you—whether it's maintaining a certain quality of life, being able to keep working, or going after the most aggressive options available.
This whole process is a collaboration, ensuring the final plan is a perfect match for both the medical science and your individual life.
Can Diet or Lifestyle Changes Make a Difference?
While diet and lifestyle changes can't cure cancer on their own, they absolutely play a powerful supportive role during your treatment. Taking care of your overall well-being can make a huge difference in how well you tolerate therapies and, just as importantly, how you feel day-to-day.
You don't need to overhaul your entire life. Simple, consistent habits can have a real impact.
Here are a few practical areas to focus on:
- Nutrition: Try to eat a balanced diet with plenty of protein to help your body heal and repair itself. If your appetite isn't great, think smaller, more frequent meals. And don't forget to stay hydrated.
- Physical Activity: Even gentle movement, like a short walk, can do wonders for fighting fatigue, boosting your mood, and maintaining muscle. The golden rule is to listen to your body and check with your doctor first.
- Stress Management: A cancer diagnosis is tough, emotionally and mentally. Finding what works for you—whether it's mindfulness, deep breathing exercises, or light meditation—can help keep anxiety in check.
These aren't replacements for medical treatment, but they are ways you can take an active, empowering role in your own care.
What Is the Difference Between Palliative Care and Hospice?
This is one of the biggest points of confusion, and it’s so important to get it right. Palliative care and hospice are not the same thing. One is a layer of support you can have from day one, while the other is specifically for the end of life.
Palliative care is not hospice. Think of palliative care as a specialty focused on one thing: improving your quality of life. The team helps manage symptoms, pain, and the stress that comes with a serious illness. It's provided right alongside curative treatments like chemo or radiation, at any stage of the disease.
Hospice care, on the other hand, begins only when a person is no longer seeking treatments to cure their cancer and is nearing the end of their life. The entire focus shifts to providing comfort and peace.
Bringing a palliative care team on board early in your bile duct cancer treatment can lead to better symptom control and an overall better experience on your journey.
At Hirschfeld Oncology, we believe that the best care combines advanced medical science with compassionate, personalized support. We're here to answer all your questions and build a treatment plan that fits you. To learn more about our approach, feel free to read more on our blog.





.png)


.png)
.png)




