Yes, chemotherapy can absolutely increase the risk of developing blood clots. It's a known and very manageable side effect of treatment, and it's something your oncology team is always on the lookout for. Knowing why it happens is the first step in taking an active role in your own care.
The Link Between Chemotherapy and Blood Clots
Before we even talk about chemotherapy, it's important to understand that cancer itself can make your blood more likely to clot. Think of your bloodstream as a smoothly flowing river. The cancer can release substances that essentially make the water a bit "stickier," slowing things down.
Now, add chemotherapy to the mix. The drugs, which are powerful enough to kill cancer cells, can also irritate the "riverbanks"—the delicate inner lining of your blood vessels. This irritation can create rough patches.
So, you have this combination of stickier, slower-moving blood and rough vessel walls. It’s the perfect setup for a logjam to form, which is exactly what a blood clot is.
A Two-Part Risk Factor
This double-whammy—from the cancer and the treatment—is why blood clots are such a big focus in oncology. The medical term for them is venous thromboembolism (VTE), and it's a statistically significant risk that we actively manage.
Just how big is the risk? Studies show that chemotherapy can push the yearly rate of VTE in cancer patients to between 11% and 20%, with the exact number depending on the type of cancer and the specific chemo drugs used. This is why your care team is so vigilant about monitoring and prevention. You can read more about the specifics of VTE risk in cancer patients.
"Understanding that both cancer and chemotherapy can alter the body's clotting system is crucial. It’s a combined effect where the underlying disease primes the system, and the treatment can act as a trigger."
At Hirschfeld Oncology, our goal is to give you this information without causing alarm. This is a known challenge in cancer care, and we have well-established ways to handle it.
The following table breaks down the main points for a quick overview.
Quick Facts About Chemotherapy and Blood Clot Risk
Knowing these connections is the foundation for a strong partnership between you and your healthcare team. It allows us to anticipate potential issues and manage them effectively, keeping your treatment on track while making your safety the top priority.
How Does Chemotherapy Increase Your Clotting Risk?
It's one thing to hear that chemotherapy can raise your risk of blood clots, but understanding why this happens can help you be a more proactive participant in your own care. This isn't just a random side effect; it's a direct result of how these powerful medicines interact with your body.
Think of your circulatory system as a finely tuned machine. Your body is constantly performing a delicate balancing act, making sure your blood clots when you have an injury but flows freely the rest of the time. Chemotherapy can throw that system off balance, pushing it towards clotting. Let's break down how.
Damage to Blood Vessel Linings
One of the most straightforward ways chemo can cause trouble is by damaging the blood vessels themselves. The inside of your veins and arteries is lined with a super-smooth layer called the endothelium. It's like nature's Teflon, designed to let blood cells slip by without a snag.
But some chemotherapy drugs are harsh. They can cause inflammation and create tiny, rough patches on this smooth lining. These damaged spots are like Velcro, giving platelets and other clotting factors a place to grab onto and start building a clot. This is a big reason why we keep a close eye on the areas around IV lines and ports.
Activating the Body's Clotting System
Chemotherapy also sends a powerful signal to your body to kick its clotting system into high gear. As the treatment destroys cancer cells, those dying cells release substances into your bloodstream. These substances act like an alarm, triggering your body's coagulation cascade—the complex chain of events that forms a clot.
Essentially, the treatment flips a switch that puts your clotting system on high alert. Your blood becomes "primed" and ready to clot much more easily than usual. The very system meant to protect you from bleeding can become overactive, creating clots when and where they aren't needed.
This overactivation is a core reason why the answer to "can chemo cause blood clots?" is a resounding yes. The treatment doesn't just create a passive risk; it can actively provoke the body's clotting mechanisms.
On top of that, certain chemo drugs can directly boost the production of proteins that encourage clotting while simultaneously reducing the levels of your body’s natural blood thinners. This double-whammy further tilts the scales toward a pro-clotting state.
The Role of Medical Devices
Beyond the drug's biological effects, the physical tools we use to deliver treatment also play a part. Devices like central venous catheters, PICC lines, and ports are incredibly important for giving chemotherapy safely, but they are still foreign objects placed inside a blood vessel.
A catheter can increase clot risk in a couple of ways:
- Physical Obstruction: The device can slightly change the way blood flows through the vein. This can create little pockets of turbulence or slow-moving blood where clots are more likely to form.
- Irritation Site: The tip of the catheter can rub against and irritate the vein's inner wall, creating an inflamed spot that's a perfect anchor for a clot to develop.
This is exactly why your team at Hirschfeld Oncology is so meticulous about the care and maintenance of your IV access. We're constantly monitoring for any signs of irritation to minimize this risk. By understanding all these factors—from the cellular level to the physical devices we use—we can better anticipate and manage your clotting risk throughout your treatment.
Which Cancers and Chemo Drugs Carry the Highest Clot Risk?
While chemotherapy raises the possibility of blood clots for any patient, the risk isn't a one-size-fits-all problem. It’s more like a weather forecast—while the whole city might be expecting rain, certain neighborhoods are under a severe thunderstorm watch. In the same way, some cancers and specific chemotherapy drugs come with a much higher statistical chance of causing a clot.
Pinpointing these factors helps us move from a general “what if” to a focused conversation about your personal care plan. Knowing if your cancer or treatment puts you in a higher-risk group is crucial because it allows your oncology team to be extra vigilant and proactive.
Cancers with a Higher Tendency to Clot
Some cancers are just naturally more "pro-thrombotic." This means their biology makes them more likely to create a super-charged clotting environment in the body. The tumors themselves often release a flood of pro-clotting substances directly into the bloodstream.
Cancers that are especially notorious for increasing the risk of venous thromboembolism (VTE) include:
- Pancreatic Cancer: This one is often at the top of the list. The aggressive nature of these tumors frequently causes a major spike in clotting factors. For a deeper dive, you can read our guide to pancreatic cancer treatment options.
- Stomach (Gastric) Cancer: Much like pancreatic cancer, tumors in the stomach can dramatically throw off the body's natural clotting balance.
- Lung Cancer: Certain types, like adenocarcinoma, are known to have a stronger link to VTE.
- Advanced-Stage Cancers: A crucial point—once a cancer has metastasized (spread), the risk of clotting goes up significantly, no matter where the tumor started.
It's also worth noting that for some cancers, like clear cell ovarian cancer, a blood clot—a large pelvic mass or a deep vein thrombosis (DVT)—can actually be one of the very first signs of the disease.
Chemotherapy Drugs That Increase Risk
Just as some cancers are bigger culprits, certain chemo agents are more directly linked to blood clot formation. These drugs can pour fuel on the fire, amplifying the risk that the cancer itself already created. They do this by directly affecting your blood vessels and clotting mechanisms.
This isn't just a theory; it's a measurable reality. A key 2015 study showed how treatment and genetics team up to elevate risk. In breast cancer patients on chemo who also had a high genetic susceptibility, the one-year VTE rate was 9.5%. That’s a huge jump from the 1.3% rate seen in patients with a low genetic risk who didn't get chemo. You can learn more about the findings on chemotherapy-associated blood clots.
This data really drives home the point that your personal risk is a combination of your diagnosis, your genetics, and your specific treatment plan.
Identifying High-Risk Drug Classes
Some of the most common chemotherapy drugs and categories known to raise clot risk include:
- Platinum-Based Drugs: This group includes workhorse drugs like cisplatin and carboplatin. They are incredibly effective against many cancers but have a known side effect of causing endothelial damage—basically, irritating the lining of blood vessels and creating a perfect spot for a clot to take hold.
- Angiogenesis Inhibitors: Drugs like bevacizumab (Avastin) work by starving tumors of their blood supply. But that same mechanism can sometimes disrupt the delicate balance of normal blood vessel health, making clots more likely.
- Immunomodulatory Drugs (IMiDs): Agents like thalidomide and lenalidomide are often used for multiple myeloma. They are very strongly linked to an increased risk of DVT and pulmonary embolism, especially when given alongside steroids like dexamethasone.
- Certain Targeted Therapies: Even though they aren't traditional chemo, some newer targeted therapies can also interfere with the body's clotting pathways.
At Hirschfeld Oncology, we weigh all these variables when designing your treatment. Knowing if you have a high-risk cancer or are getting a high-risk drug helps us build in the right monitoring and preventive strategies, making sure we stay one step ahead of any potential complications.
Recognizing the Warning Signs of a Blood Clot
When you're going through cancer treatment, one of the most powerful things you can do is learn to listen to your body. Since we know chemotherapy can increase the risk of blood clots, being able to spot the earliest signs means you can get medical help right when you need it.
Clots can show up in different places, but the two we worry about most are Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE).
Think of a DVT as a roadblock in a deep vein, usually in your leg or arm. A PE is what happens if a piece of that clot breaks off, travels to your lungs, and gets stuck, blocking a critical artery. This is a much more serious situation. Knowing how the symptoms differ is crucial for knowing what to do next.
The flowchart below can help you and your care team assess the specific risk factors that might lead to a clot during your treatment.
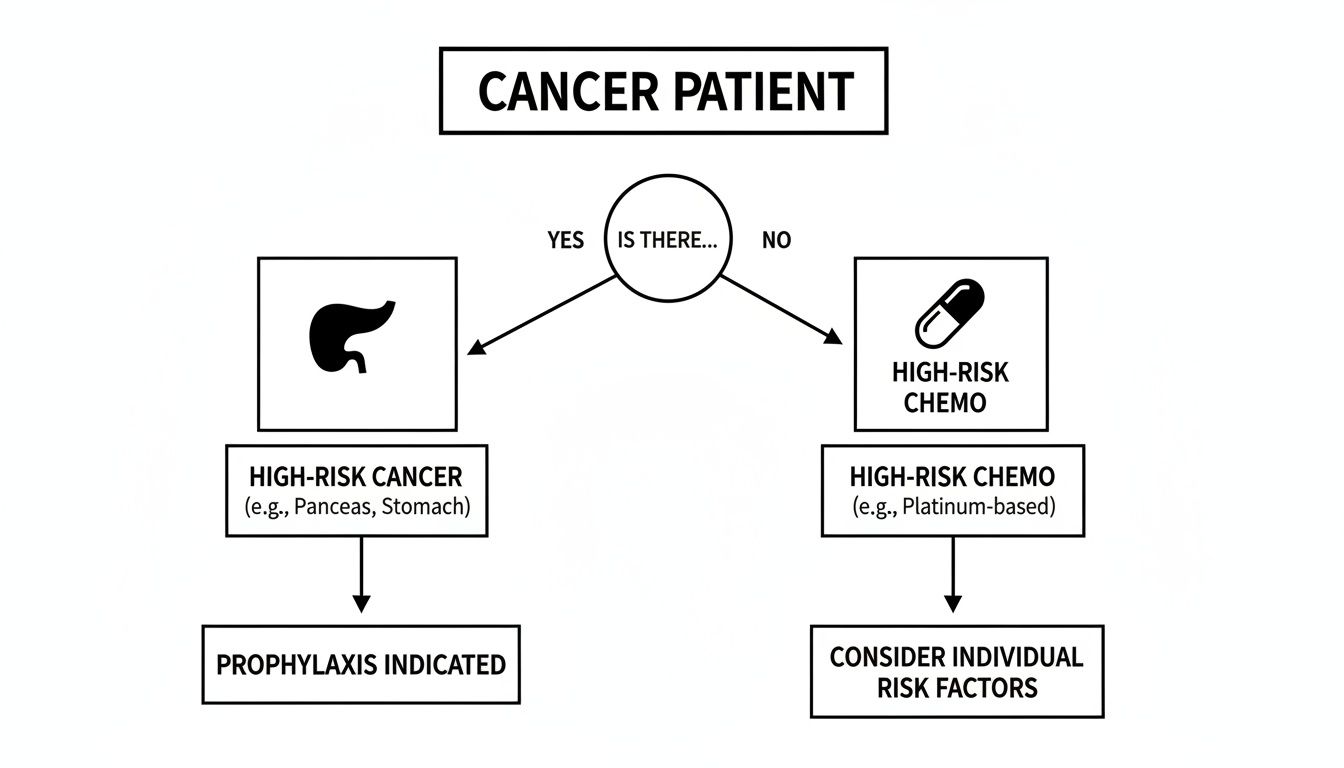
This kind of risk assessment helps us be proactive, highlighting when certain cancers or chemotherapy drugs require closer monitoring.
Symptoms of Deep Vein Thrombosis (DVT)
The signs of a DVT are almost always one-sided—you’ll notice them in just one arm or one leg, not both. If any of these symptoms appear, especially if they come on suddenly, it’s time to get in touch with your oncology team.
- Swelling: One limb suddenly looks puffier or bigger than the other.
- Pain or Tenderness: It often feels like a stubborn, deep cramp—like a charley horse that just won't quit.
- Warmth: The skin over that swollen, painful area might feel unusually warm.
- Redness or Discoloration: You may notice red streaks or a change in the skin’s color.
If you spot these signs, call your oncologist's office immediately. They need to be in the loop to decide the next steps, which usually involves getting you checked out for a clot. For more on handling these kinds of issues, check out our guide on effective symptom management during cancer therapy.
Symptoms of a Pulmonary Embolism (PE)
A pulmonary embolism is a true medical emergency. The symptoms hit fast and hard, signaling a dangerous blockage in your lungs.
A PE can be life-threatening, and every second matters. Never write these symptoms off as just a side effect of chemo. Get them checked out immediately.
If you experience any of the following, call 911 or get to the nearest emergency room right away:
- Sudden Shortness of Breath: You're struggling to breathe, and it has nothing to do with activity.
- Sharp Chest Pain: A stabbing pain that often gets worse when you try to take a deep breath or cough.
- Rapid Heart Rate: It feels like your heart is racing or pounding out of your chest.
- Unexplained Cough: A sudden cough that might even bring up bloody sputum.
- Dizziness or Fainting: Feeling lightheaded or actually passing out is a huge red flag.
To help you tell the difference at a glance, we've put together this quick reference table.
Symptoms of DVT vs Pulmonary Embolism and When to Seek Care
Remembering this distinction is key—a DVT needs prompt medical attention from your care team, while a PE requires emergency care without any delay.
Unfortunately, these events aren't rare. Large studies show that among cancer patients on chemotherapy, the incidence rate is around 6% for DVT and 4% for PE. At Hirschfeld Oncology, we make sure every patient knows these signs as a critical part of their self-care during treatment.
How Doctors Diagnose and Treat Blood Clots
When we suspect a blood clot, time is of the essence. We move quickly and methodically to get a firm diagnosis and begin treatment, and knowing what to expect can make a stressful situation feel much more manageable. The goal is simple: confirm if a clot is present and, if so, get you on a safe and effective treatment plan right away.
It all starts with a conversation and a physical exam. We'll talk through your symptoms, and from there, we’ll order specific tests to see what's really going on inside your blood vessels.
Pinpointing the Problem: Diagnostic Tools
Fortunately, we have excellent, reliable tools to investigate a potential clot. The test we choose really depends on your symptoms and where we think the clot might be—a deep vein thrombosis (DVT) in a leg, for example, or a pulmonary embolism (PE) in the lungs.
Here are the most common diagnostic tests we use:
- D-dimer Blood Test: This test looks for a substance your body releases when a blood clot starts to break down. A negative D-dimer test is a great sign—it strongly suggests a clot isn't the problem. A positive result, however, isn't a definitive "yes." Things like recent surgery or even the cancer itself can raise D-dimer levels, so a positive test means we need to keep investigating.
- Doppler Ultrasound: This is our go-to for a suspected DVT. It’s a completely non-invasive scan that uses sound waves to create a real-time map of blood flowing through your veins. It lets the technician clearly see if a clot is causing a blockage.
- CT Pulmonary Angiogram (CTPA): When we're concerned about a clot in the lungs, this is the gold standard for diagnosis. It's a special type of CT scan where a contrast dye is injected into a vein. This dye makes the blood vessels in your lungs light up on the scan, revealing any blockages with incredible clarity.
Once a clot is confirmed, we pivot immediately to treatment. Our focus is two-fold: prevent the existing clot from getting bigger and stop any new ones from forming.
Starting Treatment with Anticoagulants
The cornerstone of blood clot treatment is a group of medications called anticoagulants, which most people know as "blood thinners." It's a bit of a misnomer—they don't actually thin your blood. Instead, they work by interrupting the body's clotting cascade, making it much harder for clots to form and giving your body the chance to dissolve the one that's already there.
For anyone undergoing chemotherapy, choosing the right anticoagulant is a critical decision. Your oncology team has to strike a careful balance: we need to treat the clot effectively while managing the risk of bleeding, which can sometimes be increased by cancer treatments.
There are a couple of main types of anticoagulants we typically prescribe.
Common Types of Blood Thinners
Your medical team will select the best anticoagulant for you based on your specific cancer type, your chemotherapy regimen, and your overall health.
- Low-Molecular-Weight Heparin (LMWH): These are given as a small injection just under the skin, usually in the abdomen. Drugs like enoxaparin are often our first choice for cancer patients because they work predictably and effectively. We find that most people (or their caregivers) quickly get the hang of giving these shots at home.
- Direct Oral Anticoagulants (DOACs): These are pills, like apixaban or rivaroxaban, which have become more popular because they are so convenient. However, we have to be thoughtful when prescribing them, as some can interact with specific chemotherapy drugs. We'll always double-check for any potential conflicts.
Treatment with an anticoagulant usually lasts for at least three to six months. In many situations, especially while you're still undergoing active cancer treatment, we may continue it for longer. Throughout this period, your team at Hirschfeld Oncology will monitor you closely, ready to adjust your treatment as needed to keep you protected from clots and safe from bleeding complications.
Taking Control: Proactive Steps to Prevent Blood Clots

Hearing about the risk of blood clots during chemotherapy can be unsettling, but it’s crucial to know that you aren't powerless. By taking an active role in your own care, you can significantly reduce your chances of developing one.
It really comes down to a combination of simple, everyday habits and clear communication with your medical team. These proactive measures can turn anxiety into action, helping you stay safer and feel more in control throughout your treatment.
Lifestyle Tweaks to Keep Your Blood Moving
One of the most powerful tools you have is movement. When you’re sedentary for long stretches—whether in an infusion chair or resting at home—the blood in your legs can pool and slow down. That sluggish flow creates the perfect environment for a clot to form.
Even small, gentle movements can make a huge difference in keeping your circulation healthy.
- Pump Your Ankles: While sitting, just point your toes up towards your head, then point them down towards the floor. It’s a simple motion, but doing it 10-15 times every hour really helps.
- Do Seated Leg Lifts: Lift one leg straight out, hold it for a few seconds, and then lower it back down. Switch to the other leg.
- Stay Hydrated: This one is easy to overlook but so important. Drinking plenty of water keeps your blood from getting too thick, making it flow more freely and clot less easily.
When you have the energy, even a short walk around the house is fantastic for circulation. Getting ready for treatment can also play a role; check out our guide on how to prepare for chemotherapy for more tips to help you feel prepared.
Medical Prevention and Your Personal Risk Score
Your oncologist is your partner in prevention. For patients who are at a higher risk of clots, we often recommend specific medical strategies to stop a clot before it ever starts. We call this prophylaxis.
To figure out who needs this extra protection, we don’t just guess. We use clinical tools to assess your individual risk.
One of the most widely used methods is the Khorana score. It's a point-based system that looks at your specific cancer type, pre-chemotherapy blood work (like platelet counts), and your Body Mass Index (BMI). A higher score points to a greater risk for VTE.
This score isn't a crystal ball, but it gives your oncology team a solid, evidence-based way to personalize your care. If your score is on the higher side, your doctor will likely talk with you about starting a preventative, low-dose blood thinner.
This might be a daily pill or a small injection designed to keep your blood from getting "sticky" during treatment. We always make this decision together, carefully weighing the benefit of preventing a clot against any potential side effects, like an increased risk of bleeding.
Your voice is the most important part of this process. Never hesitate to ask your Hirschfeld Oncology team directly: “What is my personal risk for a blood clot, and what’s our plan to manage it?” That single question can kickstart one of the most important conversations you’ll have during your treatment.
Let's Talk About Chemo and Blood Clots: Your Questions Answered
When you're dealing with a cancer diagnosis, you're already juggling a ton of new information. So, when you hear that your treatment might increase your risk of blood clots, it's natural to have a lot of questions. Let's walk through some of the most common concerns we hear from patients.
How Long Am I at Risk for a Clot After Chemo Finishes?
Your highest risk is definitely during active treatment. But even after your last infusion, your body is still working hard to recover, and the risk doesn't just disappear overnight. It remains higher than normal for several months as your system gets back to baseline.
Generally, we see this risk start to drop off significantly around three to six months after your final chemo session. The key is to stay tuned in to your body and know the warning signs of a clot throughout this entire recovery period.
Can I Still Fly on a Plane While Getting Chemotherapy?
This is a great question. Flying is tricky for anyone because sitting still for long stretches in a tight space is a known risk factor for clots. Add chemotherapy to the mix, and that risk gets a bit more serious.
The most important thing to do is talk with your oncologist before you book any flights. They know your specific situation and can give you a green light or suggest precautions to make travel safer. This might include things like:
- Wearing compression stockings to keep blood moving.
- Drinking plenty of water before and during the flight.
- Making a point to get up and walk the aisle every hour or so.
- Doing simple leg and ankle exercises right in your seat.
- For some patients, a preventative dose of a blood thinner might even be prescribed just for the trip.
If I Get a Blood Clot, Does That Mean My Cancer Is Getting Worse?
This is a fear we hear a lot, and it's completely understandable. The short answer is no—getting a blood clot does not automatically mean your cancer has progressed. It's simply a known side effect that can come from the cancer itself or from the strong medicines we use to treat it.
Think of it this way: your oncology team sees a blood clot as a serious, but manageable, medical issue that runs parallel to your cancer care. It's not a sign that your cancer treatment isn't working.
Our job is to treat the clot effectively so we can keep your cancer treatment plan on track. We manage it to keep you safe, allowing us to stay focused on the main goal.
At Hirschfeld Oncology, we believe you should never have to wonder about these things alone. Open conversation is at the heart of everything we do. We're here to give you the information and support you need for every part of your treatment. To see more about our patient-first approach, feel free to visit us at https://honcology.com/blog.





.png)


.png)
.png)




