Receiving a cholangiocarcinoma diagnosis is a lot to take in. It's overwhelming, but it’s important to know there is a clear, evidence-based path forward. The official cholangiocarcinoma treatment guidelines are essentially a roadmap, developed by experts, that doctors use to navigate your care.
Think of them as the collective wisdom of the world’s leading cancer specialists, all distilled into a practical plan.
Charting Your Course Through Treatment Guidelines
When you're dealing with a rare cancer like cholangiocarcinoma, you need a solid strategy, not a series of guesses. This is exactly why treatment guidelines are so crucial. They are put together by the top oncology organizations around the globe, who comb through all the latest research to create a reliable framework for your care.
These documents give oncologists a step-by-step consensus on how to best approach diagnosis, staging, and treatment for every person, at every stage of the disease.
For you and your family, getting familiar with these guidelines can be incredibly empowering. It helps demystify the medical jargon and complex decisions, making the entire process more transparent. When you understand the "why" behind your treatment plan, you can have more confident and informed conversations with your medical team. This guide is here to break it all down for you.
The Organizations Behind the Guidelines
So, who actually creates these roadmaps? A few key groups are responsible for setting the standards of care for cholangiocarcinoma, ensuring every recommendation is safe, effective, and backed by solid science. The most influential organizations are:
- The National Comprehensive Cancer Network (NCCN): An alliance of top-tier cancer centers in the U.S. that produces some of the most widely respected guidelines.
- The European Society for Medical Oncology (ESMO): A major organization that sets the standard for cancer care across Europe and globally.
- The American Society of Clinical Oncology (ASCO): A worldwide leader in cancer research that provides essential practice guidelines for oncologists.
To give you a clearer picture, here’s a quick summary of what these guidelines cover and why each component is so important for your care.
These pillars work together to form a comprehensive strategy, ensuring every aspect of your health and treatment is addressed from day one.
The Foundation of Modern Care
Recent updates have brought major progress, especially in surgery and the medicines used to treat cholangiocarcinoma. The latest 2023 guidelines from groups like the NCCN, along with insights from the European Association for the Study of the Liver (EASL), still point to one clear goal whenever possible: surgery.
For patients whose tumors can be removed, surgical resection remains the cornerstone of treatment and the best shot at a cure. You can explore more about the evolution of these guidelines and what they mean for patients today.
A treatment guideline isn't a rigid set of rules; it's a dynamic, evidence-based map. Its purpose is to help your oncologist personalize the most effective and safest treatment path for you, ensuring you benefit from the collective knowledge of the world's leading cancer experts.
The Critical First Steps: Diagnosis and Staging
Before we can even begin to talk about treatment, we have to get two things absolutely right: an accurate diagnosis and precise staging. Think of this as the foundation of a house—if it’s not solid, everything built on top of it will be unstable. Your medical team needs to know, without a doubt, that it’s cholangiocarcinoma and then map out exactly where it is and how far it’s spread.
Getting to a diagnosis usually involves a mix of sophisticated imaging and lab work. Your doctor will likely order a CT scan or an MRI to get a high-resolution look at your bile ducts and the surrounding neighborhood of organs. Blood work, including liver function tests and tumor markers like CA 19-9, can provide important clues, but they aren't definitive on their own.
The final verdict, the one that confirms everything, comes from a biopsy. A specialist will take a tiny piece of tissue from the suspected tumor, and a pathologist will examine it under a microscope. Seeing those cancer cells is the non-negotiable step that officially starts the clock, according to all major cholangiocarcinoma treatment guidelines.
Mapping the Territory with Staging
Once the diagnosis is locked in, we move on to staging. This is where we create a detailed map of the cancer. Staging answers three critical questions for your oncology team:
- How large is the original tumor? (T)
- Has it spread to nearby lymph nodes? (N)
- Has it traveled, or metastasized, to distant parts of the body? (M)
This TNM system is the universal language doctors use to describe the extent of the cancer. Staging is absolutely vital because it’s the primary driver of your treatment options. A small, contained tumor (early stage) is a completely different ballgame than a cancer that has spread (advanced stage).
Staging isn’t just about putting a label on your cancer; it’s a strategic roadmap. It allows your medical team to match your exact situation to the most effective, evidence-based therapies, ensuring the treatment is just right—not too aggressive, but not too weak either.
This decision tree gives you a great visual of how that initial diagnosis splits into two main paths: one for cancer that can be surgically removed (resectable) and one for cancer that can't (unresectable).
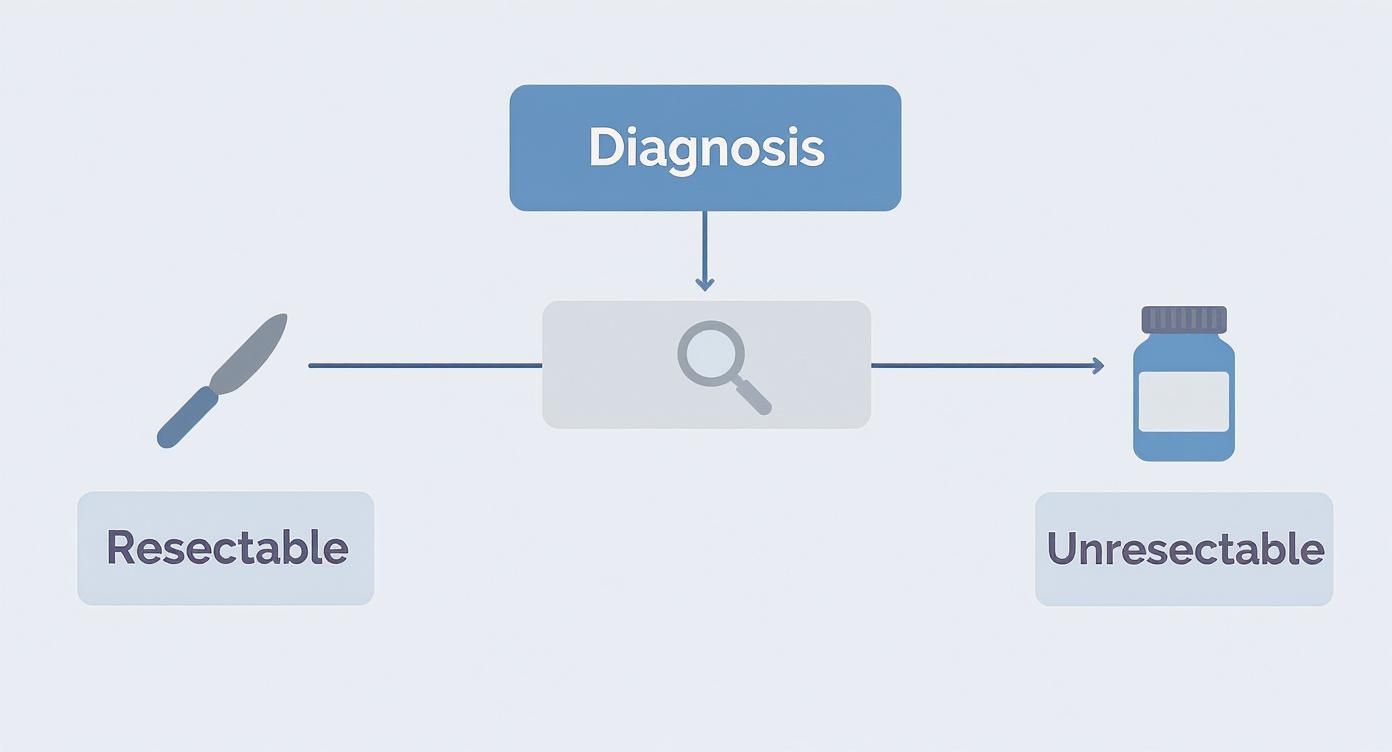
As the infographic shows, everything hinges on that initial workup. The results from your diagnosis and staging are what point your team toward either surgical or non-surgical treatments as the next step.
Why This Phase Is So Important
Getting the diagnosis and staging right from the get-go has a massive ripple effect on your entire treatment journey. A mistake here could lead to the wrong plan, which is why it's so important to nail this step. For a rare disease like this, it's often a smart move to get a second opinion from a center that sees a high volume of these cases.
Ideally, a multidisciplinary team—surgeons, radiologists, oncologists, and pathologists—will all put their heads together to review your results and agree on the cancer's stage. This team approach makes sure every angle is covered before a single treatment decision is made. Understanding this initial process is your first step toward being an active, empowered partner in your own care.
To get a more detailed look, you can learn more about bile duct cancer and how it's managed. This initial evaluation truly sets the stage for everything that follows in your treatment plan.
Understanding Surgery and Liver-Directed Therapies

When cholangiocarcinoma is caught before it has spread beyond the liver and bile ducts, our first and most aggressive goal is a cure. All major cholangiocarcinoma treatment guidelines—from NCCN to ESMO—agree that surgery is the clearest path to achieving that. The entire strategy revolves around one thing: completely removing the tumor, a procedure we call a resection.
But not every tumor can be taken out. The first critical question your medical team has to answer is whether the cancer is resectable (removable) or unresectable (not removable). This decision is the fundamental fork in the road that shapes your entire treatment journey.
A resectable tumor can be fully extracted along with a clean margin of healthy tissue around it, which helps ensure no cancer cells are left behind. On the other hand, an unresectable tumor might be too large, tangled with major blood vessels, or in a location that makes safe, complete removal impossible. Figuring this out isn't a one-person job; it's a team decision made by your surgeon, medical oncologist, and radiologist working together.
The Role of Liver Resection
For patients whose cancer is resectable and located within the liver (intrahepatic cholangiocarcinoma), a liver resection is the gold standard. This is a major operation where a surgeon removes the part of the liver that contains the tumor. It’s complex work that demands a highly skilled and experienced surgical team.
Thankfully, the liver has a unique ability to regenerate. Even if a large piece is removed, it can often grow back to its normal size. The true measure of success for this surgery is achieving an "R0 resection," which means that when the removed tissue is examined under a microscope, no cancer cells are found at the edges. Getting that clean margin is the single best predictor of long-term survival.
When Surgery Isn't the First Step
Sometimes, a tumor falls into a gray area called "borderline resectable." It might be technically possible to remove, but its size or position makes the surgery risky.
In these situations, your team may recommend shrinking the tumor first with treatments like chemotherapy or radiation. This is called neoadjuvant therapy, and its goal is to make the eventual surgery safer and more likely to succeed.
Exploring Liver-Directed Therapies
So, what happens if the tumor is clearly unresectable? This is where liver-directed therapies become incredibly important. Think of them as targeted strikes aimed directly at the cancer inside the liver, sparing the rest of the body. They are powerful tools when surgery is off the table.
Key liver-directed therapies include:
- Ablation: This technique essentially cooks or freezes the tumor to death. A specialist inserts a thin, needle-like probe directly into the cancer and uses either extreme heat (radiofrequency ablation) or cold (cryoablation) to destroy the cells.
- Embolization: This strategy cuts off the tumor's food and oxygen supply. Tiny particles are injected into the artery that feeds the cancer, blocking blood flow and starving it. Sometimes, this is combined with chemotherapy in a procedure called chemoembolization (TACE), delivering a potent dose of drugs right where they're needed most.
These aren't just backup plans; they are highly specialized weapons. By concentrating the attack on the liver, these therapies can control the cancer's growth and relieve symptoms with fewer side effects throughout the body. They are a cornerstone of managing unresectable disease.
The Option of Liver Transplantation
In a few very specific cases, a liver transplant might be considered. This is a potential cure, but it's an option for only a small group of patients, usually those with early-stage, unresectable hilar cholangiocarcinoma (cancer found right where the bile ducts exit the liver).
The eligibility criteria are incredibly strict. Patients must undergo a rigorous evaluation to see if their tumor's size and location fit within the established guidelines. While it's not a common path, a transplant can offer the hope of a cure for the right person when a standard resection isn't possible.
Systemic Treatments: Chemotherapy and Immunotherapy
When cholangiocarcinoma is too advanced for surgery or has spread beyond the bile ducts, our treatment approach has to change. We can no longer rely on localized attacks like surgery. Instead, we need therapies that can travel through the bloodstream to fight cancer cells wherever they might be hiding.
These are called systemic treatments, and they are the cornerstone of care for what we call unresectable (inoperable) or metastatic disease.
For a long time, chemotherapy was our main tool in this fight. Think of it as a powerful, body-wide therapy designed to attack any cells that are dividing rapidly—a hallmark of cancer. Chemotherapy works everywhere, helping to slow the cancer’s growth, ease symptoms, and improve survival.
The most trusted and proven chemotherapy combination for cholangiocarcinoma consists of two drugs: gemcitabine and cisplatin. You'll often hear this referred to by the shorthand GEMCIS. For years, this duo has been the go-to first-line defense, providing a solid foundation for treatment plans.
The Standard First-Line Chemotherapy Regimen
When an oncologist recommends GEMCIS, they’re drawing on years of clinical data that show these two drugs work much better together than either one does alone. They attack the cancer in different ways, which boosts their overall effectiveness.
The goals of using systemic therapy can shift depending on the situation:
- Palliative Therapy: For advanced cancer, the primary aim is to control the disease, relieve symptoms like pain or fatigue, and maintain the best possible quality of life. The focus is on managing the cancer as a chronic illness.
- Adjuvant Therapy: Sometimes, even after a successful surgery, there's a risk that microscopic cancer cells were left behind. In that case, your doctor might recommend a course of chemotherapy to hunt down and destroy these stray cells, reducing the chances of the cancer coming back.
The decision to use chemotherapy and the specific goals of treatment are always personalized, based on your diagnosis, the cancer’s stage, and your overall health, following established cholangiocarcinoma treatment guidelines.
A Major Advance: Adding Immunotherapy
Recently, a massive step forward has changed the game for many patients. We've discovered that adding an immunotherapy drug to the standard GEMCIS chemotherapy can deliver significantly better results for people with advanced cholangiocarcinoma.
So, how does this work? Imagine your immune system’s T-cells are like highly trained guard dogs, programmed to find and destroy threats like cancer. Cancer cells, however, are devious. They can put a "brake" on these T-cells, essentially telling them to back off and ignore the threat.
Immunotherapy drugs, specifically a class called immune checkpoint inhibitors, work by releasing this brake. This simple action unleashes your T-cells, allowing them to finally recognize the cancer cells as a target and attack them. It’s not about adding a new weapon—it's about empowering your body's own defenses to do the job they were meant to do.
The New Gold Standard Combination
This powerful synergy has quickly made the combination of GEMCIS plus an immune checkpoint inhibitor the new first-line standard for most people with inoperable or metastatic cholangiocarcinoma.
The latest clinical practice guidelines, including the 2024 update from EASL, now recommend this approach, showing a clear shift toward more effective, multi-faceted strategies. While surgery remains the only potential cure for localized tumors, this combination therapy offers new hope and better outcomes for controlling cancer that has spread. You can review the latest cholangiocarcinoma guidelines from EASL to see the data behind this change.
Understanding these powerful therapies is crucial. For a closer look at how your immune system can be harnessed to fight cancer, our detailed guide explains what immunotherapy is and how it fights cancer. This combination truly marks a new era in treatment, blending the raw power of chemotherapy with the targeted intelligence of your own immune system.
Cracking the Code: How Targeted Therapies Are Changing the Game

Standard chemotherapy has been a cornerstone of cancer treatment for decades. It's powerful, but it's a bit like a sledgehammer—it hits both cancerous and healthy rapidly-dividing cells. Today, for some patients, we can be much more precise. This is where personalized medicine comes in, shifting the entire treatment paradigm from the cancer's location to what's actually driving it.
This approach all hinges on something called molecular profiling. Think of it as creating a detailed genetic blueprint of your specific tumor. By analyzing a small piece of tissue, we can pinpoint the exact genetic mutations that are telling the cancer cells to grow and spread. It's like a mechanic diagnosing a single faulty wire in a complex engine instead of just replacing the whole thing.
Modern cholangiocarcinoma treatment guidelines from major cancer organizations now consider molecular profiling a standard of care for anyone with advanced disease. It's not an afterthought; it's a critical first step. This testing can reveal specific vulnerabilities in the cancer that can be attacked with a new class of drugs known as targeted therapies.
Unlocking Treatment With Key Genetic Markers
When we run these molecular tests, we're on the hunt for a handful of specific genetic alterations. If your tumor has one of these "targets," it unlocks a whole new set of treatment possibilities designed specifically for you. These are the most important markers we look for.
FGFR2 Fusions or Rearrangements: Found in roughly 10-16% of people with intrahepatic (inside the liver) cholangiocarcinoma, these fusions act like a gas pedal that's stuck to the floor. Specialized drugs called FGFR inhibitors are designed to get in there and block that runaway signal.
IDH1 Mutations: This change, present in up to 20% of intrahepatic cases, causes the cell to produce a substance that fuels cancer growth. IDH1 inhibitors work by shutting down this abnormal production line, essentially starving the cancer of its fuel.
HER2 Amplification: While famous for its role in breast cancer, an overactive HER2 protein can also drive some bile duct cancers. When we find it, we can use established HER2-blocking drugs to great effect.
BRAF V600E Mutations: This specific mutation is another "on" switch that tells cancer cells to multiply uncontrollably. It's less common in cholangiocarcinoma, but if it’s there, we have targeted BRAF inhibitors that can flip that switch off.
You can get a closer look at the science behind how these drugs work by reading our guide to the mechanisms of targeted therapy.
Matching the Right Drug to the Right Target
Identifying a genetic target is the first step. The next is matching it to an approved drug that can actually hit it. Fortunately, the science has moved quickly, and we now have a growing arsenal of therapies that line up with these specific genetic findings.
The table below shows how a specific molecular test result can directly lead to a recommended treatment plan.
This connection is what makes molecular profiling so vital. Without this testing, we would never know these highly effective options were on the table.
Think of a tumor’s genetic code as a lock. Standard chemotherapy is like trying to break the door down. Targeted therapy is the specific key, engineered to fit that one lock perfectly and stop the cancer in its tracks.
It's crucial to understand that targeted therapy isn't a fit for every patient; the tumor must carry one of these specific mutations. But for those who are a match, it represents a powerful, guideline-backed strategy that can improve outcomes and often comes with a more manageable side-effect profile than traditional chemotherapy. The most important step you can take is to ask your doctor about comprehensive molecular profiling to see if this personalized path is right for you.
Your Action Plan: What to Ask Your Doctor
When you're facing a cholangiocarcinoma diagnosis, you become the most important member of your own healthcare team. To make the most of your appointments, it helps to walk in prepared. Think of these conversations with your oncologist as planning sessions where your voice matters.
Being armed with the right questions helps you partner with your doctor to make sure your treatment plan is built on the most current, evidence-based guidelines. It’s about making sure every stone has been turned over.
First Things First: Diagnosis and Treatment Plan
Your initial questions should focus on getting a crystal-clear picture of your specific cancer and the recommended path forward. These are the foundational questions that tie directly into the cholangiocarcinoma treatment guidelines we've been discussing.
- Has my tumor had comprehensive molecular profiling? This is the single most important question you can ask. Without it, you and your doctor won't know if you're a candidate for powerful targeted therapies.
- Can I have a copy of the molecular profiling report? Don't just settle for a summary. You need to know the specifics—like whether you have an FGFR2 fusion, an IDH1 mutation, or another actionable biomarker. This report is your roadmap.
- Given my stage and molecular results, what is the standard-of-care treatment? This question helps confirm that the proposed plan aligns with established NCCN or ESMO guidelines, which represent the consensus of top cancer experts.
- Are there any clinical trials that I might be eligible for? Trials aren't a last resort; they can provide access to the next wave of promising treatments. It's a conversation worth having right from the start.
Looking at the Bigger Picture: Palliative Care and Second Opinions
Effective cancer care is about more than just treating the tumor. It’s also about managing symptoms, maintaining your quality of life, and feeling confident in your decisions.
Palliative care is a key part of this, but it's often misunderstood. It’s not just for end-of-life situations. It's a specialized layer of support focused on relieving the symptoms, pain, and stress of a serious illness. The goal is simple: to improve your quality of life, for both you and your family.
Think of palliative care as a support system that works alongside your main cancer treatment. Bringing it in early can make a huge difference in managing side effects, helping you tolerate therapy better, and making sure your well-being is a top priority from day one.
For a rare and complex cancer like this one, getting a second opinion is not just common; it's smart. It isn't a sign of mistrusting your doctor. It's a way to ensure you've explored every possible angle, especially with an expert at a major cancer center that sees a high volume of cholangiocarcinoma cases.
Here are a few questions to help you start these important conversations:
- How can we bring palliative care into my treatment plan now? It's best to be proactive. Frame it as a way to get ahead of potential symptoms like pain, fatigue, or nausea before they become a major problem.
- Would you recommend I get a second opinion? Your oncologist should be supportive of this. You can even ask for a recommendation or for their office to help send your medical records to another specialist.
- What are the biggest risks and benefits of the plan you're proposing? Getting a clear, honest answer helps you weigh the options and make sure the treatment aligns with your personal goals for your life.
By asking these questions, you shift from being a patient to being an advocate for your own health. It ensures every decision is made together, with careful thought, and is aimed at giving you the best possible outcome.
Your Top Questions About Treatment, Answered
When you're dealing with a cholangiocarcinoma diagnosis, you're bound to have questions. This is complex stuff. Let's break down some of the most common ones to give you a clearer picture of the road ahead.
How Do Doctors Decide Which Guidelines to Follow?
Think of treatment guidelines as a meticulously crafted roadmap, not a rigid set of rules. Your oncologist will likely reference frameworks from major expert groups like the NCCN (National Comprehensive Cancer Network) in the U.S. or ESMO (European Society for Medical Oncology) in Europe.
The good news is that these guidelines are largely in sync, reflecting a global agreement on the best ways to treat this cancer. Your doctor will select the most appropriate framework based on where you live and then fine-tune it to fit the specific details of your cancer, your health, and your personal goals.
What if My Tumor Doesn't Have a "Targetable" Mutation?
It can feel disheartening if molecular testing doesn't turn up a specific genetic "target," but it absolutely does not mean you're out of options. Not by a long shot.
In this case, your care team simply pivots to other powerful, proven therapies. The standard of care for many patients with advanced cholangiocarcinoma is a combination of chemotherapy and, increasingly, immunotherapy. These are highly effective, well-established treatments. The purpose of testing is to see if a shortcut exists; if not, we take the main, reliable highway.
The key takeaway here is that molecular testing is about exploring every possible advantage. If a specific genetic target isn't found, you and your team will move forward with confidence, using the best guideline-approved therapies available.
While cholangiocarcinoma is considered rare, its presence is growing worldwide. In the U.S. alone, the National Cancer Institute projected over 41,000 new cases of liver and intrahepatic bile duct cancers for 2023. To dig deeper, you can explore these cholangiocarcinoma incidence trends and see how they're shaping research.
Should I Look into Clinical Trials?
Absolutely. Every major treatment guideline strongly encourages considering clinical trials. They aren't a "last resort"; they are a fantastic option that gives you access to the next wave of promising treatments before they become widely available.
This is especially true for cancers that are advanced or have been difficult to treat with standard therapies. It's always worth asking your oncologist, "Is there a clinical trial that might be a good fit for me?" That one question can open up a whole new set of possibilities.
At Hirschfeld Oncology, our entire focus is on building a personalized treatment strategy that aligns with the latest guidelines and the specific molecular story of your cancer. If you're looking for clarity on your diagnosis or want to discuss advanced options like targeted therapy and immunotherapy, we're here to help. You can learn more by visiting our blog.





.png)


.png)
.png)




