When you first hear the words “colon cancer,” it can feel like you’re suddenly trying to learn a new language. Of all the new terms coming your way, the most important one to understand is staging. Staging is simply how doctors describe the size of a cancer and whether it has spread. Think of it as creating a precise map of the cancer, which will guide every single treatment decision we make together.
Decoding Your Diagnosis: A Clear Guide to Staging

Getting a handle on the stage of your colon cancer is the first, most crucial step in moving forward. Staging creates a common language for your entire medical team, allowing us to define the cancer’s specific characteristics, anticipate its behavior, and design the most effective treatment plan just for you. It helps turn a confusing diagnosis into a clear, actionable roadmap.
My goal here is to break down the medical jargon into plain English. We’ll walk through what each stage means for your health, clearing up the confusion so you can feel more in control and ready for the conversations ahead. Staging is much more than just a label; it’s the key that unlocks answers about your health and your future.
Why Staging Matters
At its core, staging is all about clarity. It gives both you and your oncology team a shared understanding of the cancer's extent and what that means for the journey ahead.
Specifically, staging helps us:
- Guide Treatment Decisions: Your cancer's stage is the single biggest factor in deciding if surgery, chemotherapy, radiation, or a combination of treatments is the right path.
- Predict Prognosis: While everyone’s journey is unique, the stage provides a general outlook on what to expect, which helps in planning for recovery.
- Standardize Communication: It creates a consistent framework that allows doctors and researchers all over the world to compare notes and improve treatment outcomes for everyone.
The impact of this disease is significant. The World Health Organization reported that in 2020 alone, there were over 1.9 million new cases of colorectal cancer and more than 930,000 deaths. These numbers make it the second leading cause of cancer-related deaths globally and underscore why deeply understanding your diagnosis is so critical.
Staging is the cornerstone of your cancer care plan. It’s the process of finding out how much cancer is in the body and where it is located. Knowing the stage helps your doctor recommend the best course of treatment and predict your prognosis.
This guide will focus on the TNM system—the universal language of staging—and we’ll explore what each stage means in detail. My aim is to give you the knowledge you need to be an active participant in your own care. By understanding your specific stage, you become an empowered partner in your treatment. You can find more information on our approach to various types of colon cancer here.
How Doctors Determine Your Cancer Stage
Figuring out your exact cancer stage is a bit like a detective gathering clues. Before we can map out the best treatment path, we first need a clear picture of what we're dealing with—where the cancer is, how big it is, and whether it has started to travel. This process involves a few key tests, each one giving us a vital piece of the puzzle.
It usually starts with a colonoscopy, which gives us our first look inside the colon and confirms if a tumor is present. During that procedure, we’ll take a small tissue sample, called a biopsy. A pathologist then examines that sample under a microscope to confirm that it's cancer and to learn more about its specific characteristics.
But a colonoscopy and biopsy only tell us part of the story. They show us what's happening on the surface, but not how deeply the tumor has grown into the colon wall or if it has spread elsewhere. That’s where imaging tests come in.
Creating a Clear Picture with Imaging Tests
To see the whole picture, your doctors will almost certainly order advanced imaging scans. Don't worry—these tests are painless and non-invasive, but they create incredibly detailed images of the inside of your body.
Some of the most common scans we use for staging are:
- CT (Computed Tomography) Scan: This is often our go-to imaging tool. A CT scan uses a series of X-rays to build a 3D view of your chest, abdomen, and pelvis. It’s excellent for checking if the cancer has spread to distant organs like the liver or lungs.
- MRI (Magnetic Resonance Imaging) Scan: An MRI uses powerful magnets and radio waves to create even more detailed images. We find it especially helpful for rectal cancer, as it shows us exactly how far the tumor has grown into the rectal wall and helps us spot any spread to nearby lymph nodes.
- PET (Positron Emission Tomography) Scan: In certain situations, particularly if we suspect the cancer may have spread but aren't sure where, a PET scan can be very useful. This scan highlights areas of high metabolic activity, which helps us spot cancer cells anywhere in the body.
Each of these tests adds another layer of crucial information to your "map," ensuring your treatment plan is built on the most accurate and complete understanding of your cancer.
The TNM System: The Language of Staging
Once all the test results are back, your oncologist puts all the pieces together using a standardized method called the TNM staging system. This is the universal language doctors use to describe cancer, ensuring everyone on your care team is on the same page.
Think of it like giving a specific address for the cancer. You need a street, a city, and a zip code to know exactly where something is. The TNM system works the same way, using three key pieces of information to define the colon cancer stages.
Here’s what each letter stands for:
- T for Tumor: This describes the primary tumor itself—specifically, how deeply it has grown into the wall of the colon or rectum. The "T" gets a number from 1 to 4; the higher the number, the deeper it has grown.
- N for Nodes: This tells us whether the cancer has spread to any nearby lymph nodes. The "N" value (ranging from 0 to 2) indicates if cancer cells are present in those nodes and, if so, how many are involved.
- M for Metastasis: This is the "big picture" letter. It tells us if the cancer has spread, or metastasized, to distant parts of the body, like the liver, lungs, or bones. "M" is either 0 (no distant spread) or 1 (it has spread).
By combining the T, N, and M values, your doctor arrives at a precise classification for your cancer. This TNM "address" is then translated into the overall stage number you’re more familiar with—Stage 0 through Stage IV.
This systematic approach takes the guesswork out of the equation. It turns a lot of complex medical data into a clear, understandable stage that becomes the foundation for your personalized treatment plan. Knowing your TNM classification is the first step toward understanding the strategy your care team will build with you.
Breaking Down the Stages of Colon Cancer
After all the tests are back—the biopsies, the CT scans, the bloodwork—your oncology team will take that complex data and distill it into something much clearer: a stage. Colon cancer is staged from 0 to IV, and this number is far more than just a label. It's a universal language that helps everyone on your care team understand exactly how advanced the cancer is, which is the key to mapping out the best possible treatment plan for you.
Think of it this way: the initial tests give us the raw coordinates of the cancer. The stage then places those coordinates on a map, showing us precisely where you are in this journey. Is the cancer a tiny, localized growth? Or has it started to travel? Knowing your stage is the first, most critical step in navigating the road ahead.
The visual below illustrates how we get to that final stage. It’s all based on three key factors: the Tumor (T), its spread to lymph Nodes (N), and whether it has Metastasized (M) to distant parts of the body.
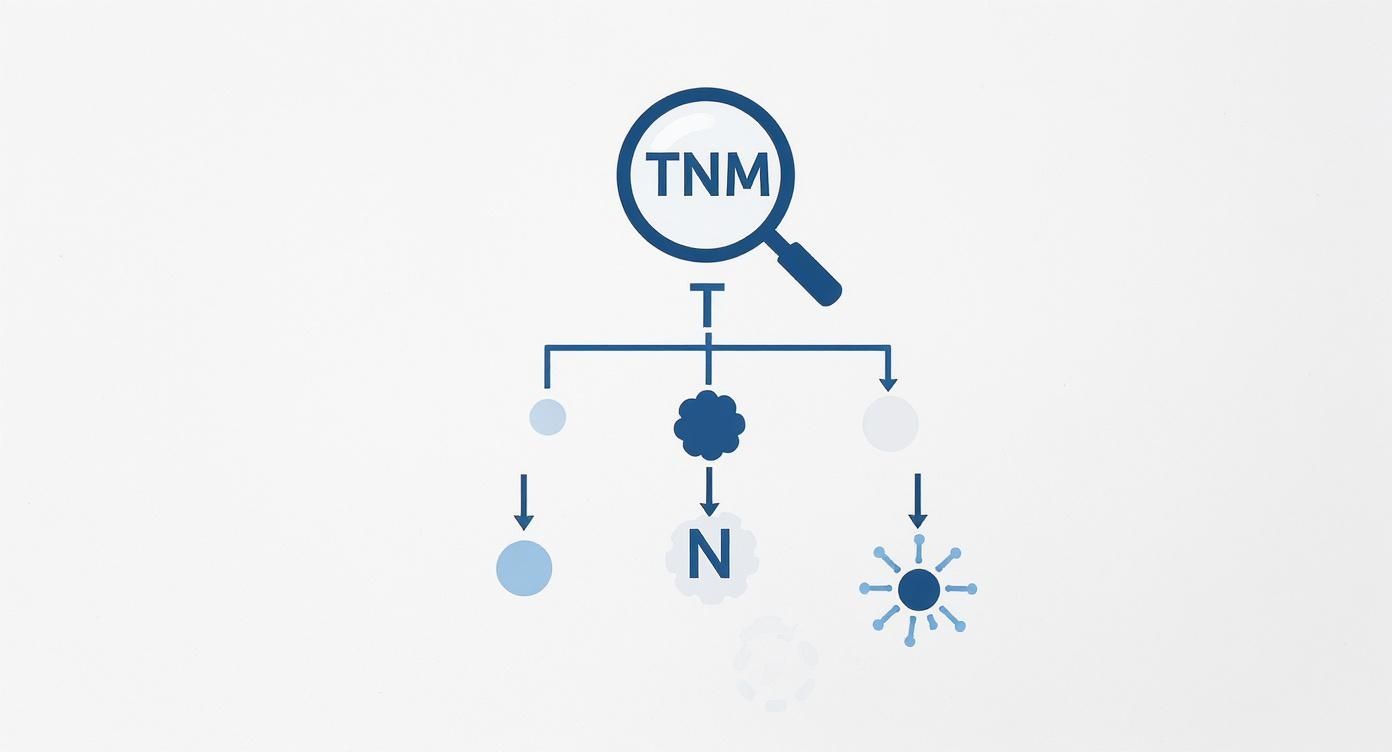
Each piece of the TNM puzzle—how deep the tumor has grown, if it's in the lymph nodes, and where else it might be—comes together to give us a single, comprehensive stage.
Stage 0: The Earliest Form
Stage 0, also known as carcinoma in situ, is the earliest possible detection of colon cancer. At this point, it’s not even a true "cancer" in the invasive sense. The abnormal cells are found only in the mucosa, which is the very innermost lining of your colon.
These cells haven't broken through this top layer into the deeper tissues of the colon wall. Because it’s completely contained, it’s considered non-invasive.
The good news? Treatment is often remarkably simple. In most Stage 0 cases, the entire group of abnormal cells can be removed during a colonoscopy in a procedure called a polypectomy. That single procedure can be both the diagnosis and the cure, meaning no further treatment is usually needed beyond follow-up surveillance.
Stage I: Localized Cancer
When we talk about Stage I colon cancer, we mean the tumor has started to grow into the deeper layers of the colon wall, but it’s still confined entirely within the colon itself.
It has pushed past the mucosa into the submucosa or perhaps even the main muscle layer. Think of it like a plant that has put down slightly deeper roots but hasn't yet started to spread its seeds. Crucially, it has not reached any lymph nodes or distant organs.
Surgery is the gold standard for Stage I. The goal is to remove the section of the colon that contains the tumor, plus a bit of healthy tissue on either side just to be safe. For the vast majority of people with Stage I disease, that's it. The surgery is curative, and chemotherapy isn't necessary.
Stage II: Regional Growth
Stage II means the tumor has become more invasive, growing all the way through the muscular wall of the colon to its outermost layers. In some cases, it may even be touching or stuck to nearby tissues or organs. The critical distinction for Stage II, however, is that it has not yet spread to any lymph nodes.
This stage has a few subcategories based on just how far the tumor has gone:
- Stage IIA: The cancer has reached the serosa, the colon's outermost layer.
- Stage IIB: The cancer has grown through the colon wall and is now attached to or invading nearby structures.
- Stage IIC: The tumor has pushed all the way through the colon wall and perforated it, creating a hole.
Surgery to remove the cancerous part of the colon is still the main treatment. But for some people with higher-risk Stage II cancer (like a perforated tumor), we may recommend chemotherapy after surgery. This is called adjuvant chemotherapy, and it’s a protective measure to wipe out any stray cancer cells and lower the chances of the cancer coming back.
Your oncology team will carefully examine the removed tumor for high-risk features to determine if chemotherapy is a necessary next step. This decision is highly personalized and based on your unique situation.
Stage III: Spread to Lymph Nodes
The moment cancer cells are found in nearby lymph nodes, the diagnosis becomes Stage III. This is the defining feature, no matter how big or small the primary tumor is.
The body's lymph nodes act like a drainage and filtering system. If cancer cells get into them, it’s a sign that the disease has found a potential highway to travel to other parts of the body. This automatically increases the risk that the cancer could return even after a successful surgery.
Because of this heightened risk, the standard of care for Stage III is a two-pronged attack: surgery followed by adjuvant chemotherapy. The surgery gets rid of the main tumor, and the chemotherapy works systemically to hunt down and destroy any microscopic cancer cells that might have escaped.
Stage IV: Metastatic Disease
Stage IV is the most advanced stage. It means the cancer has metastasized—it has spread from the colon to distant organs.
The most common places for colon cancer to travel are the liver and the lungs, but it can also show up in the brain, bones, or lymph nodes far from the original tumor. When cancer reaches this stage, the treatment goals shift. We focus on controlling the disease, shrinking tumors, relieving symptoms, and extending and improving your quality of life.
While surgery to remove the colon tumor might still be an option, the foundation of treatment becomes systemic therapies that can fight cancer throughout the entire body. This often involves a combination of:
- Chemotherapy: To attack fast-growing cancer cells.
- Targeted Therapy: Modern drugs that zero in on specific weaknesses in the cancer cells.
- Immunotherapy: Powerful treatments that unleash your own immune system to fight the cancer.
Even at Stage IV, there are many effective treatments available. The field is constantly evolving, giving us more tools than ever to manage advanced disease and help our patients live longer, fuller lives.
Overview of Colon Cancer Stages, Treatments, and Prognosis
To pull all this information together, the table below provides a snapshot of each stage, what it means, the typical treatment path, and the general prognosis.
It's important to remember that these survival rates are statistics based on large groups of people. They're a helpful guide, but they can't predict any single person's outcome. Your individual prognosis will depend on many factors, including the specific biology of your tumor, your overall health, and how well you respond to treatment. Understanding your stage is the starting point for a productive conversation with your doctor about your personal care plan.
How Staging Shapes Your Treatment Plan
https://www.youtube.com/embed/SGaQ0WwZ_0I
Knowing your specific colon cancer stage is much more than just a label—it’s the actual blueprint your oncology team uses to build a treatment strategy just for you. Each stage comes with its own unique set of circumstances, and that means each requires a different game plan to achieve the best possible outcome. Think of your stage as the starting point on a map; it tells us which route to take.
The goals of treatment can change quite a bit from one stage to the next. For early-stage cancers, the main objective is usually a cure, which we can often achieve with surgery alone. But for more advanced stages, the focus might shift to controlling the disease, managing symptoms, and making sure you maintain a high quality of life.
Let’s walk through how these treatment plans are designed for each stage of colon cancer.
Treating Early Stage Colon Cancer
For Stage I and many Stage II colon cancers, the tumor is still contained within the colon. It hasn't spread to nearby lymph nodes or other parts of the body. When that's the case, surgery is the absolute cornerstone of treatment and, in many cases, is all that's needed for a cure. The surgeon will remove the piece of the colon with the tumor, plus a bit of healthy tissue around it, to make sure no cancer cells are left behind.
After surgery, a pathologist will put the tumor under a microscope to look for certain "high-risk" features. This could mean the cancer cells look particularly aggressive or that the tumor had grown through the colon wall. If a Stage II cancer has any of these features, your oncologist might recommend adjuvant chemotherapy.
Think of this postsurgical chemo as an insurance policy. The goal is to wipe out any microscopic cancer cells that might have broken away from the main tumor but are too tiny for any scan to pick up. This extra step helps lower the chances of the cancer ever coming back.
Addressing Stage III Colon Cancer
Once colon cancer reaches Stage III, it means cancer cells have been found in the lymph nodes near the colon. This is a big deal because it’s a sign that the cancer has figured out how to travel through the body’s lymphatic system. So, even after a successful surgery to remove the tumor and the affected lymph nodes, there's a higher risk that some cells have already ventured out to other places.
Because of this higher risk, the standard approach for Stage III colon cancer is a one-two punch:
- Surgery: First, the surgeon removes the cancerous part of the colon and the nearby lymph nodes.
- Adjuvant Chemotherapy: After you've had some time to recover from surgery, a course of chemotherapy is crucial. It travels through your whole body to hunt down and destroy any of those lingering cancer cells.
This two-step strategy has been proven time and again to dramatically improve survival rates for people with Stage III disease by tackling both the cancer we can see and the cancer we can't.
Your specific stage is a critical piece of the puzzle. Research consistently shows that disease progression and survival outcomes are closely tied to the stage at diagnosis, which is why a stage-appropriate treatment plan is so essential. You can find detailed research on how the disease stage impacts recurrence and survival by reading more on these findings.
Managing Advanced Stage IV Cancer
Stage IV colon cancer, also called metastatic cancer, means the disease has spread to distant organs—most often the liver or lungs. Because the cancer is now widespread, the treatment goals shift away from a simple cure. Instead, we focus on controlling the disease, shrinking tumors to relieve symptoms, and extending your life while preserving its quality.
The foundation of treatment here becomes systemic therapies—medicines that travel through the bloodstream to fight cancer wherever it is in the body. Your oncologist will put together a personalized regimen that might include:
- Chemotherapy: The primary tool used to attack fast-growing cancer cells.
- Targeted Therapy: These are smarter drugs that zero in on specific weaknesses in the cancer cells, often causing fewer side effects than traditional chemo.
- Immunotherapy: These exciting treatments work by unleashing your own immune system to recognize and attack the cancer.
Surgery can still have a role in some Stage IV cases, like removing a limited number of tumors from the liver or lungs. For most people, though, the focus will be on these powerful systemic treatments. The great news is that the field is moving incredibly fast. You can learn more by exploring our guide to advancements in Stage 4 colorectal cancer treatments. These newer options are giving patients more time and a better quality of life than ever before.
Understanding Prognosis and Survival Rates

Talking about the future after a cancer diagnosis can be incredibly tough. It’s completely natural to wonder what your specific stage means for your prognosis and to look for answers in survival rates. These are simply statistics that show the percentage of people with the same type and stage of cancer who are still alive after a certain amount of time, usually five years.
But it’s absolutely critical to remember one thing: you are not a statistic. These numbers are averages based on data from thousands of different people, and they can't possibly account for your unique health, the specific biology of your tumor, or how well you'll respond to treatment.
Think of survival rates less as a prediction and more as a powerful way to illustrate a single, vital point: early detection saves lives. The data is crystal clear—the earlier we find colon cancer, the more treatment options we have and the better the outcomes.
The Impact of Early Detection
The difference in outcomes between cancer found early and cancer that has already spread is staggering. This is precisely why screening is our most important tool in the fight against this disease. When we catch cancer before it has a chance to travel, treatment is generally more straightforward and much more effective.
Data from the American Cancer Society, looking at cases from 2014 to 2020, really drives this home. For patients with localized colon cancer (meaning it's only in the colon or rectum), the five-year relative survival rate is 91%. But, if the cancer spreads to regional areas like nearby lymph nodes, that number shifts to 73%. For cancer that has metastasized to distant parts of the body, the five-year survival rate is 13%. You can see a more detailed breakdown and learn about the impact of staging on survival rates here.
These numbers aren’t meant to scare you. They are a powerful motivator for taking control of your health. They show exactly why routine screenings are not just a casual recommendation—they are a potentially life-saving action for you and the people you love.
Looking Beyond the Numbers
While staging is a major piece of the puzzle, it’s far from the only thing that shapes your prognosis. When we sit down to talk about your outlook and build a care plan, we look at a much wider picture.
Several other important factors come into play:
- Tumor Grade: This is a measure of how aggressive the cancer cells appear under a microscope. Lower-grade tumors generally grow more slowly.
- Genomic Markers: We can now run advanced tests on the tumor itself to find specific genetic mutations. This information can open the door to targeted therapies designed to attack those exact mutations, often with better results and fewer side effects.
- Your Overall Health: Your general health, age, and ability to handle treatment are all crucial elements that influence your outcome.
- Response to Treatment: How your cancer reacts to the first round of therapy gives us invaluable information and helps guide our next steps.
Your prognosis is a dynamic, personal, and evolving picture. Incredible progress is being made every day, and new treatments are constantly improving outcomes for patients at all colon cancer stages. To learn more about how we're personalizing care, take a look at our guide on genomic profiling and its impact on gastrointestinal cancer treatment. These advancements are making yesterday's statistics obsolete.
Planning Your Next Steps in NYC
Getting a colon cancer diagnosis is a heavy weight to carry. It can leave you feeling lost and overwhelmed, but the first step toward taking back control is to create a clear, actionable plan. For anyone in the New York City area, this starts with putting together a team of experts who can help you make sense of your diagnosis, from understanding the different colon cancer stages to what they mean for your future.
A crucial part of this process—and one I always recommend—is getting a second opinion. This isn't about doubting your first doctor; it's about confirming your diagnosis, stage, and the proposed treatment plan. Think of it as due diligence for your own health. It provides the peace of mind that comes from knowing every angle has been considered, so you can feel confident in the road ahead.
Finding an Expert Partner in Your Care
Navigating cancer treatment in a place like NYC means finding a specialist who truly understands the intricate details of advanced care. At Hirschfeld Oncology, our team, led by Dr. Azriel Hirschfeld, is dedicated to offering not just expert consultations but compassionate, personalized guidance. We see our role as being your partner on this journey, exploring every single option right alongside you.
This partnership includes in-depth conversations about innovative treatments and access to clinical trials that might be a good fit for your specific situation. Having an experienced guide ensures your treatment strategy is built just for you.
Taking the time to get a comprehensive second opinion isn’t a delay in your treatment. It's a critical investment in your health and your peace of mind, empowering you to move forward with a plan built on certainty and collaboration.
If you or someone you love is facing a colon cancer diagnosis, please know you don’t have to figure this all out on your own. We encourage you to reach out to us at Hirschfeld Oncology. Let our team provide the clarity and support you need to make informed decisions and start your treatment with confidence. Making that connection could be the most important next step you take.
Your Top Questions About Cancer Staging, Answered
After taking in all this information about the different stages of colon cancer, it's completely normal to have some questions still rattling around. Let's tackle some of the most common ones that come up after a diagnosis, giving you clear, straightforward answers to help you feel more confident in your understanding.
Can a Cancer’s Stage Ever Change?
This is one of the most frequent—and important—questions we hear. The simple answer is no; the original stage given at your diagnosis is a permanent part of your medical record. It does not change.
For example, if you were first diagnosed with Stage II colon cancer and, sometime later, the cancer shows up in your liver, it isn't suddenly reclassified as Stage IV. Instead, your doctors will refer to it as recurrent Stage II colon cancer with metastasis. This detail is crucial because it tells the whole story of your cancer journey and helps guide future treatment decisions.
Stage vs. Grade: What’s the Difference?
It's easy to get "stage" and "grade" mixed up, but they tell us two very different things about a cancer.
Here’s a simple way to think about it:
- Stage answers the question, "Where is the cancer and how far has it traveled?" It’s all about the tumor's size and physical location in the body.
- Grade answers the question, "How aggressive do the cells look?" This is determined by a pathologist looking at the cancer cells under a microscope.
A cancer's grade helps predict its behavior. Low-grade cancer cells look a lot like normal cells and usually grow slowly. High-grade cells, on the other hand, look very abnormal and tend to be more aggressive. Both pieces of information—the stage and the grade—are critical for putting together the most effective treatment plan for you.
How Accurate Is the Initial Staging?
The staging you receive right after your initial tests, like scans and biopsies, is highly accurate based on the available information. This is called the clinical stage.
However, the complete picture often comes into focus only after surgery. Once the tumor and nearby lymph nodes are removed, a pathologist can examine the tissue up close. This leads to the pathologic stage, which is the most definitive and precise assessment. Sometimes, the pathologic stage confirms the clinical stage, and other times it adjusts it slightly. This is a very normal part of the process and helps your care team fine-tune any next steps in your treatment.
Getting a handle on the specifics of your diagnosis is a powerful first step in taking control of your health. At Hirschfeld Oncology, we believe that clarity is key, and we're here to support you every step of the way. If you have questions about your diagnosis or want to discuss treatment options here in NYC, we encourage you to start a conversation with our team. You can learn more about our approach and read our latest insights at https://honcology.com/blog.





.png)


.png)
.png)




