At its core, a monoclonal antibody is a laboratory-engineered protein that acts like a heat-seeking missile for your immune system. Each one is designed to recognize and latch onto a very specific target—called an antigen—found on the surface of cancer cells. Once attached, it can flag the cancer cell for destruction or block signals that help it grow, all while leaving most healthy cells alone.
Your Immune System's Special Forces
Think of your immune system as a well-trained army. It’s fantastic at fighting off common invaders like bacteria and viruses. But cancer cells are clever; they're masters of disguise and can often fly under the radar, evading the army's natural defenses.
This is where monoclonal antibodies (mAbs) come in. They are like a special forces unit, engineered in a lab and programmed with a single, highly specific mission: find a particular target on a cancer cell and neutralize it.
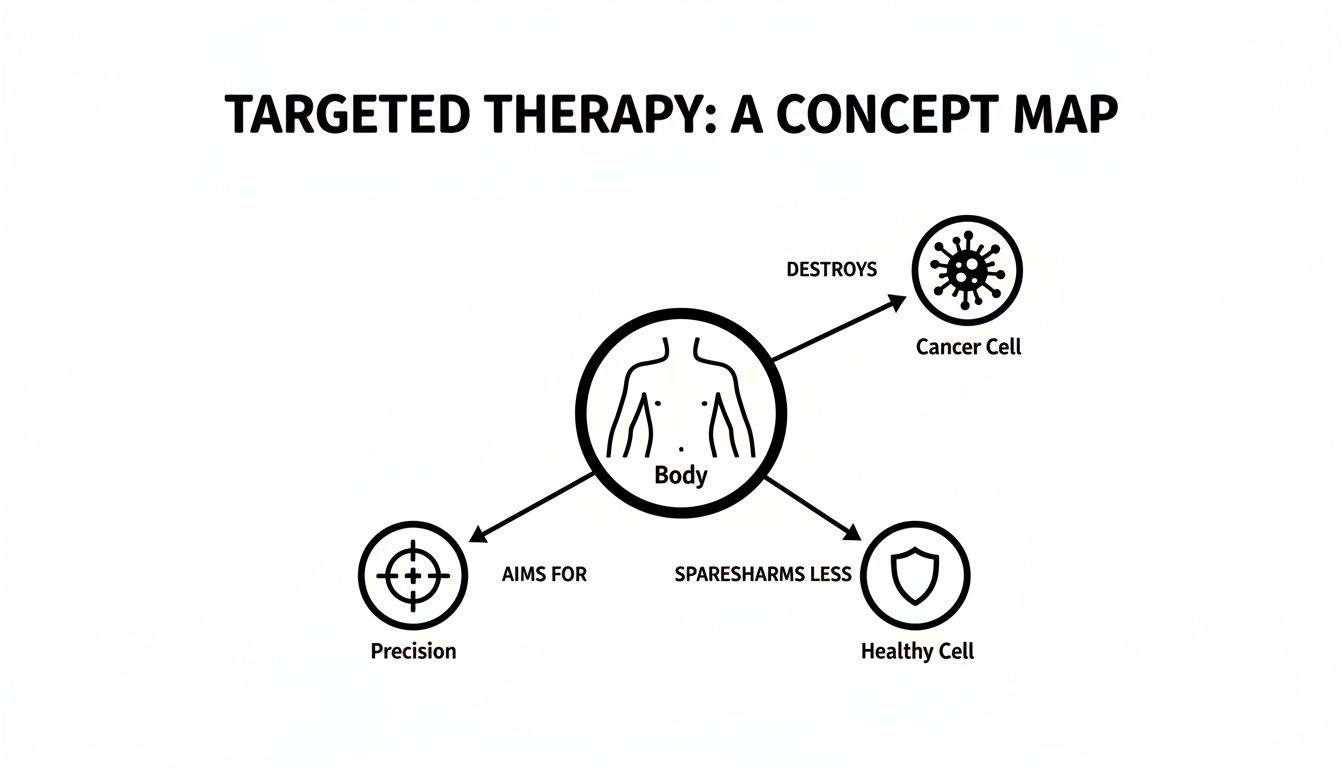
This is a world away from traditional chemotherapy. Chemotherapy is more like carpet bombing—it’s powerful, but it hits both the enemy targets (cancer cells) and the surrounding civilian areas (healthy cells) that happen to be dividing quickly. Monoclonal antibodies, on the other hand, are the precision-guided missiles of cancer therapy. Their accuracy is what makes them a pillar of targeted treatment.
By essentially creating a supercharged version of your body’s own defense proteins, mAbs offer a smarter, more strategic way to fight cancers like pancreatic, colorectal, and breast cancer.
A New Era in Cancer Treatment
The idea of using targeted antibodies has completely changed the field of oncology. The whole journey kicked off when the first monoclonal antibody was approved by the FDA back in 1986 to prevent organ transplant rejection. That success opened the floodgates for cancer research.
Fast forward to 2023, and the field has grown exponentially. We now have over 100 mAbs approved for use worldwide, with more than 50 designed specifically for cancer treatment in major markets. You can read more about the history and impact of these therapies and see just how far we've come.
This targeted strategy allows oncologists to move beyond a one-size-fits-all approach. Instead of treating "cancer," we can now treat the specific molecular drivers of your cancer, opening doors for patients who may have exhausted standard options.
To really understand the shift, it helps to see monoclonal antibodies and chemotherapy side-by-side.
Monoclonal Antibodies vs Traditional Chemotherapy
This table breaks down the fundamental differences between these two approaches, highlighting why mAbs have become such a cornerstone of modern oncology.
The takeaway is clear: monoclonal antibodies represent a move toward smarter, more personalized cancer care, where treatments are chosen based on the unique biology of a patient's tumor.
The Five Ways Monoclonal Antibodies Fight Cancer
Monoclonal antibodies are incredibly versatile. To really understand how they work, you can't just think of them as a single type of weapon; they're more like a multi-tool, with different attachments designed for very specific jobs. There are five main ways these therapies outsmart and attack cancer cells, each leveraging a unique biological process to stop the disease in its tracks.
The core principle behind all of them is precision. The goal is always to zero in on cancer cells while sparing healthy tissue from collateral damage.
This idea of precision is key. Now, let's get into the specifics of how they actually achieve this.
1. Blocking Critical Cell Signals
Cancer cells are often hooked on specific signals that tell them to grow, divide, and spread. Think of these signals as a stuck accelerator pedal, constantly telling the cell to go faster. Certain monoclonal antibodies are engineered to find the receptors on a cancer cell's surface—the docking stations for these growth signals.
By latching onto these receptors, the antibody acts like a shield, physically blocking the "grow" message from getting through. It’s like putting a boot on the accelerator. Without these constant instructions, the cancer cell’s growth can slow down or stop altogether. A great example of this is Cetuximab, which blocks the epidermal growth factor receptor (EGFR) in some colorectal and head and neck cancers.
2. Delivering Payloads Like a Trojan Horse
Some of the most innovative monoclonal antibodies are what we call Antibody-Drug Conjugates (ADCs). These therapies function like a Trojan Horse, designed to sneak a highly potent dose of chemotherapy or a radioactive particle directly inside a cancer cell.
It’s a three-part system:
- The Antibody: This is the guidance system, programmed to seek out a specific marker found only on cancer cells.
- The Linker: A stable chemical bond connects the antibody to its toxic cargo.
- The Payload: This is a powerful chemotherapy drug, often too toxic to be given to the whole body on its own.
The ADC travels through the bloodstream until the antibody finds and binds to its target. The cancer cell then absorbs the entire package. Only once it's safely inside is the payload released, killing the cell from within. This allows us to hit the tumor with a much higher, more effective dose of medication while dramatically reducing the damage to healthy tissues.
3. Releasing the Brakes on Your Immune System
Cancer cells are masters of disguise and evasion. One of their cleverest tricks is to exploit natural "checkpoints" on our own immune cells. These checkpoints are like safety brakes that stop the immune system from attacking our healthy tissues. Cancer hijacks this system to turn off the very T-cells that should be destroying it.
Immune checkpoint inhibitors are a special type of monoclonal antibody that works by blocking these checkpoints. In essence, they release the brakes on your T-cells, unleashing their natural ability to hunt down and kill cancer.
This approach is different because it doesn't target the cancer cell directly. Instead, it empowers your own immune system to do the job it was built for. Drugs like Pembrolizumab (Keytruda) and Nivolumab (Opdivo) have been game-changers in many cancers by simply "taking the foot off the brake" and letting the immune system fight back.
4. Tagging Cancer Cells for Destruction
Another brilliant strategy is to simply make cancer cells more obvious to the immune system. Some monoclonal antibodies are designed to attach to cancer cells and act like bright red flags, making them impossible for your body’s defenders to miss.
This process, known as immune-mediated cytotoxicity, basically puts a "kick me" sign on the back of every cancer cell. Once a cell is "tagged" by an antibody, it triggers two powerful immune responses:
- Antibody-Dependent Cellular Cytotoxicity (ADCC): Immune cells, like Natural Killer (NK) cells, spot the flag and release toxins that destroy the cancer cell.
- Complement-Dependent Cytotoxicity (CDC): The antibody activates a cascade of proteins in the blood (the complement system) that literally punch holes in the cancer cell's membrane, causing it to rupture.
Rituximab, used to treat certain lymphomas, is a classic example of a monoclonal antibody that excels at marking cancer cells for destruction by the immune system.
5. Starving the Tumor by Stopping Blood Supply
Like any living tissue, tumors need a steady supply of blood to get the oxygen and nutrients they need to grow. To do this, they build their own network of blood vessels in a process called angiogenesis.
Some monoclonal antibodies are designed to starve tumors by cutting off this critical supply line. They target a protein called Vascular Endothelial Growth Factor (VEGF), which is the main signal telling the body to grow new blood vessels. By blocking VEGF, these antibodies stop new vessels from forming around the tumor. This can choke off its access to nutrients, slowing its growth or even causing it to shrink.
Turning Your Own Immune System Into a Weapon
Some monoclonal antibodies work by blocking signals or delivering a payload. But one of the most brilliant strategies is far simpler: it turns your body's own immune system into a precision-guided, cancer-destroying force. This approach doesn't need to carry any toxins or interfere with complex signals. It just has to make cancer cells impossible for your natural defenses to ignore.
Cancer cells are masters of disguise, blending in to avoid being noticed by the immune system. Think of these monoclonal antibodies as a can of bright, fluorescent spray paint. They tag the camouflaged enemy cells, making them light up like a target.

This "tag and destroy" mission is a huge part of modern immunotherapy, and it works through two powerful, related processes.
Recruiting the "Natural Killer" Cells
The first method is a mouthful: Antibody-Dependent Cellular Cytotoxicity (ADCC). Here’s what that really means. Once an antibody latches onto a cancer cell, its "tail" (called the Fc region) acts like a bright red flag.
This flag attracts some of the immune system's most effective first responders, particularly the Natural Killer (NK) cells. When an NK cell spots an antibody-coated cancer cell, it locks on and releases a storm of toxic proteins. These proteins punch holes in the cancer cell’s outer wall, causing it to fall apart from the inside out. The antibody provides the coordinates, and the NK cell delivers the knockout blow.
Setting Off a Protein Chain Reaction
The second process is called Complement-Dependent Cytotoxicity (CDC). Instead of recruiting immune cells, this mechanism activates a group of proteins already floating in your blood, known as the complement system.
Think of it as a domino effect. When a monoclonal antibody tags a cancer cell, it tips over the first domino in the complement system. This triggers a cascade, with proteins quickly assembling into a structure called the Membrane Attack Complex (MAC). The MAC literally drills holes into the cancer cell's surface, causing it to burst.
Together, ADCC and CDC form a powerful one-two punch that uses the built-in strengths of your own immune system to take down cancer.
Real-World Proof: How Rituximab Changed Everything
A classic example of this "tag and destroy" strategy is rituximab, a monoclonal antibody used for certain B-cell lymphomas and leukemias. It targets a protein called CD20, which is found all over the surface of these cancerous B-cells.
When rituximab binds to CD20, it triggers both ADCC and CDC with incredible force. The immune system, which might have been ignoring these cancer cells before, now sees them as an urgent threat and launches an all-out attack.
This approach has been a game-changer. Since its approval in 1997, rituximab has completely reshaped the treatment of non-Hodgkin lymphoma. When added to chemotherapy, it helped improve 5-year survival rates for some lymphomas from around 40% to over 60%.
It's a perfect illustration of just how effective monoclonal antibodies can be. By simply putting a flag on the enemy, they can unleash the natural power of your body's defenses, turning a hidden threat into an unmissable target.
What to Expect on Treatment Day
Knowing the science behind monoclonal antibodies is helpful, but it’s just as important to know what your actual treatment day will look like. Let's walk through what you can expect during an infusion session so you can feel more prepared and at ease.

The entire process is designed with your comfort and safety in mind. Most monoclonal antibodies are given through an intravenous (IV) line, which allows the medicine to enter your bloodstream directly for consistent and effective delivery.
A Step-by-Step Look at Your Infusion
When you arrive at an outpatient center like ours, your care team will get you settled in. One of the first things we often do is give you pre-medications. This isn't the treatment itself, but rather a preparatory step to prevent or lessen any potential reactions. These might include an antihistamine, a steroid, or something to reduce fever.
After your IV is placed, the infusion begins. How long it takes really depends on the specific drug you're receiving. Some infusions are as quick as 30 minutes, while others might last for a few hours. Your care team will always let you know what to expect for your particular therapy.
Throughout the entire infusion, you’ll be in good hands. Your nurses will be monitoring you closely, checking your blood pressure, heart rate, and temperature to make sure everything is going as planned.
What We Need from You
Your voice is a crucial part of the process. You know your body better than anyone, so it’s incredibly important to tell your nurse or doctor right away if you start to feel "off" or notice anything different.
While our experienced staff will be monitoring you constantly, you are the expert on your own body. Speaking up early about any new symptom allows your team to manage it quickly—often, all it takes is slowing down the infusion rate.
Some common signs of an infusion reaction to watch for include:
- Chills or a sudden fever
- Itching, a rash, or hives
- Shortness of breath or wheezing
- Feeling dizzy or faint
- Nausea or a headache
If these reactions happen, they are most likely to occur during your very first infusion and tend to be much less common in later treatments. Your team is fully prepared to handle them. To see how we put this into practice, you can learn more about receiving immunotherapy at Hirschfeld Oncology.
Once the infusion is finished, we'll have you stay for a short observation period. This is just to make sure you’re feeling well before you leave. We'll also give you clear instructions on what to look for over the next day or two and who to contact if any questions or concerns pop up. Our goal is to make every part of your treatment feel clear, supported, and centered on you.
Navigating the Benefits, Risks, and Side Effects
Every effective cancer treatment involves a conversation about its potential benefits and its possible risks. It's a delicate balance. When it comes to monoclonal antibodies, our goal is to give you a clear, honest picture of both sides of that equation, so we can make informed decisions together as a team.
The single biggest advantage of monoclonal antibody therapy is its precision. Think of it as a smart bomb versus a blanket attack. Unlike traditional chemotherapy that can't always tell the difference between a cancer cell and a healthy one, these therapies are designed to hunt for a specific marker on the cancer cell's surface. This focused approach means we can attack the cancer while doing our best to leave your healthy tissues alone, which often translates to fewer of the widespread side effects you might be used to.
Beyond precision, another incredible benefit is the potential for durable, long-term responses. By working with your body's own immune system—either by marking cancer for destruction or by taking the brakes off your T-cells—these treatments can sometimes create a lasting "memory" of the cancer. For patients with advanced or stubborn cancers, this can lead to sustained remissions and a meaningful improvement in quality of life.
Understanding the Potential Side Effects
Now, even though these therapies are targeted, they aren't free from side effects. Because they directly interact with your immune system, the reactions they cause are often immune-related. The important thing to remember is that most of these are very manageable, and our team has deep experience in preventing and treating them.
One of the most common things we watch for is an infusion-related reaction. This usually happens during or right after the treatment, especially with the very first dose. Symptoms can be mild—like a fever, chills, or a rash—or more significant. We monitor you very closely the entire time you're here and can easily manage these reactions by slowing down the infusion or giving you pre-medications.
Other common side effects really depend on the specific job the antibody is doing. These can include:
- Fatigue: This isn't just feeling tired; it’s a deep sense of exhaustion that rest doesn’t always fix. It's very common.
- Skin Issues: Rashes, dry skin, and itching can pop up, especially with antibodies designed to block growth signals on cancer cells.
- Flu-like Symptoms: As your immune system gets revved up, you might experience headaches, muscle aches, or a low-grade fever.
It's crucial to understand that a side effect isn't necessarily a sign that something is wrong. In many cases, it’s an indication that the therapy is successfully engaging your immune system to fight the cancer.
Proactive Management Is Key
The side effect profile of a monoclonal antibody is directly tied to its specific mechanism. An antibody that unleashes the immune system (a checkpoint inhibitor) will have a different set of potential side effects than one that blocks a growth signal. Your oncologist will walk you through exactly what to expect based on the drug you're receiving.
Here at Hirschfeld Oncology, we are big believers in proactive management. We don't just wait for side effects to happen; we work to stay ahead of them. This is a core part of our philosophy and involves:
- Thorough Education: We make sure you and your family know exactly what signs to look for once you get home.
- Preventive Measures: We often use medications before and during your infusion to head off common reactions before they start.
- Open Communication: We've built our practice on trust. We want you to feel comfortable calling us about any new symptom, no matter how small it seems.
Your well-being is our absolute priority. By working closely together, we can navigate your treatment journey, harnessing the incredible power of these therapies while keeping a careful eye on the risks to protect your quality of life.
Is Monoclonal Antibody Therapy the Right Choice for You?
We've covered a lot of ground on the science behind monoclonal antibodies, but it all comes down to one crucial question: could this be the right treatment for you? The answer really gets to the heart of what personalized cancer care is all about. This isn't a one-size-fits-all therapy; it’s a highly targeted approach designed for the specific molecular fingerprint of your cancer.
The decision always starts with a deep dive into your tumor's unique biology. This is where biomarker testing comes in. Think of the proteins, or antigens, on the surface of your cancer cells as specific locks. Monoclonal antibodies are the custom-made keys, engineered to fit only those exact locks.
For instance, a patient whose breast cancer cells have too much of a protein called HER2 might be a great candidate for trastuzumab (Herceptin). That antibody is built to do one thing: find and attach to HER2. If that specific marker isn't there, the key has no lock to open, and the treatment simply won't work. This same principle holds true for many different types of cancer.
A Conversation with Your Oncologist
This is exactly why open, detailed conversations with your oncology team are so important. They’ll use sophisticated tests to create a profile of your tumor, which helps them map out the most effective strategy. It's a careful process of matching the right key to the right lock to give the therapy the highest possible chance of success.
The first step is always understanding your cancer's profile. You can learn more about what molecular testing for cancer involves and how it guides treatment in our detailed guide on the topic.
To help you get the most out of your next appointment, here are a few questions you might want to ask:
- Has my tumor been tested for biomarkers that might make a monoclonal antibody a good option for me?
- If so, which specific antibody would you recommend, and what protein does it target?
- Based on my cancer's profile, how exactly is this therapy supposed to work?
- What are the potential benefits you hope to see, and what specific side effects should I be on the lookout for?
The decision to move forward with monoclonal antibody therapy is always a collaborative one, grounded in a deep understanding of your individual diagnosis. It’s a powerful shift away from treating cancer broadly and toward targeting the very things that make your disease grow.
This highly specific approach can open up a new path forward, especially for patients with advanced or treatment-resistant cancers. By arming yourself with knowledge and asking the right questions, you become an empowered partner in your own care. Your cancer's unique profile holds the clues, and these remarkable therapies may just hold the key.
Frequently Asked Questions About Monoclonal Antibodies
Getting your head around the science is one thing, but it’s the practical, day-to-day questions that really matter when you're considering a new treatment. Let's walk through some of the most common things patients ask us. We want you to feel prepared and confident when you talk with your care team.
These are powerful therapies, and understanding exactly how they fit into your overall cancer care is key.
Can Monoclonal Antibodies Be Used with Other Treatments?
Yes, and they often are. In fact, think of monoclonal antibodies as team players. We frequently use them alongside traditional chemotherapy to create a potent, multi-pronged attack on cancer.
There's a real strategic advantage to this approach:
- A One-Two Punch: The monoclonal antibody can tag or weaken a cancer cell, essentially setting it up for the chemotherapy to come in and deliver the final blow.
- Smarter Delivery: With antibody-drug conjugates (ADCs), we can use the antibody as a guided missile to deliver chemotherapy directly to cancer cells, maximizing its impact while sparing healthy tissue.
- Outsmarting Resistance: Cancers can be stubborn and sometimes learn to resist a single therapy. By combining treatments that work in different ways, we can often overcome that resistance and achieve a better outcome.
This combination strategy lets us fight the cancer from several angles at once, which is often far more effective than relying on a single treatment alone.
How Long Will I Need This Therapy?
There's no single answer to this question—the duration of your therapy is completely personalized. Your treatment plan is built around you.
Your treatment schedule is tailored specifically to you. The goal is always to achieve the best possible outcome while carefully managing your quality of life and minimizing long-term side effects.
Your oncologist will map out a timeline based on a few key things:
- Your Specific Cancer Type: Some cancers simply need longer treatment courses than others.
- How Your Body Responds: We'll be monitoring you closely. If the treatment is working well and the side effects are manageable, we might continue it for quite a while.
- The Specific Drug Itself: Every monoclonal antibody has a well-researched protocol that guides how long it should be given for the best effect.
Are All Monoclonal Antibody Drugs the Same?
Not at all. This is one of the most important things to understand about how monoclonal antibodies work. Each one is an incredibly specific, custom-designed protein. It’s engineered to find and attach to one, and only one, specific target (or antigen).
Think of it like a lock and key. A key designed for a HER2-positive breast cancer cell won’t fit the lock on a cancer cell with an EGFR protein. This is precisely why biomarker testing is essential. We first analyze your tumor to figure out which specific "locks" are present. Only then can we choose the exact "key" that will work against your cancer.
At Hirschfeld Oncology, our focus is on creating personalized treatment plans that use these precise therapies. If you’re wondering whether monoclonal antibody therapy could be an option for you, we encourage you to request a consultation. You can explore your options with our experienced and compassionate team by visiting us at https://honcology.com/blog.





.png)


.png)
.png)




