When you're dealing with stage 4 cancer, you need powerful, intelligent treatments. Immunotherapy is exactly that—it's a way of using your own body's immune system to fight back against cancer.
Instead of bringing in outside forces like chemotherapy drugs, this approach essentially "wakes up" and retrains your internal defense system to recognize and destroy cancer cells that have spread.
How Immunotherapy Fights Advanced Cancer
Think of your immune system as an incredibly sophisticated security force. Its job is to patrol your body and eliminate any threats. But cancer cells are crafty; they've learned how to wear a disguise. They exploit natural "checkpoints" in your body—signals that basically tell your immune cells, "I'm one of you, nothing to see here."
This clever trick allows the cancer to grow and spread completely under the radar, eventually leading to a stage 4 diagnosis. Immunotherapy is the strategy that rips off that disguise.
Rather than attacking the cancer directly, immunotherapy drugs give your immune system's top soldiers—the T-cells—the intel they need to finally see the cancer for what it is: a dangerous intruder that must be eliminated.
Unleashing Your Body's Natural Protectors
This is a complete game-changer in how we approach cancer treatment. We're not just carpet-bombing an area with chemotherapy, hoping to kill more bad cells than good ones. We’re empowering a highly targeted, internal special-ops team to do its job.
The goal is to remove the biological "handcuffs" that cancer has put on your immune system.
By reactivating a patient's own defenses, immunotherapy for stage 4 cancer can create a durable, long-lasting response. We're aiming to turn the body from a passive environment where cancer thrives into an active, hostile one where it can't.
The Main Strategies We Use
This "retraining" isn't a one-size-fits-all process. It comes in a few different forms, each designed to empower your immune system in a unique way. The primary methods include:
- Immune Checkpoint Inhibitors: These are the most common immunotherapy drugs. They work by blocking the "I'm a friend" signals that cancer cells use, effectively taking the brakes off your T-cells so they can attack.
- CAR-T Cell Therapy: This is a more intensive approach where we take your own T-cells out, re-engineer them in a lab to become super-charged cancer hunters, and then infuse them back into your body.
Getting a handle on this core idea is the first step. By tapping into the body’s own incredible power, immunotherapy gives us a sophisticated and often more personalized way to manage stage 4 cancer, offering new hope where it's needed most.
Exploring Different Immunotherapy Treatments
Immunotherapy for stage 4 cancer isn't just one treatment. It's a whole category of different strategies, each with a unique way of nudging your immune system into action. Think of it as a specialized toolkit—each tool has a specific job, and understanding them helps make sense of why your oncologist might recommend one over another.
The most common types of immunotherapy all work on a similar principle: turning your own body into an environment that's hostile to cancer. But how they do it is what makes them different.
Immune Checkpoint Inhibitors: Taking the Brakes Off
Imagine your immune system’s T-cells are like powerful race cars, always revving their engines and ready to hunt down threats. To keep them from causing chaos by attacking healthy tissue, they’re equipped with powerful brakes called checkpoints. Cancers are devious; they've learned how to slam on these brakes, effectively stopping T-cells right in their tracks.
Immune checkpoint inhibitors are drugs that block this from happening. They don’t press the gas pedal—they just take the T-cell’s foot off the brake. This simple action allows the immune system to finally "see" the cancer as an invader and launch the attack it was always meant to.
This class of drugs has been a major breakthrough in treating many advanced cancers. By disabling the "stop" signal cancer sends, checkpoint inhibitors unleash the pre-existing power of a patient's immune system.
Drugs targeting the PD-1, PD-L1, and CTLA-4 pathways are common checkpoint inhibitors. They've become a go-to first-line treatment for several stage 4 cancers, including certain lung cancers and melanomas.
CAR-T Cell Therapy: Creating Super Soldiers
While checkpoint inhibitors work with the T-cells you already have, Chimeric Antigen Receptor (CAR)-T cell therapy is much more hands-on. It’s like pulling your best soldiers out of the field, sending them to a special ops training facility, and arming them with high-tech gear to hunt a very specific enemy.
It’s a highly personalized process that works like this:
- Collect: We start by collecting a patient's own T-cells from their blood.
- Re-engineer: In a specialized lab, these T-cells are genetically modified to produce new receptors on their surface, called CARs. These receptors are custom-built to recognize and latch onto a specific protein (an antigen) found only on the patient’s cancer cells.
- Multiply: The newly engineered CAR-T cells are grown into an army of millions.
- Infuse: Finally, these "super soldiers" are infused back into the patient's bloodstream, where they can now seek and destroy cancer cells with incredible precision.
This approach has been a game-changer for blood cancers, and researchers are actively working on ways to apply it to solid tumors as well.
Cancer Vaccines: A Proactive Training Program
When you hear "vaccine," you probably think of preventing illnesses like the flu. Therapeutic cancer vaccines work differently—they are designed to treat an existing cancer. Their whole purpose is to train the immune system to recognize and attack cancer cells by showing it what to look for.
Think of it as giving your immune system a "most wanted" poster of the cancer cell. By introducing a harmless piece of the tumor (an antigen), the vaccine teaches T-cells what their target looks like. This helps the immune system build a long-term memory, preparing it to hunt down and eliminate any cell that displays that specific marker.
Cytokine Therapy: Sounding the Alarm
Cytokines are the proteins that act as messengers for your immune system, coordinating the body's response to threats. In cancer treatment, giving a patient high doses of lab-made cytokines is like sounding a five-alarm fire bell throughout the body, rallying every available immune cell to the fight.
This is one of the older forms of immunotherapy. While it can be effective for certain cancers like melanoma and kidney cancer, its powerful, system-wide activation can also cause significant side effects. For that reason, newer, more targeted therapies are often preferred, but cytokine therapy still has its place.
Each of these methods offers a different way to engage the immune system. Below is a simple table to help visualize how they compare.
Comparing Common Immunotherapy Approaches
This table provides a simplified overview of the main immunotherapy types, their mechanisms, and how they are typically administered for advanced cancers.
Understanding this spectrum of available treatments is a key part of your journey. You can learn more about how specialists approach immunotherapy at Hirschfeld Oncology for a deeper look into personalized care in the NYC area.
Which Cancers Respond Best to Immunotherapy?
Immunotherapy has been a game-changer for treating stage 4 cancer, but its success isn't the same across the board. The effectiveness really depends on the unique characteristics of the cancer itself.
Think of it like a lock and key. Some cancer "locks" are a perfect fit for an immunotherapy "key," unlocking a powerful and lasting response. Others, however, are built differently and are more resistant. This isn't a failure of the treatment; it's a reflection of biology.
Cancers that tend to have a lot of genetic mutations, like melanoma and certain lung cancers, often produce more abnormal proteins. These proteins act like little red flags, making it much easier for a re-energized immune system to spot and attack the cancer cells.
On the flip side, some cancers are considered "cold" tumors. They are masters of disguise, creating an environment that actively shuts down immune cells or simply doesn't have enough red flags to trigger an alarm. Figuring out where a specific cancer falls on this "hot" to "cold" spectrum is a crucial first step in deciding if immunotherapy is the right path.
Cancers with Strong Responses to Immunotherapy
Some stage 4 cancers have become the poster children for immunotherapy's potential, showing incredible and durable responses where older treatments offered very little hope.
- Melanoma: Advanced melanoma was one of the very first cancers where we saw profound benefits from checkpoint inhibitors. For patients with metastatic melanoma, these drugs have completely rewritten the rules on survival expectations.
- Non-Small Cell Lung Cancer (NSCLC): This is another area where immunotherapy is now a cornerstone of treatment. For patients whose tumors express high levels of a protein called PD-L1, immunotherapy can be even more effective than chemotherapy.
- Kidney Cancer (Renal Cell Carcinoma): Immunotherapy, often paired with targeted therapy, has become a standard first-line treatment for advanced kidney cancer, leading to significantly better outcomes.
- Bladder Cancer: Checkpoint inhibitors are now a key part of the treatment plan for metastatic bladder cancer, especially for patients who can't tolerate traditional chemotherapy.
These successes are often tied to specific biomarkers that help predict who will benefit most, a topic we’ll dive into a bit later.
The Success Story in Stage 4 Lung Cancer
Immunotherapy has dramatically changed the outlook for patients with stage 4 non-small cell lung cancer (NSCLC), a diagnosis that historically came with a very poor prognosis. The introduction of immune checkpoint inhibitors has led to major breakthroughs.
For instance, in advanced NSCLC patients with high PD-L1 expression (≥50%), a key drug has shown a 5-year overall survival rate of 23.2%, a huge leap from the 15.5% for those treated with chemotherapy alone. When combined with chemo, even patients with low PD-L1 benefit; some trials have reported a pathological complete response rate of 25.3% with the combination, versus just 4.7% with chemotherapy.
Cancers with More Variable or Limited Responses
While the breakthroughs are exciting, it's just as important to be realistic about where immunotherapy is still an evolving science. For some of the most difficult stage 4 cancers, a positive response is often limited to a smaller subset of patients who have very specific genetic markers.
Pancreatic and Biliary CancersThese cancers are notoriously tough to treat and are often classic "cold" tumors. They build a dense, fibrous wall around themselves that immune cells struggle to break through. However, there's hope: a small percentage of these patients with a biomarker known as MSI-high have shown good responses to immunotherapy, which underscores why comprehensive tumor testing is so vital.
Colorectal CancerThe story of immunotherapy in stage 4 colorectal cancer is a perfect illustration of personalized medicine. For the vast majority (around 85%) of patients whose tumors are "microsatellite stable" (MSS), checkpoint inhibitors have shown very little benefit on their own.
But for the 15% with microsatellite instability-high (MSI-H) tumors, the results can be truly extraordinary. In this specific subgroup, immunotherapy isn't just an option—it's often the best treatment. You can learn more about how our specialists approach treatment for colon cancer in our detailed guide.
It's not about the cancer's location, but its genetic signature. A colorectal cancer with an MSI-High status may have more in common with an MSI-High uterine cancer than it does with a typical MSS colorectal cancer when it comes to immunotherapy response.
Breast and Ovarian CancerFor a long time, these weren't considered immunotherapy-responsive cancers. That’s starting to change. For triple-negative breast cancer, combining immunotherapy with chemotherapy has been approved for patients whose tumors express PD-L1. In ovarian cancer, research is moving quickly, but for now, responses are seen in a smaller group of patients, often those with specific genetic profiles.
This all points to a critical shift in cancer care. Immunotherapy for stage 4 cancer is moving away from a one-size-fits-all model and toward a highly personalized strategy, driven by the unique biology of your tumor.
Using Biomarkers to Personalize Your Treatment
Immunotherapy isn't a one-size-fits-all solution. Its success hinges on understanding the unique biological signature of a tumor, and that's where biomarkers come in. Think of biomarkers as clues or signposts on cancer cells that reveal whether your immune system can be effectively rallied to fight them.
By testing for these markers in your tumor tissue, we can move beyond a generalized approach and tailor a treatment plan specifically for you. These results don't just predict if a therapy is likely to work; they also help us sidestep treatments that won't, saving you precious time and unnecessary side effects. It’s all about finding the right key for the right lock.
Decoding PD-L1 Expression
One of the first biomarkers we look for is PD-L1, which stands for Programmed death-ligand 1. The simplest way to think about PD-L1 is as a "don't attack me" flag that cancer cells wave to fool your immune system. When your T-cells see this flag, they stand down, mistaking the tumor for a normal part of your body.
If your tumor shows high levels of PD-L1, it means the cancer is relying heavily on this disguise to survive. This is often great news for a type of immunotherapy called checkpoint inhibitors. These drugs essentially block the PD-L1 signal, ripping off the cancer's camouflage and exposing it to your immune system's attack. A high PD-L1 score is often a strong indicator that you’ll respond well to these drugs.
Identifying Genetic Instability with MSI-H and dMMR
Another crucial set of biomarkers is MSI-H (microsatellite instability-high) and dMMR (deficient mismatch repair). These are telltale signs that a tumor's internal DNA repair machinery is broken. Because the cancer cells can't fix their genetic mistakes, they accumulate a massive number of mutations.
While that sounds dangerous, it's actually a huge advantage for immunotherapy. All those mutations lead to abnormal proteins, which act like bright red flags that make the cancer cells look incredibly foreign to your immune system. A tumor with an MSI-H or dMMR status is practically screaming for attention, making it a prime target once your immune system is unleashed.
Biomarkers like MSI-H have turned immunotherapy into a game-changer for certain colorectal, gastric, and endometrial cancers that were historically very tough to treat. It's a perfect example of how a cancer's genetic profile can be more important than where it started in the body.
The following infographic helps visualize how different biomarker profiles can influence the response to immunotherapy.
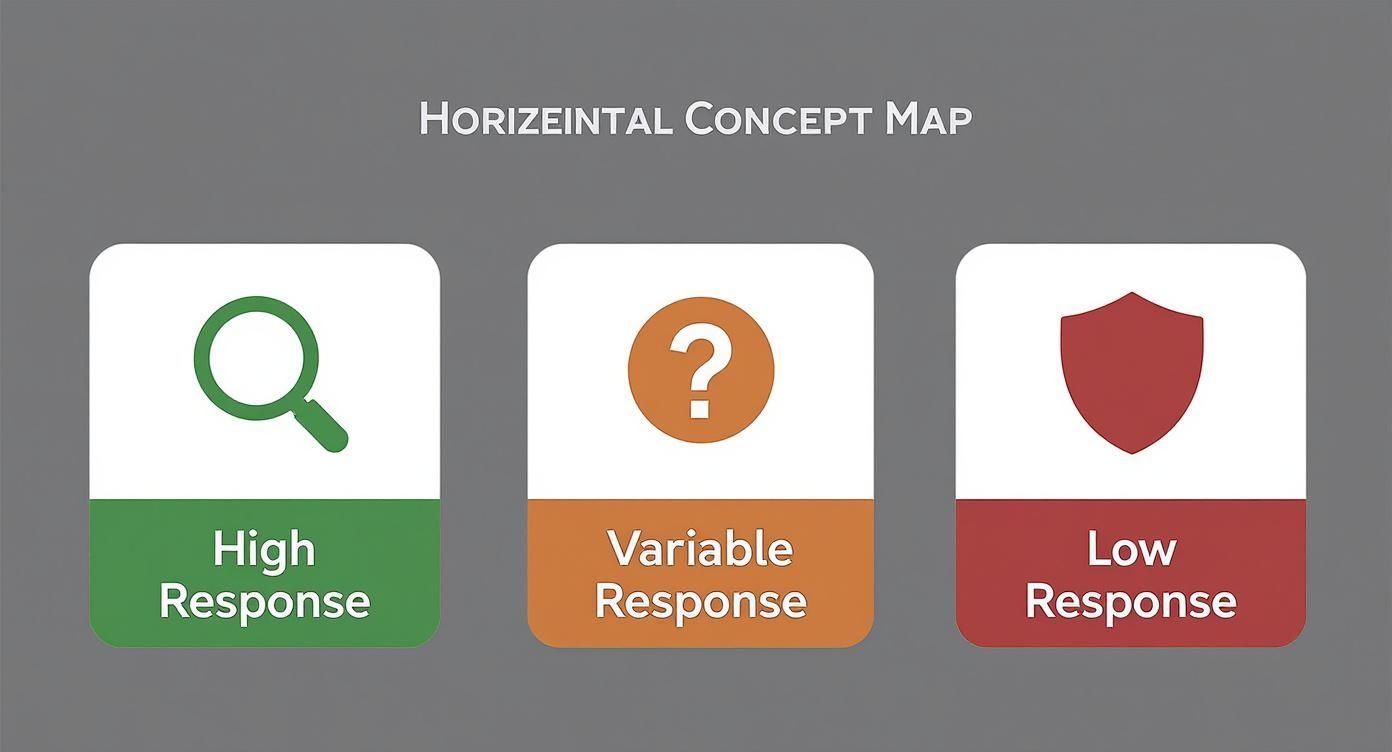
As you can see, tumors with lots of mutations (like those with MSI-H) are far more likely to trigger a strong response, while others might need a different strategy.
Measuring Tumor Mutational Burden (TMB)
A third key biomarker, Tumor Mutational Burden (TMB), gives us a direct count of the total number of mutations within a cancer cell's DNA. Just like with MSI-H, a high TMB means the tumor is churning out lots of unusual proteins. These proteins, called neoantigens, are what your immune system can be trained to recognize and destroy.
While PD-L1, MSI-H, and TMB are the most established biomarkers today, the field is always advancing, with new markers being discovered all the time. These tests give us the data we need to build a truly personalized treatment plan, sometimes combining immunotherapy with other powerful approaches. To see how this compares with other precision treatments, you can read our guide to targeted therapy.
Understanding your tumor's biomarkers is the critical first step in harnessing the full power of immunotherapy for your fight.
Navigating Immunotherapy Side Effects

While immunotherapy is a game-changer for stage 4 cancer, its unique approach brings a very different set of side effects than what you might expect from chemotherapy. These issues don't come from the drug itself, but from the very thing that makes it work: a newly supercharged immune system.
I often tell my patients to think of their immune system like a guard dog we've just woken up. Its main job is to go after the cancer, but sometimes, in its newfound enthusiasm, it can start barking up the wrong tree and mistakenly go after healthy tissues. This friendly fire causes inflammation, which we call immune-related adverse events (irAEs).
In an interesting way, seeing some mild side effects can actually be a good sign. It tells us your immune system is awake and responding to the treatment. The key, of course, is keeping that response targeted on the cancer and not on you.
Understanding Common irAEs
Because your immune system has access to every part of your body, irAEs can pop up in almost any organ. The good news is that most are mild to moderate and very manageable, especially when we catch them early. This is why open and constant communication with your oncology team is so important.
Here are some of the most common things we see:
- Skin Reactions: A rash, itching, or dry skin is often one of the first things patients notice. It’s very common but usually handled well with simple creams or oral medications.
- Fatigue: This isn't just feeling a little tired; it's a profound sense of exhaustion. Pacing yourself and letting your doctor know how you're feeling is crucial.
- Gastrointestinal Issues: Inflammation in the digestive tract can lead to diarrhea or colitis. You must report these symptoms right away, as they can become serious if we don't get them under control.
- Endocrine Problems: Sometimes, the immune system can target glands that produce hormones, like the thyroid or pituitary gland. This might mean you'll need hormone replacement therapy to get things back in balance.
How We Manage Side Effects
Early detection is everything. Your care team will monitor you closely, but you are the most critical person on that team. It is absolutely vital that you report any new or unusual symptom, no matter how minor it seems.
The core principle of managing immunotherapy side effects is to temporarily suppress the overactive immune response without completely shutting down its cancer-fighting activity. Your vigilance in reporting symptoms allows us to do this effectively.
For something simple like a minor rash, a topical steroid cream might be all it takes. For more serious inflammation like colitis, we might prescribe oral steroids such as prednisone to calm the immune system down.
In some situations, we may need to press pause on your treatment to give your body a chance to recover. The goal is always to strike a balance where the therapy is tough on the cancer but easy on you, allowing you to stay on this powerful treatment for as long as it's working.
Essential Questions to Ask Your Oncologist
When you’re facing a stage 4 cancer diagnosis, the conversations with your medical team are everything. It’s easy to feel overwhelmed, but walking into those appointments prepared can make all the difference. Having a solid list of questions ready helps you become an active partner in your own care.
Think of your oncologist as your most critical ally on this journey. The goal isn’t just to follow instructions, but to build a partnership where you truly understand the “why” behind every decision. These questions are designed to start that conversation and make sure all your bases are covered when considering immunotherapy.
Understanding Your Personal Treatment Plan
First things first: you need to know if immunotherapy is even on the table for you. The answer to that question comes down to the specific biology of your cancer.
- Is immunotherapy a realistic option for my type of stage 4 cancer? Ask for the reasoning—what does the current clinical evidence say?
- What did my biomarker tests (like PD-L1, MSI-H, or TMB) show? Have your doctor walk you through how these results point toward—or away from—immunotherapy.
- What are we hoping to achieve with this treatment? Get a clear picture of the potential outcomes. Are we talking about shrinking the tumor, keeping it stable, or achieving long-term control?
- What are the biggest risks and most common side effects? This is essential for weighing the potential benefits against the day-to-day impact on your quality of life.
Navigating the Practical Details
Once you understand the "why," it's time to get into the "how." Knowing the logistics of treatment can take a huge amount of stress and uncertainty out of the equation, letting you plan your life around your care.
An effective treatment plan is one that you can realistically follow. Asking about the practical side of care—scheduling, monitoring, and side effect management—is just as important as understanding the science behind it.
Here are a few practical questions to get you started:
- What will the treatment schedule actually look like? How often will I need to come in for infusions, and how long do they usually take?
- How will we know if it’s working? Discuss the timeline for your first follow-up scans and what a "good result" would look like.
- What’s our game plan for managing side effects? Be proactive. Ask who you should call—and when—if you start feeling unwell, even if it's in the middle of the night.
- What's our plan B? It's always a good idea to ask what comes next if the immunotherapy doesn't work as well as we hope, or if side effects become unmanageable.
Exploring Clinical Trials and Future Options
For many people with advanced cancer, clinical trials aren't a last resort; they're a gateway to the next wave of promising treatments.
- Are there any immunotherapy clinical trials that could be a good fit for me? This lets your oncologist know you're open to exploring every possible avenue.
- If this treatment eventually stops working, what else is on the horizon? The field is moving incredibly fast. Knowing what other immunotherapy options might be available down the road can offer a real sense of hope and direction.
These conversations form the very foundation of personalized cancer care. By asking thoughtful, detailed questions, you empower yourself and become a true partner in your treatment. If you’re in the New York City area and looking for an expert opinion on immunotherapy for stage 4 cancer, our team at Hirschfeld Oncology is ready to provide in-depth consultations to help you find your path forward.
Common Questions About Immunotherapy
When you're facing a stage 4 cancer diagnosis, exploring a treatment like immunotherapy brings up a lot of questions. That’s completely normal. Getting clear answers is the first step toward feeling in control and ready for what’s ahead. Let's walk through some of the practical things patients often ask.
How Long Will I Need Immunotherapy Treatment?
This is one of the most common questions, but there's no single, straightforward answer. The duration of your immunotherapy is entirely based on your individual situation.
Several key factors come into play: your specific type of cancer, the particular drug you're receiving, and—most importantly—how your cancer responds. How you feel and manage any side effects is also a big part of the equation.
For some people who see a fantastic, lasting response, we might discuss pausing treatment after a set period, often around two years. For others, the therapy might continue as long as it's working and the side effects are manageable. Your oncologist will map out a starting plan and continually adjust it based on your progress.
Can I Receive Immunotherapy With Other Treatments?
Absolutely. In fact, combining treatments is now a cornerstone of fighting many stage 4 cancers. For several advanced cancers, like certain lung or bladder cancers, pairing immunotherapy with chemotherapy is the standard of care because it simply works better.
Think of it as a powerful one-two punch. The chemotherapy can kill cancer cells, and as those cells break down, they release signals (called tumor antigens) that the immune system can see. This process basically shines a spotlight on the cancer, making it much easier for the newly-unleashed immune system to find and destroy any remaining cancer cells.
Combining therapies is all about creating synergy. We use the strengths of one treatment to amplify the effectiveness of another, aiming for an outcome that is greater than the sum of its parts. This is a core principle of modern cancer care.
Your oncologist will look at your specific diagnosis and biomarkers to figure out if a combination approach is the right call for you.
Does Immunotherapy Cure Stage 4 Cancer?
In oncology, we use the word "cure" very carefully, especially when talking about stage 4 disease. That said, immunotherapy has completely changed the game. For a small but growing number of patients, it has led to incredible, long-term remissions where the cancer disappears and doesn't come back for years.
In most cases, the immediate goal of immunotherapy for advanced cancer is to turn it into a manageable, chronic condition. We aim for durable control, giving you more time and preserving your quality of life. For some, immunotherapy has achieved a complete response, offering a kind of hope that was hard to imagine just a decade ago.
At Hirschfeld Oncology, we focus on creating treatment plans that bring the latest cancer science directly to you. If you're looking into immunotherapy for stage 4 cancer in the NYC area, we’re here to offer an expert consultation and talk through what makes sense for your unique situation. You can read more on our blog.





.png)


.png)
.png)




