When you or a loved one receives a cancer diagnosis, the first step is often trying to make sense of the treatment options. The core difference between targeted therapy and chemotherapy is quite simple: chemotherapy is a broad approach that attacks all fast-growing cells, while targeted therapy is a precision treatment that zeroes in on cancer cells based on their specific genetic makeup.
Charting Your Cancer Treatment Path
Choosing the right path forward means getting a solid handle on how each treatment actually works. For decades, chemotherapy has been a foundational tool in oncology. Think of it as a powerful, system-wide attack on cancer. It travels throughout your body, killing cells that divide quickly—a classic trait of cancer cells, but unfortunately, also a trait of healthy cells in places like your bone marrow, digestive tract, and hair follicles.
Targeted therapy, on the other hand, is a much more modern and precise strategy. These drugs are engineered to interfere with specific molecules, or "targets," that are essential for the cancer's growth and survival. It’s like having a key designed to fit a very specific lock found only on the cancer cells, leaving most of your healthy cells alone.
This fundamental difference is what shapes everything from treatment eligibility to potential side effects and overall effectiveness. The move from broad-stroke chemotherapy to these more precise options has been a game-changer. In just the last few years, the FDA has approved around 40 new targeted therapies across 12 different cancer types, completely changing the outlook for patients whose tumors have identifiable genetic drivers. To see how far we've come, it's worth taking a look at the history of cancer chemotherapy and how these treatments have evolved.
To really nail down the differences between these two powerful approaches, let's break them down side-by-side.
Quick Comparison: Targeted Therapy vs Chemotherapy
This table offers a snapshot of the key distinctions, helping you see at a glance how these treatments stack up.
This comparison is just the starting point for the targeted therapy vs chemotherapy conversation. While one is a powerful, time-tested tool and the other a highly specialized instrument, both are critical in today's cancer care. In many cases, the best treatment plans actually use them together—either in combination or one after another—all based on the specifics of your diagnosis.

How Each Treatment Fights Cancer

To really get to the heart of the targeted therapy vs chemotherapy discussion, you have to understand how each one actually works inside the body. They aren't just two slightly different drugs; they're two fundamentally different strategies for fighting cancer. One is a powerhouse of overwhelming force, while the other is more of a precision strike.
Chemotherapy's entire game plan is built around one of cancer's defining features: its cells divide and multiply at a frantic, uncontrolled pace. Chemo drugs are cytotoxic agents—they are designed to be toxic to cells, especially those caught in the act of splitting. This broad, powerful attack is why chemotherapy has been a pillar of cancer care for decades.
The problem is, this method is powerful but not very discriminating. It’s like casting a giant net to catch one specific kind of fish; you’ll get your target, but you’ll also haul in a lot of other things you weren't aiming for. The drugs travel throughout the body and attack any rapidly dividing cell they come across.
The Broad Reach of Chemotherapy
While cancer cells are the main target, plenty of healthy cells in your body also divide quickly as part of their normal function. This collateral damage is what causes chemotherapy's most notorious side effects.
Cells that often get caught in the crossfire include:
- Hair Follicles: These cells grow constantly, which is why chemotherapy often leads to hair loss.
- Bone Marrow: This disrupts the factory that makes new blood cells, leading to fatigue (from low red blood cells), a higher risk of infection (from low white blood cells), and easy bruising (from low platelets).
- Lining of the Digestive Tract: The constant turnover of these cells is interrupted, causing nausea, mouth sores, and diarrhea.
Chemotherapy’s mechanism is a double-edged sword. Its power to kill rapidly dividing cells makes it a lifesaver against many aggressive cancers. But its lack of specificity is also its biggest drawback, causing systemic side effects that can take a toll on a patient's quality of life.
Even with its limitations, chemotherapy remains an indispensable tool. Oncologists have become much better at managing its side effects. For some patients, options like low-dose chemotherapy from Hirschfeld Oncology can strike a better balance, aiming to control the cancer with a more tolerable impact on the body.
The Precision of Targeted Therapy
Targeted therapy is playing an entirely different ballgame. Instead of attacking all fast-growing cells, it zeroes in on specific molecules—the internal machinery—that a cancer cell needs to grow, spread, and survive. Think of it less like a net and more like a smart key cut to fit a unique lock found only on or inside cancer cells.
These "locks" are typically proteins or genetic mutations that act like faulty on/off switches, constantly telling the cancer cell to multiply. Targeted therapies are designed to find these specific molecular targets and jam the lock. This precision is the defining difference in the targeted therapy vs chemotherapy matchup.
These drugs have several clever ways of accomplishing their mission:
- Blocking Growth Signals: Some drugs, like tyrosine kinase inhibitors (TKIs), get inside the cell and block the signals that scream "grow and divide!" A classic example is the use of drugs that shut down the EGFR mutation in certain non-small cell lung cancers.
- Cutting Off Blood Supply: Tumors are hungry and need their own blood supply to grow—a process called angiogenesis. Certain targeted drugs, called angiogenesis inhibitors, stop the formation of new blood vessels, essentially starving the tumor.
- Delivering Toxins Directly: In another smart approach, a targeted drug acts like a homing missile, carrying a payload of poison directly to cancer cells while largely ignoring healthy ones.
Because targeted therapy is so specific, its side effects are usually quite different from chemo's. Instead of widespread issues like hair loss and fatigue, the side effects often relate directly to what the drug is targeting. This might mean skin rashes, diarrhea, or changes in blood pressure. It's a much more focused approach and represents a major evolution in cancer treatment.
How These Treatments Perform in the Real World
Ultimately, the best cancer treatment is the one that works. When we compare targeted therapy and chemotherapy, we're not just looking at a tumor on a scan. We're talking about extending lives, improving the quality of those lives, and achieving responses that last. Chemotherapy is still a powerful, broad-spectrum weapon and remains the best choice for many cancers, but targeted therapy has completely rewritten the rulebook for specific groups of patients.
If a patient's tumor has a specific molecular "switch" we can flip, a targeted drug can produce incredible results. We've seen this time and again in certain lung cancers. For example, patients with non-small cell lung cancer (NSCLC) that has an EGFR mutation often see a much better response and live longer without their cancer progressing when treated with a targeted inhibitor compared to traditional chemotherapy.
This same idea applies across many different cancers, creating a clear difference in outcomes that all comes down to the tumor's specific biology.
Where Targeted Therapy Really Shines
The wins for targeted therapy are most dramatic in cancers fueled by a single, dominant genetic flaw. In these situations, the treatment can be incredibly effective because it cuts off the cancer's primary growth signal right at the source.
Kidney cancer, or renal cell carcinoma (RCC), is a perfect example. Studies have shown that for the right patients, targeted therapy leads to better survival. One analysis found that RCC patients treated with targeted therapy had a higher one-year survival rate (55% vs. 49%) and a median survival that was 3.0 months longer than those who didn't receive it. You can learn more about these survival findings in renal cancer in the published research.
This drives home a critical point: for the right patient, targeted therapy isn't just another option—it's a life-extending one.
For patients with specific biomarkers, like HER2-positive breast cancer or BRAF-mutated melanoma, targeted therapies have turned what were once dire prognoses into manageable long-term conditions. The power to shut down the specific engine driving the cancer can lead to rapid tumor shrinkage and a noticeable improvement in symptoms. This gives patients not just more time, but better quality time.
Why Chemotherapy Is Still a Cornerstone of Cancer Care
With all the excitement around targeted drugs, it’s easy to think chemotherapy is obsolete, but that’s far from the truth. For a huge number of cancers, chemotherapy is still the most effective treatment available, especially for tumors that don't have a known, "targetable" mutation.
Many cancers aren't driven by one simple genetic mistake but by a complex mess of mutations. In those cases, chemotherapy's broad-based attack is far more likely to work than a drug aimed at a single target. It also remains the go-to option when a targeted therapy stops working, which is a common problem known as acquired resistance.
The Constant Challenge of Treatment Resistance
No treatment is a permanent fix for every patient. Cancer is smart and can figure out ways to get around both targeted drugs and chemotherapy.
- Targeted Therapy Resistance: A tumor might develop a new mutation that switches a growth pathway back on, or it might find a completely different pathway to fuel its growth, making the original drug useless.
- Chemotherapy Resistance: Cancer cells can become experts at pumping chemo drugs out before they cause harm or learn to quickly repair the DNA damage the drugs are designed to create.
This reality is why the conversation about targeted therapy vs. chemotherapy almost always evolves into a discussion about strategy. An oncologist might start with a targeted drug, then switch to chemotherapy if the cancer becomes resistant. Sometimes, we even use them together to hit the cancer from multiple angles at once, trying to stay one step ahead of its next move.
Navigating Side Effects and Quality of Life

When we talk about targeted therapy vs chemotherapy, the conversation inevitably turns to side effects. But this isn't just about listing potential symptoms; it's a deeply personal discussion about quality of life during treatment. How each therapy affects your body is a direct result of how it fights cancer.
Chemotherapy's broad-spectrum approach often leads to body-wide effects, while targeted therapy's precision creates a more specific—but no less significant—set of challenges. Understanding these differences is the first step in preparing yourself, both mentally and physically, for what lies ahead. It allows us to build a proactive plan to manage symptoms and protect your well-being.
The Systemic Impact of Chemotherapy
Think of chemotherapy as a systemic treatment—it travels through your entire bloodstream. Its side effects stem directly from its inability to distinguish between a cancer cell and any other rapidly dividing healthy cell in your body. This is what we call "collateral damage."
Because of this, many patients experience a familiar set of issues as the treatment affects healthy tissues in the gut, hair follicles, and bone marrow.
- Profound Fatigue: This is more than just feeling tired. Affecting up to 80% of patients, it’s a debilitating exhaustion driven by the body's immense effort to repair healthy tissue and, often, by anemia from a low red blood cell count.
- Nausea and Vomiting: While modern anti-nausea medications have come a long way, more than 70% of patients still grapple with these symptoms as the chemo irritates the sensitive lining of the digestive tract.
- Hair Loss (Alopecia): A well-known side effect, this happens simply because hair follicles are some of the fastest-growing cells in the body, making them an unintentional target.
- Increased Risk of Infection: Chemo suppresses bone marrow, which is the factory for our immune cells. This lowers the white blood cell count, leaving patients more vulnerable to bacteria and viruses.
These side effects can build up over time, sometimes becoming more intense with each cycle. Managing them is a core part of cancer care, involving careful medication timing, lifestyle tweaks, and constant communication with your oncology team.
"The experience of chemotherapy is often defined by its systemic nature. The goal of supportive care is to anticipate these body-wide effects and intervene early, ensuring patients can tolerate and complete their full treatment course with the best possible quality of life."
The Specific Side Effects of Targeted Therapy
Targeted therapies work on a completely different principle, and so do their side effects. These drugs are designed to interfere with specific molecular pathways that fuel a tumor's growth. The side effects, then, are often a direct result of that specific pathway being blocked.
This precision means you can often avoid the classic chemo side effects like total hair loss or severe bone marrow suppression. But it introduces its own set of challenges. For instance, drugs targeting the EGFR pathway—a key driver in some lung and colorectal cancers—also hit EGFR proteins in the skin. The result? A very common and sometimes severe acne-like rash. While challenging, it's also a sign the drug is hitting its target.
Common targeted therapy side effects include:
- Skin Problems: Rashes, intense dryness, and changes to fingernails and toenails are very common with certain drug classes.
- Diarrhea: Some therapies disrupt the lining of the gut, causing persistent diarrhea that requires active management to prevent dehydration.
- High Blood Pressure (Hypertension): Drugs that choke off a tumor's blood supply (angiogenesis inhibitors) can also constrict blood vessels elsewhere, leading to a rise in blood pressure.
- Liver Issues: Since the liver processes many of these drugs, it can become inflamed. We monitor this closely with regular blood tests.
It's a common misconception that "targeted" automatically means "milder." The side effects are different, but they can still significantly affect your day-to-day life. For a deeper dive, you can learn more about managing targeted therapy side effects in our detailed guide.
Side by Side Comparison of Common Effects
Seeing the different side effect profiles laid out can make the trade-offs between targeted therapy vs chemotherapy much clearer. The following table highlights the common impacts you can expect from each approach.
Side Effect Profile Chemotherapy vs Targeted Therapy
Ultimately, the goal is to find a treatment that not only works against the cancer but also works for you as a person. An honest conversation with your oncologist about potential side effects and your own priorities is the cornerstone of a truly personalized cancer care plan.
Determining Your Eligibility for Treatment
Deciding between targeted therapy and chemotherapy isn't a matter of simple preference. It's a decision rooted in the very biology of your cancer. The first and most important question your oncologist needs to answer is this: does your tumor have a specific, identifiable vulnerability that a targeted drug can attack? Answering that is the first step toward a genuinely personalized treatment plan.
Chemotherapy's eligibility is, by comparison, quite broad. Because it goes after all rapidly dividing cells—a hallmark of most cancers—it can be used across a wide range of cancer types without needing a specific molecular trigger. It remains a powerful, often essential, tool in our arsenal, especially when a tumor doesn't have an identifiable target.
Targeted therapy, on the other hand, is like a key that only fits a specific lock. This is why biomarker testing is the absolute gateway to figuring out if this approach is right for you. These tests aren't just routine; they are a form of molecular detective work.
The Role of Biomarker Testing
Biomarker testing means we analyze a sample of your tumor tissue or sometimes your blood (what we call a liquid biopsy). We're searching for specific genetic mutations, overexpressed proteins, or other molecular flags that are fueling the cancer’s growth. These biomarkers tell us, in no uncertain terms, whether a particular targeted drug is likely to hit its mark.
Some of the most common biomarkers we look for include:
- EGFR mutations in non-small cell lung cancer
- ALK rearrangements, also found in lung cancer
- BRAF mutations in melanoma
- HER2 protein overexpression in breast and stomach cancers
If your tumor tests positive for one of these markers, it completely changes the game. For instance, a woman diagnosed with breast cancer will have her tumor tested for its HER2 status. If it's HER2-positive, we can bring in drugs like trastuzumab (Herceptin) to specifically shut down that protein's activity. This single piece of information transforms her entire treatment plan and prognosis.
The presence of a single biomarker can completely alter the therapeutic strategy. It shifts the entire conversation from a broad, systemic treatment like chemotherapy to a precise, molecularly guided one. This is why comprehensive genomic testing has moved from being a niche practice to a true standard of care in modern oncology.
Navigating Eligibility in the Real World
While the science sounds straightforward, the reality of who is eligible for these treatments is a bit more nuanced. The development of targeted drugs has been a monumental step forward, offering incredible outcomes for the right patients. For example, in patients with metastatic lung cancer driven by an EGFR mutation, the targeted drug osimertinib has pushed the median survival to nearly 39 months.
But it’s important to have a realistic perspective: not every patient has a targetable mutation. In 2018, it was estimated that only about 8.3% of the 610,000 U.S. patients with advanced cancer were eligible for a targeted therapy based on their biomarkers. You can explore more about the impact of targeted therapies on cancer care to see how these numbers reflect the ongoing challenges and progress in the field.
That statistic drives home a critical point: for the majority of patients, chemotherapy isn't a "lesser" choice—it is the most effective and appropriate one. When a tumor lacks a known target, chemotherapy’s foundational ability to attack rapidly dividing cells remains our strongest line of defense. Ultimately, the decision in the targeted therapy vs. chemotherapy debate comes down to the unique genetic signature of your cancer.
How Doctors Combine and Sequence Treatments
When we talk about targeted therapy vs. chemotherapy, it’s rarely a simple choice of one over the other. Think of modern cancer care as a dynamic, evolving strategy. Your treatment plan isn't set in stone; it's designed to adapt to your cancer's unique biology and how it responds over time.
Oncologists are constantly thinking several moves ahead to control the disease. The goal is always to use the right tool at the right time, creating a carefully orchestrated sequence to maximize effectiveness at every stage of your cancer journey.
Common Sequencing and Combination Strategies
A common approach is to lead with targeted therapy. If biomarker testing shows a specific vulnerability—like an EGFR mutation in lung cancer—starting with a targeted drug can deliver a powerful, rapid response with fewer of the widespread side effects we see with chemo.
This strategy is often the first line of attack until the cancer eventually develops resistance, which unfortunately can happen. Once the targeted drug loses its effectiveness, your oncologist might pivot to a chemotherapy regimen to hit the cancer from a completely different angle.
Another powerful tactic is to use chemotherapy first. This is often done to quickly shrink a large tumor, a process called debulking. Once the initial threat is under control, a targeted therapy can be introduced as maintenance therapy.
The purpose of maintenance therapy isn't necessarily to wipe out every last cancer cell, but to keep any remaining microscopic disease in check. This can dramatically delay a cancer's return and extend remission, helping to manage an aggressive disease almost like a chronic condition.
This infographic shows the typical decision-making path that determines whether a patient starts with targeted therapy or another option like chemotherapy.
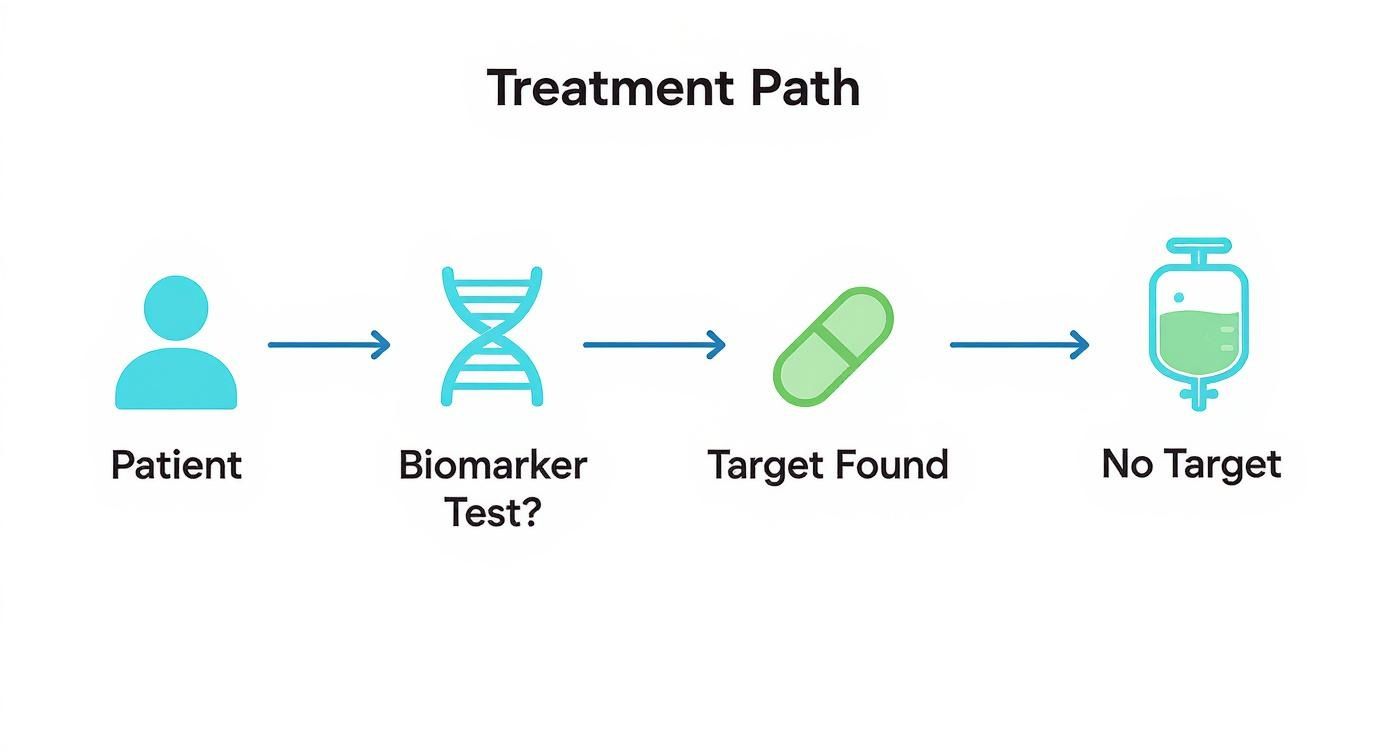
As the visual shows, biomarker testing is the critical fork in the road. Finding a specific target is what unlocks a precision-based approach.
Creating a Truly Personalized Plan
Sometimes, the best plan involves using both therapies at the same time. Combining a targeted drug with chemotherapy can produce a synergistic effect, where the two treatments together are more potent than either one alone. In some cases, the targeted agent weakens the cancer cells, making them more vulnerable to the chemotherapy.
This decision hangs on a few key factors:
- The cancer type and stage: Certain cancers have a known history of responding well to combination approaches right from the start.
- Your overall health: Your oncologist needs to determine if you're strong enough to handle a more intensive combination regimen.
- Your specific biomarkers: The tumor's genetic profile is the ultimate guide for which, if any, targeted drugs are on the table.
Ultimately, your treatment path is deeply personal. It’s a continuous cycle of treating, monitoring, and adjusting based on the latest science and your specific health needs.
Common Questions About Cancer Treatment
When you're facing cancer, you and your family will naturally have a lot of questions. As you start to look at different paths like targeted therapy or chemotherapy, getting straight answers is the first step toward making a confident decision with your oncologist. Here are a few of the most frequent questions we discuss with our patients.
Is Targeted Therapy Always a Better Choice?
Not at all. The best treatment is always the one that’s right for your specific cancer and its unique biology. If a tumor has a very specific genetic mutation that we can hit with a particular drug, then yes, a targeted therapy can be remarkably effective and often comes with more manageable side effects.
But if your cancer doesn't have one of those specific "targets," then chemotherapy often remains the most powerful and proven tool in our arsenal. It’s all about matching the right treatment to the job at hand, based on solid biomarker testing and clinical evidence.
The most effective treatment isn't about what's newest; it's about what's scientifically matched to your tumor's biology. This is the heart of personalized cancer care today.
Can I Switch from One Treatment to Another?
Absolutely. Switching treatments is a normal and often planned part of a cancer care strategy. We might recommend a change if your cancer develops acquired resistance and stops responding to the current therapy.
It's also possible that a new blood test—what we call a liquid biopsy—reveals a new mutation that has developed, opening the door for a different targeted drug. Your treatment plan isn't set in stone; it's a dynamic road map that we adjust based on how the cancer evolves and how you're feeling.
How Do Doctors Know if a Treatment Is Working?
We use a combination of tools to get the full picture. Regular imaging, like CT or PET scans, gives us a clear look at whether tumors are shrinking, stable, or growing. We also use blood tests to track specific tumor markers, which can tell us how much cancer activity is happening in the body.
Just as importantly, we listen to you. How you feel and whether your symptoms are getting better is a critical part of the puzzle. This blend of objective data and your personal experience tells us if we’re on the right track. For anyone about to begin chemotherapy, taking some time to learn how to prepare for chemotherapy can also make the process feel much more manageable.
At Hirschfeld Oncology, we believe that clear communication is key to good care. If you're looking into advanced cancer treatment options in the New York City area, please reach out. We're here to schedule a consultation and talk through a plan that’s built just for you. You can learn more at https://honcology.com/blog.





.png)


.png)
.png)




