When you’re going through chemotherapy, the last thing you want to worry about is a complicated diet. The best place to start is with simple, gentle, nutrient-dense foods that are easy on your system. Think of food as a key part of your support team—things like lean proteins, soft fruits, and well-cooked vegetables can help you keep your strength up and handle treatment side effects.
Navigating Your Chemotherapy Diet With Confidence
Starting treatment is a lot to handle, and figuring out what to eat can feel like just one more thing on a very long list. Instead of getting bogged down in rules, try to see your nutrition as a powerful ally. Your body is doing some incredibly hard work right now, and the food you eat is the fuel it needs to heal, fight off infection, and stay as strong as possible.

It helps to think about your diet having three main jobs:
- Keeping Up Your Strength and Energy: Getting enough calories and protein is crucial to prevent muscle loss and keep you from feeling completely drained.
- Supporting Your Immune System: The right vitamins and minerals give your body the tools it needs to defend itself when it’s most vulnerable.
- Managing Side Effects: The right food choices can make a real difference in soothing common issues like nausea, mouth sores, or changes in taste.
Being proactive about what you eat can genuinely improve your quality of life during treatment. The physical toll of chemo is no joke, and it often leads to a dip in diet quality and key micronutrient deficiencies. In fact, one study found that the intake of essential nutrients like calcium, iron, vitamin C, and zinc was alarmingly low for many patients. You can read more about the research into post-chemotherapy nutrient inadequacy to understand the full picture.
Your Foundational Food Groups
Getting started doesn't have to be complex. The goal isn't perfection; it's about making small, smart choices every day that add up. Thinking about these core food groups is also a key step in getting ready for your treatment. For more on this, our guide on how to prepare for chemotherapy has some great additional tips.
Here’s a quick rundown of what to focus on and why it helps.
Quick Guide to Chemotherapy-Friendly Food Groups
This isn't a rigid plan, but a flexible framework. The most important thing is to listen to your body and adapt your meals based on how you feel each day. This way, nutrition becomes a source of empowerment, not stress, in your cancer care journey.
Using Protein to Rebuild and Recover
Picture your body during chemotherapy as a construction site working overtime. Protein is the crew's most crucial material—the bricks, mortar, and steel beams needed to repair and rebuild healthy cells, maintain your strength, and keep your immune system in fighting shape. If you run short on these supplies, the whole recovery process can grind to a halt.
Many people find their appetite for protein-rich foods takes a nosedive during treatment, but making it a priority is one of the best things you can do for yourself. This isn't just about feeling stronger; it's about handing your body the fundamental tools it needs to get through therapy and bounce back.
Why Protein Becomes Your Priority
During chemo, your body's demand for protein skyrockets. The treatment is designed to attack rapidly dividing cells—which, unfortunately, includes not just cancer cells but also healthy ones in your mouth, digestive tract, and hair follicles. Protein is what your body uses to patch up that damage, helping you heal more effectively between infusions.
But that’s not all it does. Getting enough protein is also critical for:
- A Stronger Immune System: Your immune system needs protein to manufacture the antibodies and white blood cells that protect you from infections.
- Keeping Your Muscle: Chemotherapy can often lead to muscle loss, which is a major reason people feel so exhausted. Protein helps you hold onto that muscle, preserving your strength and energy.
- Balancing Fluids: Proteins play a key role in keeping fluids where they belong, which can help prevent uncomfortable swelling (edema) in your hands, feet, and ankles.
The research really drives this point home. One study found that consuming less than 1.0 gram of protein per kilogram of body weight per day was the single biggest nutritional factor linked to more intense fatigue and worse outcomes. Because of this, most experts now recommend aiming for 1.0–1.5 g/kg/day. You can read more about these important findings on protein intake during chemo.
Finding Your Best Protein Sources
The trick here is to find protein sources that are easy to eat and gentle on your system. Some days, a simple piece of baked chicken might sound great. On other days, the very idea of meat can be a turn-off. It’s all about having a variety of options ready so you can roll with whatever your body is telling you. For a comprehensive list of ideas, take a look at our guide on the best foods for chemotherapy patients.
Here are some fantastic choices to have in your kitchen:
Animal-Based Proteins (Often easier for your body to absorb):
- Poultry: Think skinless chicken or turkey—baked, poached, or even shredded into a comforting soup.
- Fish: Mild, flaky fish like cod, tilapia, or haddock are usually well-tolerated. Fatty fish like salmon is also a great choice for its anti-inflammatory omega-3s.
- Eggs: Scrambled, hard-boiled, or folded into an omelet. Eggs are soft, easy to prepare, and packed with nutrition.
- Dairy: Greek yogurt, cottage cheese, and milk are simple, no-cook options. If you have trouble with dairy, lactose-free versions work just as well.
Plant-Based Proteins (Perfect for days when meat just won't do):
- Legumes: Lentils, chickpeas, and black beans are wonderful in soups and stews. You can also mash them into dips like hummus.
- Tofu and Tempeh: These soy-based foods are soft, incredibly versatile, and great at soaking up the flavors of whatever you cook them with.
- Nuts and Seeds: Smooth nut butters are easy to spread on toast or crackers. Ground seeds can be blended right into smoothies for an invisible protein boost.
Remember, the goal is consistency, not perfection. A little bit of protein with each meal and snack is far more effective than trying to eat one large, protein-heavy meal when you’re not feeling up to it.
Simple swaps can make all the difference. Try stirring a scoop of unflavored protein powder into oatmeal, mashed potatoes, or soups. Keep hard-boiled eggs and single-serving Greek yogurts in the fridge for a quick snack that requires zero effort. By weaving these foods into your day, you give your body that steady supply of building blocks it needs to stay strong and recover.
Managing Treatment Side Effects Through Smart Food Choices
Chemotherapy is an incredibly powerful treatment, but the side effects can feel like a battle in themselves. The great news? Your kitchen can be one of your strongest allies. By being strategic about what you eat, you can directly tackle common discomforts and get back a sense of control over how you feel.
Think of food as more than just fuel; it's a tool for comfort. Just as you’d grab a cool cloth for a fever, you can use certain foods to soothe an upset stomach or ease a sore mouth. This approach lets you respond to what your body is telling you in the moment, making a real difference in your day-to-day comfort.
When you're dealing with a mix of symptoms, it can be tough to know where to start. The following table breaks down common side effects and offers simple, practical food swaps to help you feel better.
Symptom-Specific Food Strategies
Think of this table as your quick-reference guide. Keep it handy on your phone or fridge so you can easily adapt your meals based on how you’re feeling that day.
Taming Nausea And An Upset Stomach
Nausea is easily one of the most challenging side effects, but you can often find relief with some simple dietary changes. The goal is to stick with foods that are bland, plain, and easy on your system. Anything too greasy, spicy, or heavy is likely to make a queasy stomach feel much worse.
When that feeling hits, reach for one of these:
- Dry and Salty: Plain crackers, toast, or pretzels can be incredibly calming. They are easy to get down, even when you have zero appetite.
- The BRAT Diet: This classic combination—Bananas, Rice, Applesauce, and Toast—is famous for a reason. It’s gentle and effective.
- Soothing Teas: A warm cup of ginger or peppermint tea has natural properties that can help settle your stomach.
"Listen to your body. If a full meal sounds overwhelming, switch to small, frequent snacks. Keeping your stomach from getting completely empty is a great trick to keep nausea from creeping in."
These small moves can make a huge impact. For a more detailed look, our guide on managing fatigue and nausea during cancer therapy offers even more practical tips.
Soothing Painful Mouth Sores
Mouth sores can turn eating into a painful chore, but the right food choices will help you stay nourished without adding to the pain. The strategy here is simple: choose foods that are soft, cool, and non-irritating.
Try to focus on foods with a smooth texture:
- Cool and Creamy: Yogurt, cottage cheese, smoothies, and milkshakes are fantastic. The cool temperature alone can be incredibly soothing.
- Soft and Simple: Think scrambled eggs, mashed potatoes, and creamy soups that are easy to swallow with minimal chewing.
- Hydrating Fruits: Go for soft fruits like melon, bananas, or applesauce. Stay away from citrus fruits like oranges or grapefruit, as their acid will sting.
You’ll also want to steer clear of anything crunchy, sharp, or spicy—like chips, raw vegetables, or hot sauce—that can scrape or irritate sore spots.
Overcoming Changes In Taste
It's deeply frustrating when your favorite foods suddenly taste wrong. A persistent metallic taste is a common complaint that can make eating feel like a chore, but you can fight back with a few kitchen tricks.
If you're dealing with that metallic flavor, give these a shot:
- Ditch the Metal: Using plastic or bamboo utensils instead of metal forks and spoons can make a surprising difference.
- Add a Little Tartness: A squeeze of lemon or lime in your water or on fish and chicken can help cut through that metallic flavor.
- Cleanse Your Palate: Chewing on sugar-free mints, ginger candies, or gum can refresh your mouth and mask the unpleasant taste for a while.
Sometimes the issue isn't a bad taste, but almost no taste at all. If that’s the case, don't be shy about adding more flavor. Experiment with bold herbs, spices, and marinades to make your food more interesting. This simple flowchart can also help when certain foods, like meat, just don't sound good anymore.
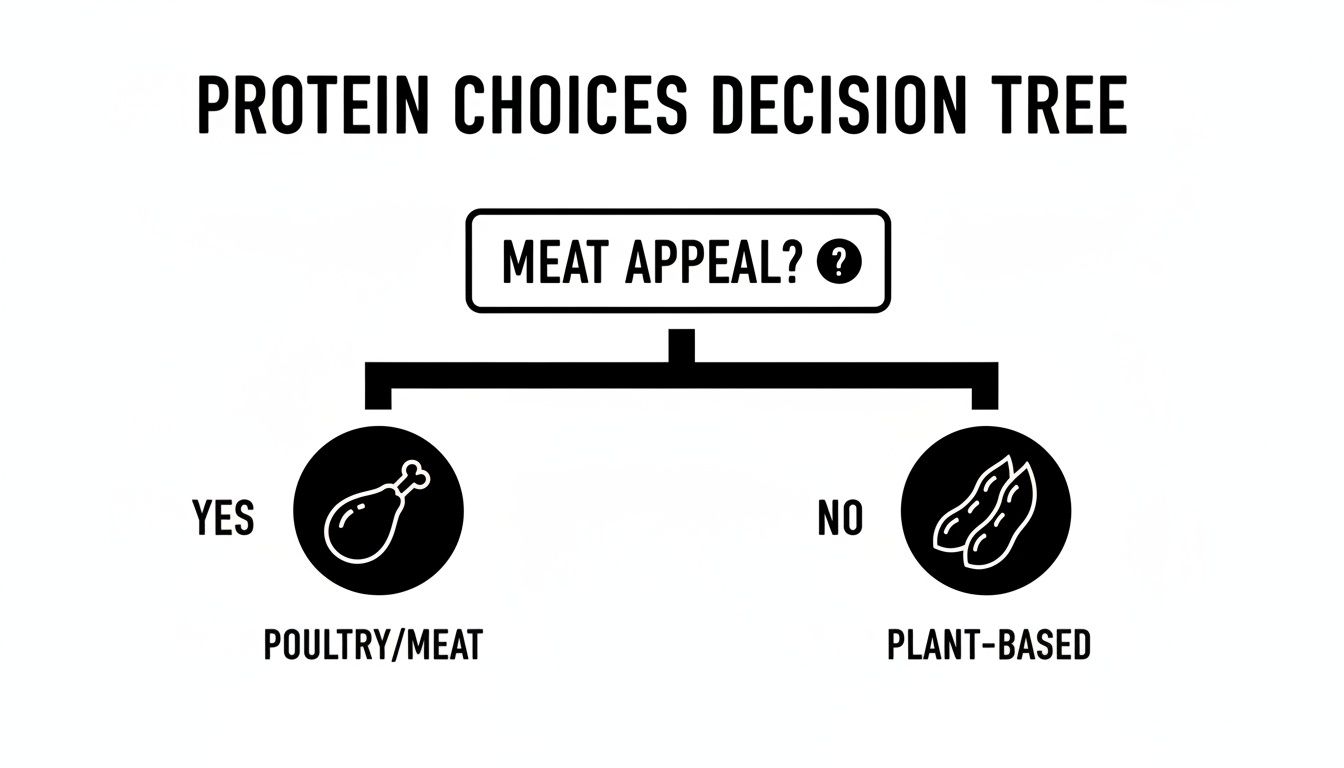
As the chart shows, if meat has lost its appeal, plant-based proteins are an excellent alternative to make sure you’re still getting what your body needs. Finding what works for you is a process of trial and error, but with these strategies, you're much better equipped to navigate it one meal at a time.
Mastering Food Safety When Your Immune System Is Low
Chemotherapy is a powerful tool, but it can temporarily weaken your body's defenses. One of the common side effects is a drop in white blood cells, a condition called neutropenia, which leaves your immune system vulnerable.
Think of your immune system as your body's personal security detail. During chemo, some of that team is temporarily off-duty, which means you have to be extra vigilant about germs—especially the ones that can sneak in through your food. This doesn't mean you need to be afraid of eating. It just means adopting a few smart, simple habits in the kitchen to keep yourself safe and well-nourished.
The Four Pillars of Safe Food Handling
By building these four simple practices into your daily routine, you can create a powerful defense against foodborne illness when you need it most.
Clean: This one is non-negotiable. Wash your hands thoroughly with soap and warm water for at least 20 seconds before you touch any food and again after you finish. Give all your fruits and vegetables a good rinse under running water, even if you plan on peeling them. Bacteria on the outside can easily transfer to the inside when you cut into it.
Separate: Cross-contamination is a major culprit in food poisoning. Keep raw meat, poultry, seafood, and eggs completely separate from foods that are ready to eat. A simple way to do this is by using different cutting boards—one for raw proteins and another for everything else.
Cook: The only way to know for sure that food is cooked to a safe temperature is by using a food thermometer. Color is not a reliable indicator. For example, all poultry needs to reach an internal temperature of 165°F (74°C), while ground meats should hit 160°F (71°C).
Chill: Bacteria love to grow at room temperature. Get perishable foods into the refrigerator within two hours of buying or cooking them. And when it's time to thaw something, do it safely in the fridge, under cold running water, or in the microwave—never on the countertop.
This quick reference chart from the FDA is a great visual reminder of these crucial steps.
These aren't complicated rules, but together, they form a rock-solid foundation for keeping your food safe while your immune system is recovering.
Foods That Require Extra Caution
While safe handling is your best defense, some foods naturally carry a higher risk. When your immunity is low, it’s wise to temporarily steer clear of these items.
The goal here isn’t to create a long list of forbidden foods. It's about making smart, temporary swaps to choose the safest path while your body is focused on healing.
Here are the main foods to be mindful of during your treatment:
- Raw or Undercooked Proteins: This means saying no to sushi, raw oysters, steak tartare, and eggs with runny yolks for now.
- Unpasteurized Products: Always check labels to make sure milk, cider, and juices are pasteurized. Soft cheeses made from raw milk, like some types of brie, feta, or queso fresco, should also be avoided.
- Deli Counter Meats and Salads: Freshly sliced deli meats and prepared salads (like potato or macaroni salad) can be a source of listeria. Opt for pre-packaged lunch meats instead, and always heat them until they are steaming hot before eating.
- Raw Sprouts: Alfalfa, mung bean, and other raw sprouts can be contaminated with bacteria that are hard to wash off. It's best to skip them entirely.
- Untested Well Water: If your home uses well water, make sure it's tested regularly. Otherwise, it’s much safer to stick with bottled or filtered water for drinking and cooking.
Following these guidelines can dramatically lower your risk of picking up an infection, allowing you to put all your energy where it belongs: on getting better.
Why Hydration Is More Than Just Drinking Water
Staying hydrated during chemotherapy is absolutely fundamental, but it’s about so much more than just drinking glass after glass of water. Think of fluids as your body's essential clean-up crew. They're constantly at work, helping to flush out the byproducts of treatment and other waste. Getting enough fluids is one of the most powerful things you can do to fight off that deep-seated fatigue, keep constipation at bay, and give your kidneys the support they need to process strong medications.

But let's be realistic. When you're feeling nauseous or your appetite has vanished, forcing down plain water can feel like a monumental task. The great news is you don’t have to. Plenty of other liquids and even certain foods can help you meet your hydration goals, often while delivering some much-needed calories, electrolytes, and comfort along the way.
Expanding Your Hydration Toolkit
The trick is to think beyond the water bottle. Your body is craving a constant, gentle supply of fluids, and there are countless ways to provide it. On days when solid food just isn't an option, these hydrating alternatives can become a lifeline.
Try working some of these into your day:
- Soothing Broths: A warm mug of bone broth or a simple vegetable broth isn't just hydrating; it's deeply comforting. It also helps replace sodium and potassium—key electrolytes that are easily depleted by side effects like diarrhea or vomiting.
- Herbal Teas: You can’t go wrong with ginger or peppermint tea for an unsettled stomach. Chamomile is wonderful for helping you relax. Whether you like them warm or iced, they offer gentle, caffeine-free hydration.
- Diluted Juices: Sometimes full-strength juice can be overwhelmingly sweet. Try cutting it with water (half and half is a good start). Apple or cranberry juice are often good choices that provide a hint of flavor and a few calories.
A key piece of advice: Aim to sip fluids consistently all day long instead of trying to chug large amounts all at once. Just keeping a drink within arm's reach makes it so much easier to stay on top of your needs without feeling overwhelmed.
When Your Fluids Need to Be Food
There will be days when chewing feels like too much work or a sore mouth makes it painful. This is when you can lean on nutrient-rich liquids to pull double duty, providing both hydration and calories. These options are kind to your digestive system and easy to get down.
Here’s how to turn your drinks into a meal:
- Protein-Packed Smoothies: These are a game-changer. Blend a soft fruit like a banana with some Greek yogurt or a scoop of unflavored protein powder and your choice of milk (or a non-dairy alternative like almond milk). It’s an incredibly efficient way to get protein, vitamins, and calories in a form that’s easy to swallow.
- Creamy Soups: Thin, pureed soups feel like a warm hug. Think butternut squash, tomato, or cream of mushroom. You can easily enrich them by blending in some soft-cooked carrots, beans, or even a swirl of cream or coconut milk for extra calories.
When you start to see hydration as a flexible, creative part of your nutrition plan, it becomes much easier to give your body what it needs. Every sip, whether it's from a comforting cup of tea or a nourishing smoothie, is a small victory that supports your strength and recovery.
Common Questions About Your Chemotherapy Diet
It's completely normal to have a lot of specific questions pop up as you go through chemotherapy. Even with a solid nutrition plan, day-to-day realities can bring new challenges. Let's tackle some of the most common questions we hear from patients, so you can feel more confident about your food choices.
Should I Take Vitamins or Supplements?
This is a big one, and the short answer is: be extremely careful. It is absolutely critical to run every single vitamin, herb, or supplement by your oncology team before you take anything. What seems like a harmless health booster can sometimes cause serious problems.
For example, high-dose antioxidants, like vitamins C and E, can potentially interfere with how chemotherapy does its job. The best and safest route is to get your vitamins and minerals directly from whole foods. Your doctor will only suggest a supplement if a blood test shows a specific deficiency that needs correcting. Otherwise, let food be your medicine.
Think of it this way: your chemo is a very precise instruction for your cells. You don't want supplements sending a different, conflicting message that could weaken your treatment's impact. Always let your medical team have the final say.
What Are Some Easy Snack Ideas for Low-Appetite Days?
When you have zero appetite, a full plate of food can feel like a mountain you just can't climb. The trick is to forget about three big meals a day. Instead, think about small, frequent, and nutrient-packed snacks. The goal is just to get something in your system every couple of hours to keep your energy up.
Having ready-to-go options within arm's reach is a game-changer. Here are a few simple ideas:
- A handful of almonds or walnuts
- A single-serving cup of Greek yogurt or cottage cheese
- One hard-boiled egg (keep a few pre-peeled in the fridge)
- A slice of whole-wheat toast with a smear of avocado or nut butter
- A cheese stick with a few crackers
- A small smoothie made with protein powder
Keeping these things stocked and visible makes it so much easier to fuel your body, even when you really don't feel like it.
Is It Safe to Drink Alcohol During Treatment?
For most people undergoing chemo, the answer is a firm no. Oncologists usually advise steering clear of alcohol entirely, and for good reason. Alcohol can make common side effects like dehydration and mouth sores much worse. It also puts extra strain on your liver, which is already working overtime to process all the chemotherapy drugs.
On top of that, alcohol can interact poorly with other medications you might be taking, leading to potentially harmful reactions. If you have a special occasion and are thinking about having even one drink, you must ask your doctor first. They are the only ones who can say whether a small amount is safe with your specific treatment plan.
How Do I Handle the Metallic Taste in My Mouth?
Ugh, that metallic taste. It’s a frustratingly common side effect known as dysgeusia, and it can make your favorite foods taste completely off. Thankfully, a few simple tricks can help you fight back.
Give these strategies a try:
- Switch Your Utensils: Ditch the metal forks and spoons for a bit. Using plastic, bamboo, or wooden utensils can make a surprisingly big difference.
- Embrace Tart Flavors: A little bit of tartness can cut right through that metallic flavor. Try squeezing lemon or lime into your water or using citrus marinades for chicken and fish.
- Cleanse Your Palate: Sucking on sugar-free mints, ginger chews, or lemon drops between meals can help mask the taste and refresh your mouth.
It might take a little trial and error to see what works for you, but these tips can offer real relief.
At Hirschfeld Oncology, we believe that personalized care extends to every aspect of your well-being, including nutrition. If you have more questions or are exploring advanced treatment options, our team is here to provide the expert guidance and compassionate support you deserve. To learn more or request a consultation, please visit us at https://honcology.com/blog.





.png)


.png)
.png)




