For many people navigating cancer treatment, a high-quality whey protein isolate is often a top recommendation. It's packed with leucine for muscle repair, absorbs quickly, and is very low in lactose. But everyone's journey is different, and what works for one person may not work for another, especially with varying treatment side effects. That's why talking it over with your care team is always the first step.
Why Protein Becomes a Critical Ally in Cancer Care
When you're fighting cancer, your body is working overtime. Imagine your body as a house caught in a relentless storm—that storm being the cancer and its treatments. Protein is the lumber, nails, and concrete needed to constantly repair the damage, rebuild healthy cells, and keep the structure strong.
This intense physical stress dramatically increases your body's protein requirements, pushing them far beyond the standard recommendations for a healthy person. Your body is simply demanding more of these essential amino acids to keep up.
The Increased Demand for Cellular Repair
Cancer treatments are designed to attack fast-growing cancer cells, but they often can't tell the difference between a cancer cell and a healthy one. This collateral damage means your body has a massive repair job on its hands.
Protein provides the raw materials to:
- Heal Tissues: It helps rebuild everything from the sensitive lining of your gut to your skin and hair follicles.
- Support Immune Function: Your immune system relies on protein to create the antibodies and white blood cells that fight off infections—a common risk during treatment.
- Produce Enzymes and Hormones: These are the messengers that regulate metabolism and keep countless bodily functions running smoothly.
This is why nutrition experts often recommend a much higher protein intake during cancer therapy. Research shared by Moffitt Cancer Center, for instance, suggests that patients may need 1.2 to 1.5 grams of protein per kilogram of body weight each day. That’s nearly double the standard guideline. Meeting this target is directly linked to better tissue repair and a stronger immune response. You can learn more about these protein findings.
"During cancer treatment, protein isn't just about food; it's a strategic part of your therapy. Meeting these heightened needs is fundamental to improving treatment tolerance, preserving strength, and supporting your body’s ability to heal."
Combating Muscle Wasting and Fatigue
One of the toughest challenges during cancer treatment is a condition called cachexia, which is a severe and often rapid loss of muscle. It’s more than just weight loss; it’s a metabolic crisis where the body starts breaking down its own muscle tissue for energy. This leads to extreme fatigue, weakness, and can make it harder to tolerate treatments.
Getting enough protein is your number one defense against this. It supplies the essential amino acids—especially leucine—needed to protect and rebuild that precious muscle mass.
Unfortunately, side effects like nausea, a poor appetite, or mouth sores can make eating a full meal feel like an impossible task. This is where the right protein powder can be a game-changer. It offers a concentrated, high-quality dose of protein that’s often much easier to get down than a plate of chicken or beans, making it a powerful and practical tool in your nutritional toolkit. To dive deeper, you can learn more about managing cancer-related cachexia in our detailed guide.
Picking the Right Protein Powder For You
Walking down the supplement aisle can feel overwhelming, especially when you’re already juggling so much with cancer treatment. The labels, the different types, the claims—it's a lot. But the goal here is simple: find a protein that fits your body's needs right now.
The first big question is usually dairy or no dairy. Your personal tolerance, any allergies, and even your taste preferences will point you in the right direction. There's no single "best" choice for everyone; what matters is what works for you.
This little decision tree can help you find your starting point.
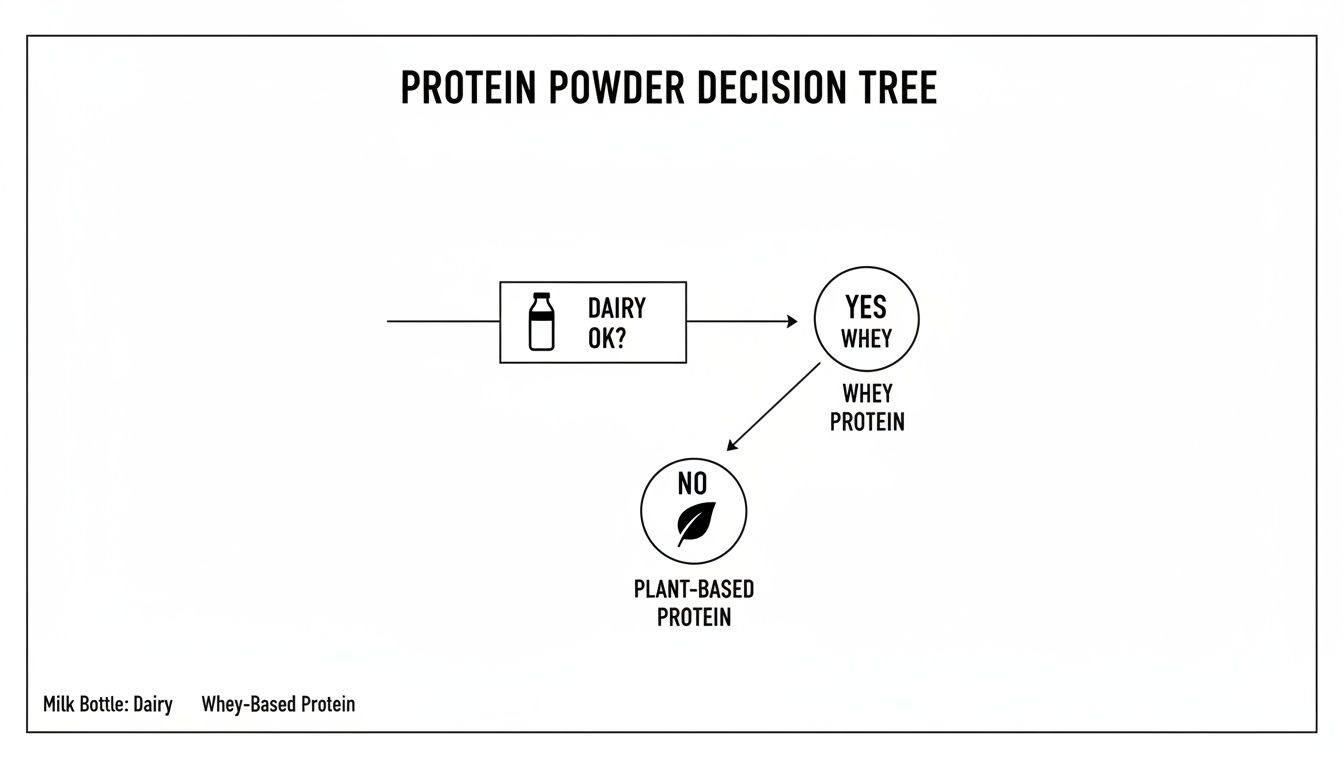
Think of this as step one. Can your system handle dairy right now? If yes, whey is a fantastic option. If not, the plant-based world has plenty of excellent choices waiting for you.
The Gold Standard: Dairy-Based Proteins
For most people who can tolerate dairy, whey protein is the go-to for a reason. It’s a complete protein, which means it packs all nine of the essential amino acids your body needs but can't make itself. It's especially rich in an amino acid called leucine, which is like the master switch for kickstarting muscle repair.
But not all whey is the same. Two types are particularly helpful for people going through cancer treatment:
- Whey Protein Isolate (WPI): This is whey that’s been extra-filtered to remove most of the fat and lactose (the sugar in milk). You’re left with something that’s about 90% pure protein, making it incredibly efficient. It also absorbs quickly, which is perfect for right after physical therapy or even just a short walk.
- Hydrolyzed Whey Protein: You can think of this as "pre-digested" whey. The protein chains have already been broken down into smaller bits, which can be a lifesaver for a sensitive gut. If you find regular protein powders cause bloating or discomfort, this is often a much gentler option.
The clinical evidence for whey protein isolate is compelling. One study looked at malnourished cancer patients on chemotherapy who added WPI to their diet. The results were significant: they gained muscle, strength, and body weight. Even better, overall chemotherapy toxicity dropped by 9.8%, and severe side effects plummeted by over 30%. You can read the full clinical trial findings here.
There's one other dairy option worth knowing: casein protein. It’s the opposite of whey. While whey is a fast-acting protein, casein digests very slowly, feeding your muscles a steady stream of amino acids over hours. This makes it a great choice for a bedtime shake to help prevent muscle breakdown overnight.
Gentle & Effective: Plant-Based Proteins
If dairy is off the table—whether due to lactose intolerance, an allergy, or personal choice—don't worry. There are some truly fantastic plant-based options out there that are often much easier on the digestive system.
When you're looking for a plant-based protein powder, here are the top contenders to keep an eye out for:
- Pea Protein: Made from yellow split peas, this is a wonderful hypoallergenic choice that's naturally rich in iron. It has a surprisingly smooth texture and is known for being very easy to digest, making it a safe bet for a sensitive stomach.
- Soy Protein: Soy is one of the few plant sources that is a complete protein, meaning it has an amino acid profile similar to whey. If you've heard conflicting information about soy and hormone-sensitive cancers, it’s reassuring to know that major cancer organizations have found that moderate amounts of whole soy foods are safe. This is absolutely a conversation to have with your oncologist, but for many, it's a great option.
- Brown Rice Protein: On its own, brown rice protein is not complete, but it’s often blended with pea protein to create a full amino acid spectrum. It’s another gentle, hypoallergenic choice that is usually well-tolerated.
Often, the best plant-based powders are actually a blend of a few different sources, like pea and rice. This is a smart way to ensure you're getting the full range of amino acids your body needs to heal and stay strong. The key is to find a clean, simple formula that works with your system, not against it.
How to Read the Label and What to Avoid
The front of a protein powder container tells you what the company is selling; the back tells you what you’re actually buying. Learning to be a label detective is one of the most empowering skills you can develop during treatment. It’s your best defense in making sure the product you choose is a true ally, not a source of hidden problems.
Think of the nutrition label as your personal checklist for safety and effectiveness. If you know where to look, you can quickly separate the high-quality options from the ones that could get in the way of your progress. It all comes down to spotting a few key red flags and green flags.

Ingredients to Avoid
When your system is already under stress, the last thing it needs is a supplement that adds to the burden. Unfortunately, many popular protein powders are packed with ingredients that can aggravate common treatment side effects like digestive upset or inflammation.
Keep an eye out for these red flags on the ingredient list:
- Artificial Sweeteners: Things like sucralose, aspartame, and acesulfame potassium can be really harsh on a sensitive gut. For many people, they trigger or worsen gas, bloating, and diarrhea.
- Excessive Added Sugars: A little sugar is okay, but you always want the protein content to be higher than the sugar content. Too much sugar can fuel inflammation and cause unwanted blood sugar spikes, which is the last thing you need.
- Thickeners and Gums: Additives like xanthan gum or carrageenan are just there for texture, but they can sometimes cause digestive distress, especially if your gut is already feeling fragile.
- Proprietary Blends: This is a big one. If you see a "proprietary blend" on the label, the company isn't telling you the exact amount of each ingredient. This lack of transparency means you have no idea if you're getting an effective dose of the good stuff or just a lot of cheap fillers.
A great rule of thumb is to look for a short, simple ingredient list. The very first ingredient should always be the protein source itself—like "whey protein isolate" or "pea protein"—not a sugar or filler.
Green Flags to Look For
Just as important as knowing what to avoid is knowing what to look for. These "green flags" are signs of a high-quality, safe, and effective product that puts your health first. You're looking for a powder that is clean, pure, and trustworthy.
It’s important to remember that the supplement industry isn’t regulated as tightly as pharmaceuticals. That’s why third-party certifications are so crucial—they are your best guarantee that the product is free from harmful contaminants and actually contains what the label claims.
Here are the seals of approval you want to see:
- Third-Party Certifications: Look for logos from organizations like NSF Certified for Sport or Informed-Sport. These independent groups test products to verify purity and potency, checking for things like heavy metals, pesticides, or banned substances. This is a huge layer of safety.
- Minimal Ingredients: Often, the best protein powder for someone going through cancer treatment is the one with the shortest ingredient list. A simple, unflavored powder with just one or two ingredients is the safest and most versatile choice.
- Helpful Add-Ins: Some formulas include beneficial extras. For example, L-glutamine is an amino acid known to support gut health and help repair the intestinal lining, which can be damaged by chemotherapy. This can be a great bonus, but the main focus should always be on the quality of the protein itself.
Ultimately, choosing an unflavored powder gives you the most control. You can mix it into foods and drinks you already enjoy without being locked into a specific flavor, which is a lifesaver when taste changes make certain flavors unappealing. This simple strategy helps you beat taste fatigue and stay consistent with your nutrition goals.
Making Protein Powder Work for You
Picking the right protein powder is a great first step, but figuring out how to actually use it in your daily life is where the real magic happens. This is where we go beyond just shaking powder and water in a bottle. We need practical, real-world strategies that can help you navigate the challenges that come with cancer treatment.
The goal here is simple: to make getting enough protein feel less like a medical task and more like a normal, comfortable part of taking care of yourself. What works for you one week might not the next, so having a few tricks up your sleeve is the key to staying on track.

Strategies for Managing Side Effects
Treatment side effects can make eating feel like a monumental effort. Nausea, changes in taste, and difficulty swallowing (dysphagia) are common hurdles that can get in the way. The trick is to adapt how you prepare your protein to work with your body, not against it.
Here are a few targeted ideas:
- When Nausea Strikes: A thick, sweet shake is probably the last thing you want. Try mixing an unflavored protein isolate into something cold, light, and easy on the stomach. Think chilled coconut water, a mild smoothie with frozen melon, or even just ice-cold water.
- For Difficulty Swallowing: If thin liquids are a problem, use protein powder to your advantage. Blend it into foods to create a thicker, smoother, and more nutrient-dense consistency that’s easier to manage. Think yogurt, oatmeal, or applesauce.
- To Combat Taste Fatigue: When everything tastes "off," unflavored powder becomes your best friend. You can sneak it into savory foods like mashed potatoes, creamy soups, or broths to boost protein without messing with a flavor you can actually tolerate. For more ideas, check out our guide on what to eat during chemotherapy.
Timing and Dosage for Better Results
It’s not just what you take, but when and how much. Tossing back a huge, 25-gram protein shake all at once can be overwhelming for a sensitive digestive system. There’s a better way.
The "little and often" approach is your best strategy. By breaking up your daily protein target into smaller, more frequent servings, you help your body absorb it more efficiently and sidestep issues like bloating or discomfort.
Aim for smaller servings of 10-15 grams of protein several times a day instead of one large shake. This is much gentler on your system and gives your body a steady stream of amino acids for ongoing tissue repair.
Think of it like watering a plant. You wouldn't dump a whole bucket of water on it at once—most of it would just run off. A slow, steady drip allows the soil to absorb what it needs. Your body is much the same with protein.
It can also be helpful to time your protein around light activity, like a short walk or a physical therapy appointment. Having a small protein serving within an hour of moving can help your muscles put those amino acids to work for repair and maintenance right away.
The Impact of Consistent Protein Intake
Sticking with it really does pay off. Keeping your protein levels up isn't just about feeling a bit stronger; it has a real, measurable impact on your recovery and ability to tolerate treatment.
For instance, a major review of studies found that high-protein nutritional supplements significantly cut down on post-treatment complications. It even helped shorten hospital stays by an average of 1.5 days, which is a huge deal when it comes to reducing infection risk. The analysis showed that protein intakes below 1.2 g/kg of body weight were linked to muscle wasting, while getting more than 1.4 g/kg helped preserve that crucial lean body mass. This is why finding a sustainable way to use your protein powder is such a vital part of your overall care plan.
Working with Your Oncology Team on Nutrition
While this guide gives you a solid foundation, your single greatest resource is your own healthcare team. Online articles are a great place to start, but they can never replace the personalized advice from people who know your complete medical history.
Your oncologist, registered dietitian, and nurses see the full picture. Think of it as a partnership. They have the clinical expertise, but you are the expert on your own body. You know how you feel day-to-day and which side effects are hitting you the hardest. This teamwork makes you an active, empowered participant in your own care.
Asking the Right Questions
One of the most powerful things you can do is walk into your appointments prepared. Having a list of specific questions makes your limited time more focused and productive. It’s how you build a nutrition plan that truly supports your medical treatment.
Jot your questions down in a notebook ahead of time so you don't forget anything in the moment. Taking this simple step ensures every choice you make, right down to finding the best protein powder for cancer patients, strengthens your body for the road ahead.
Your oncology dietitian is your go-to expert for this. They are specially trained to handle the unique nutritional needs that come with a cancer diagnosis. They can look at your bloodwork, factor in your specific treatment protocol, and even recommend particular brands that are safe and effective for you.
Your Nutrition Appointment Checklist
Instead of trying to figure it all out on your own, use your next appointment to get clear, actionable answers. Here are some essential questions to ask your oncologist or dietitian to fine-tune your protein strategy:
- What is my personal protein goal? Given my current weight, treatment schedule, and recent lab results, how many grams of protein should I be aiming for each day?
- Are there specific protein types I should use or avoid? Based on my diagnosis, is there any reason I should lean toward a plant-based protein instead of something like a whey isolate?
- Are there any specific ingredients I need to watch out for? Should I be concerned about any sweeteners, additives, or even extra vitamins in a supplement that could interfere with my chemo or other medications?
- How should I time my protein intake for the best results? Is it better to have it before or after my infusion appointments or on days I have physical therapy?
- What should I do if I start having digestive issues? If a protein powder makes me feel bloated or uncomfortable, what’s the best plan B?
Taking this proactive approach makes sure your nutrition plan is safe, effective, and working in sync with your medical care. This kind of collaboration often goes beyond diet alone. To learn about other ways to handle treatment challenges, you might want to read our guide on integrative therapies to manage side effects.
Your Questions, Answered
It's completely normal to have a lot of questions when you're navigating nutrition during cancer treatment. Let's tackle some of the most common ones that come up about protein supplements so you can feel more confident in your choices and have more informed talks with your healthcare team.
Can Too Much Protein Hurt My Kidneys During Treatment?
This is a really smart question and a very common concern. You’re being told to ramp up your protein, but you also want to be careful.
Here's the good news: for most patients without severe, pre-existing kidney disease, the higher protein levels we recommend during cancer treatment (typically 1.2 to 1.5 grams per kilogram of body weight) are not only safe but necessary. Your body is working overtime to fight the cancer and repair the damage from treatments, and that process requires a serious amount of protein.
That said, this doesn't mean more is automatically better. The key is to never self-prescribe very high doses of protein without getting the green light from your doctor. Your oncologist and dietitian are looking at your whole health picture, including your kidney function tests (like creatinine levels). They'll set a protein target that’s effective for healing without putting extra stress on your organs.
Is Soy Protein Safe if I Have a Hormone-Sensitive Cancer?
This is probably one of the biggest myths in oncology nutrition, and thankfully, we now have solid science to clear things up. The confusion comes from natural compounds in soy called phytoestrogens. Even though the name sounds a bit like human estrogen, they are chemically very different and act in a much weaker, more nuanced way in the body.
Major cancer research groups, like the American Institute for Cancer Research, have concluded that eating moderate amounts of soy is safe for survivors of breast cancer and other hormone-sensitive cancers. Some studies even suggest it could be beneficial.
So, when you're looking at a soy protein powder, it's still a good idea to have a quick chat with your oncology team to make sure it's a good fit for your specific plan. But you can let go of the old fear that "soy is unsafe"—the research just doesn't support it.
What if Protein Shakes Make Me Feel Sick?
Nausea can make even the thought of eating or drinking feel impossible. If protein shakes are turning your stomach, the trick is to outsmart the nausea, not force your way through it.
First, go for a high-quality, unflavored protein isolate. The artificial flavors, sweeteners, and even strong "natural" vanilla or chocolate flavors can be major triggers for a sensitive stomach. An unflavored powder is a clean slate and much less likely to cause a problem.
Next, play with the temperature and your pacing.
- Go Cold: Blend your powder with something ice-cold. Chilled almond milk, coconut water, or just plain ice water are often much easier to tolerate than room-temperature drinks.
- Sip, Don't Gulp: Use a straw and drink your shake slowly over 30 to 60 minutes. Small, steady sips are much gentler on your system than chugging it down.
- Add a Soothing Ingredient: Try blending in something known to calm the stomach. A small slice of fresh ginger, a few frozen peach slices, or a spoonful of plain yogurt can work wonders.
If you're still struggling, let your dietitian know. Sometimes, simply switching to a different protein source, like a pre-digested hydrolyzed formula or an easy-on-the-gut plant protein like pea, is all it takes.
Aren't Meal Replacement Shakes and Protein Powders the Same Thing?
This is a great question because they look similar on the shelf but do very different jobs.
Think of it this way: a protein powder is a specialist. Its main job is to deliver a concentrated dose of high-quality protein to help you rebuild tissue and preserve muscle. It doesn't bring a lot of extra carbs, fats, or calories to the party.
A meal replacement shake, on the other hand, is a generalist. It's designed to be a balanced meal in a glass, providing a mix of protein, carbs, fats, vitamins, and minerals. While these can be a lifesaver when you just can't face a solid meal, they often don't contain enough protein to meet the high demands of cancer treatment. A meal replacement might offer 10-15 grams of protein, whereas a single scoop of protein powder can easily provide 20-25 grams or more.
For many people, a better strategy is to add a pure, unflavored protein powder to foods you're already eating. You can stir it into oatmeal, boost a soup, or blend it into a fruit smoothie. This way, you get the protein you need without unwanted fillers or flavors, giving you more control and a more direct path to your goals.
At Hirschfeld Oncology, we know that a smart nutrition plan is a powerful part of your cancer care. If you have questions about how to best support your body through treatment, our team is here to help you find a path that feels right. Request a consultation today to explore a care plan built around your personal goals and well-being.





.png)


.png)
.png)




