When you hear the word “chemotherapy,” it’s completely normal to feel a wave of uncertainty. Let’s break down what it really is. At its heart, chemotherapy is a type of medicine that uses powerful drugs to find and destroy fast-growing cells anywhere in the body.
What Is Breast Cancer Chemotherapy and How Does It Work?
Think of it like this: if surgery and radiation are targeted strikes on a specific location, chemotherapy is a systemic, body-wide mission. The drugs travel through your bloodstream to hunt down cancer cells wherever they might be hiding.
This is chemotherapy’s greatest strength. It can attack the main tumor and any stray cancer cells that might have broken off and traveled elsewhere, even if they're too tiny to show up on a scan.
Of course, this powerful approach has a downside. The drugs can’t always tell the difference between a cancer cell and other healthy, fast-growing cells in your body—like the ones in your hair follicles or the lining of your mouth and stomach. This is why side effects happen. Your oncology team’s job is to strike a precise balance: being tough on the cancer while keeping you as comfortable and healthy as possible.
The Strategic Roles of Chemotherapy
Chemotherapy isn't a one-size-fits-all treatment. Its role in your plan is carefully chosen based on your specific type of breast cancer, its stage, and your overall health. Knowing why you’re receiving chemo can make the process feel much more manageable.
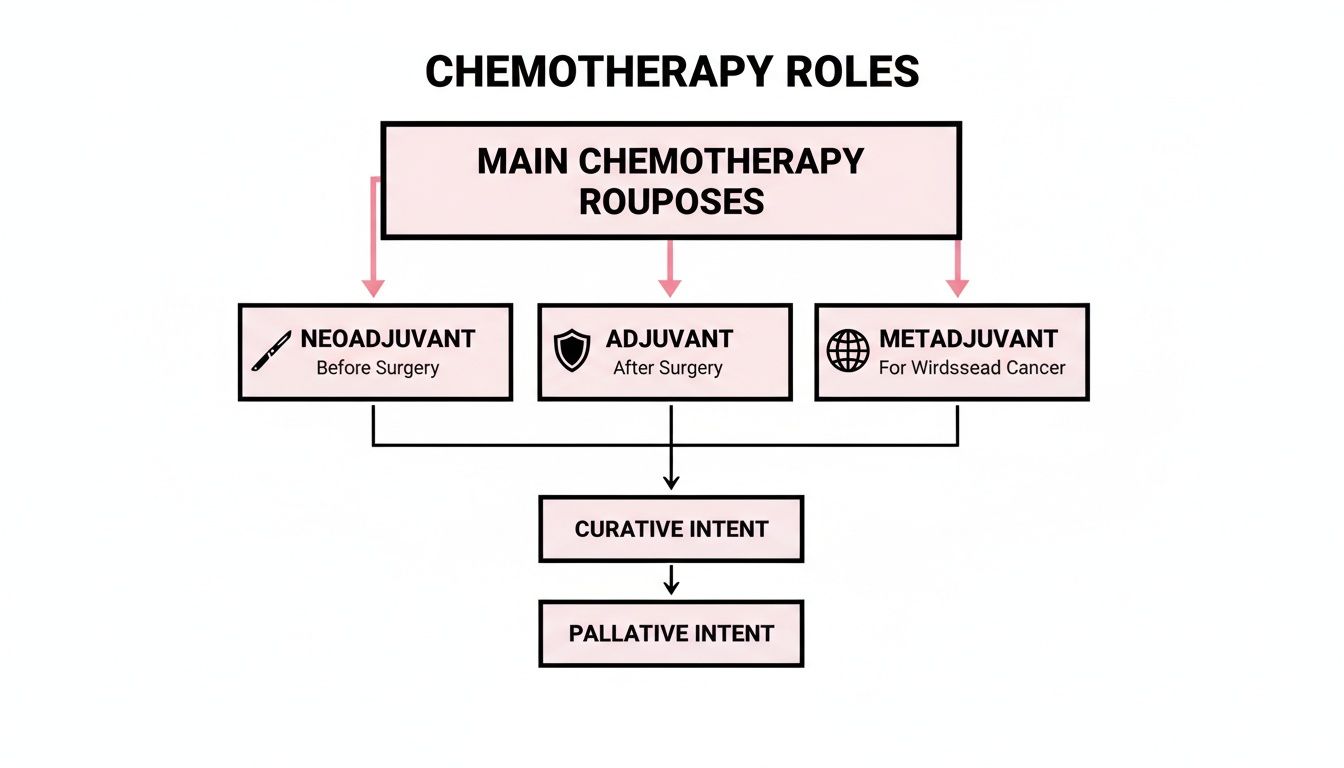
Your doctor might recommend chemotherapy in one of three main scenarios:
- Neoadjuvant Chemotherapy: This is chemo given before surgery. The primary goal here is to shrink the tumor. A smaller tumor is often easier to remove completely, and in some cases, it can make a less invasive surgery (like a lumpectomy instead of a mastectomy) possible.
- Adjuvant Chemotherapy: This is chemo given after surgery. Even when a surgeon is confident they've removed all visible cancer, there's always a chance some microscopic cells were left behind. Adjuvant chemo acts like a clean-up crew, circulating through the body to eliminate any lingering cells and lower the odds of the cancer coming back.
- Metastatic Cancer Treatment: For breast cancer that has spread to other parts of the body (Stage IV), chemotherapy is a cornerstone of treatment. Here, the goal shifts from a cure to long-term management. It’s used to shrink tumors, slow the cancer’s growth, ease symptoms, and help you live longer and better.
Every chemotherapy plan has a clear purpose. Whether it's to set the stage for a better surgical outcome, to get rid of any remaining cancer cells, or to manage advanced disease, the strategy is always tailored to your specific situation and long-term health.
The decision to include breast cancer chemotherapy in your treatment is one you'll make together with your care team. By understanding how it works and the specific job it’s meant to do for you, you can move forward with a clearer sense of purpose. It’s all about turning a complex medical plan into a series of understandable steps, all aimed at giving you the best possible outcome.
How Your Cancer Stage Shapes Your Chemotherapy Plan
When you're diagnosed with breast cancer, the chemotherapy plan your oncologist recommends is anything but a one-size-fits-all prescription. Think of it more like a custom-tailored strategy, built from the ground up based on the unique details of your diagnosis—especially your cancer's stage and its specific biological fingerprint.
This personalized approach is crucial because it ensures the treatment’s goals align perfectly with your situation.
For early-stage breast cancer (Stages I-III), the objective is simple and powerful: a cure. Chemotherapy is brought in to either make surgery more successful or to track down and eliminate any microscopic cancer cells that might be hiding out after surgery. It’s a proactive step that dramatically cuts down the risk of the cancer ever coming back.
The story changes when breast cancer has spread to distant parts of the body, which is known as Stage IV or metastatic cancer. Here, the goal shifts from a cure to long-term management. We use chemotherapy to control the cancer, slow its growth, ease symptoms, and—most importantly—extend and protect your quality of life.
Chemotherapy Goals by Breast Cancer Stage
To make this clearer, let's break down how the purpose of chemotherapy aligns with each stage. This table gives a quick overview of what we're trying to accomplish at different points in the journey.
As you can see, the timing and intent of the treatment are completely different depending on whether the cancer is localized or has spread.
The Strategic Roles of Chemo in Early-Stage Cancer
When cancer is still contained in the breast and nearby lymph nodes, we often use chemotherapy in one of two key ways.
- Neoadjuvant Therapy: This is chemo given before surgery. The main goal is to shrink the tumor, which can make the operation much easier. Sometimes, it can shrink a tumor enough to allow for a lumpectomy (breast-conserving surgery) instead of a full mastectomy.
- Adjuvant Therapy: This is chemo given after surgery. Think of it as an insurance policy. It travels through your entire bloodstream to hunt down and destroy any stray cancer cells that might have broken away from the main tumor but are too small to show up on scans.
The big idea here is to hit the cancer from every possible angle. By combining a systemic treatment like chemotherapy with a local one like surgery, your care team builds a really strong defense against the disease.
This flowchart helps visualize how these different roles fit into an overall treatment plan.
Going Deeper: Tailoring Treatment to Your Cancer's Subtype
Beyond just the stage, oncologists look at the specific "fingerprint" of your cancer cells to pick the most effective drugs. This is where personalized medicine really shines. Some of the most important factors we look at are:
- Hormone Receptor (HR) Status: If cancer cells have receptors for estrogen or progesterone, they're called HR-positive. These cancers use hormones to grow. While hormone-blocking therapy is a key treatment, we might add chemotherapy if the cancer seems aggressive or has a high chance of returning.
- HER2 Status: Some breast cancers make too much of a protein called HER2, which acts like a gas pedal for cancer growth. For these HER2-positive cancers, we often combine chemotherapy with targeted drugs that specifically shut down the HER2 protein. It’s a powerful one-two punch.
- Triple-Negative Breast Cancer: This type tests negative for estrogen receptors, progesterone receptors, and extra HER2 protein. Since it lacks these common targets, chemotherapy becomes the main treatment. The good news is that these faster-growing cells are often very responsive to chemotherapy.
Getting this level of detail is a core part of what is precision oncology, a field focused on matching the right treatment to the right tumor.
The impact of these smarter, more targeted strategies is huge. The 44% decline in U.S. breast cancer mortality since 1989—which translates to an estimated 517,900 lives saved through 2022—is a direct result of combining early detection with more effective treatments like chemotherapy and targeted therapies.
Understanding Common Chemotherapy Drugs and Regimens

When your oncologist starts talking about drug regimens and using acronyms like "AC-T," it can feel like you’re suddenly trying to learn a new language. But behind those technical terms is a very deliberate strategy for fighting breast cancer from multiple angles at once. The idea isn't just to use one drug, but to create a powerful, coordinated attack.
Instead of one single "chemotherapy" drug, there are actually several different classes of medications. Each one has a unique way of targeting cancer cells. Think of it like a specialized toolkit—your care team selects the right tools for your specific situation to build the most effective treatment plan.
Major Classes of Chemotherapy Drugs
Two of the most common and effective groups of drugs used in breast cancer chemotherapy are Anthracyclines and Taxanes. While both are powerful, they go about disrupting cancer cells in completely different ways.
Anthracyclines (e.g., Doxorubicin): These drugs get inside a cancer cell and damage its DNA. Imagine a cancer cell is a factory with a set of blueprints (its DNA) for making more factories. Anthracyclines scramble those blueprints, making it impossible for the cell to copy itself and divide. This is a direct way to halt the cancer's ability to grow.
Taxanes (e.g., Paclitaxel, Docetaxel): These drugs take a totally different approach. They target the cancer cell's internal "skeleton," known as microtubules, which need to be flexible for a cell to divide. Taxanes essentially freeze this skeleton in place, making it rigid and useless. It’s like pouring concrete into the factory's machinery—everything grinds to a halt, and the cell can no longer complete the division process.
Other types of drugs, like Alkylating agents and Antimetabolites, also play key roles. They might introduce errors into the cancer cell’s genetic code or block it from getting the nutrients it needs to grow. Each class gives us a distinct method for stopping cancer in its tracks.
Building a Powerful Treatment Regimen
This is where the strategy really comes together. A "regimen" is simply the specific combination of drugs you receive and the schedule for giving them. Oncologists almost never use just one chemotherapy drug because cancer cells are notoriously clever and can develop resistance to a single line of attack.
By combining drugs that work in different ways, we create a multi-pronged assault that is much, much harder for cancer cells to withstand.
A common analogy is planning a siege on a castle. You wouldn't just attack the front gate. You'd also cut off supply lines and target the command center. A chemotherapy regimen does the same thing to cancer cells, hitting them from multiple angles at once to overwhelm their defenses.
This approach is what leads to the acronyms you'll hear, which are just shorthand for the combination of drugs being used. For instance, a very common and effective regimen is "AC-T":
- "A" stands for Adriamycin (the brand name for Doxorubicin, an Anthracycline).
- "C" stands for Cytoxan (an Alkylating agent).
- "T" stands for Taxol (the brand name for Paclitaxel, a Taxane).
With this regimen, a patient typically receives the 'AC' combination for a set number of cycles, followed by the 'T' for several more. This strategic sequencing ensures the cancer is hit with different mechanisms of action over the course of treatment.
How a Regimen Is Chosen for You
Deciding on a chemotherapy regimen is a highly personalized process. Your oncology team considers a whole host of factors to create a plan that is both tough on your cancer and manageable for you.
Key factors that influence this decision include:
- Cancer Subtype: This is a big one. As we've discussed, whether your cancer is HR-positive, HER2-positive, or triple-negative is a primary driver, as certain drugs are known to be far more effective for specific subtypes.
- Cancer Stage and Grade: The tumor's size, whether it has spread to lymph nodes, and how aggressive the cells look under a microscope (the grade) all help us determine how intensive the regimen needs to be.
- Your Overall Health: Your age, other medical conditions (like your heart health), and your general fitness level are crucial. The goal is to choose a regimen your body can handle without causing unnecessary harm.
- Genomic Test Results: For some breast cancers, tests that analyze the tumor's genes can help predict the odds of recurrence and tell us whether chemotherapy will provide a significant benefit at all.
This careful, personalized selection process is at the heart of modern cancer care. We've moved far beyond a one-size-fits-all approach and toward truly individualized plans that maximize the treatment's impact while always keeping your well-being front and center.
Navigating and Managing Chemotherapy Side Effects

Let's be honest: thinking about the side effects of breast cancer chemotherapy can be incredibly intimidating. It’s often one of the most stressful parts of starting treatment. But it's crucial to know that not everyone gets every side effect, and we have more tools than ever to keep you comfortable.
The first step in feeling more in control is understanding why these side effects happen. Chemotherapy drugs are designed to hunt down and attack rapidly dividing cells—the very definition of cancer. The catch is that some of your body's healthy cells also divide quickly. Think of the cells in your hair follicles, the lining of your mouth and digestive system, and the bone marrow responsible for making blood cells. When chemo affects these healthy cells, that’s when side effects pop up.
The great news is that your healthy cells are incredibly resilient. They can repair themselves, which is why most side effects are temporary and fade after treatment ends. Your oncology team’s entire focus is on getting you through this as smoothly as possible, and your voice is the most important part of that process.
Common Side Effects and Proactive Strategies
While everyone’s journey is different, there are a few side effects that tend to be more common. The good news is that we have proven strategies—both medical and lifestyle-based—to help you through them.
Fatigue
This isn’t just feeling tired. It's a profound, bone-deep exhaustion that sleep doesn't always fix. It's also one of the most common things patients report.
- Management Tip: It might sound backward, but gentle movement like a short walk can actually boost your energy. Most importantly, listen to your body. Prioritize what needs to get done and don’t be afraid to ask for help with things like groceries or cooking.
Nausea and Vomiting
Modern anti-nausea drugs (called antiemetics) are a game-changer. Your doctor will likely have you take them before you even feel sick, both before and after your infusion, to prevent nausea from starting in the first place.
- Management Tip: Try eating small, frequent snacks throughout the day instead of three large meals. Bland foods like crackers, toast, and rice are often easier to tolerate. You might also find that avoiding strong smells helps keep your stomach settled.
Hair Loss
This can be an incredibly emotional experience, but hair loss from chemo is almost always temporary. It usually starts a few weeks after your first treatment and will grow back.
- Management Tip: Some people find that getting a short haircut beforehand gives them a feeling of control over the situation. Others start exploring fun wigs, scarves, or hats. There's also an option called cold capping, a therapy that cools the scalp during infusions to help reduce hair loss, which is something you can discuss with your care team.
"Managing side effects is a partnership between you and your care team. Your input is vital. By tracking your symptoms and speaking up about what you're experiencing, you give your team the information they need to adjust your supportive care plan and keep you feeling your best."
Addressing Cognitive and Blood-Related Changes
Beyond the more visible side effects, chemo can also affect how you think and what's going on inside your body.
Cognitive Changes ('Chemo Brain')
This is a frustratingly real side effect. You might feel a bit foggy, have a hard time concentrating, or struggle to find the right word. It’s common, and it’s usually temporary.
- Management Tip: Lean on tools to help you out. Use a notebook or your phone for reminders. Sticking to a routine can help, as can getting enough sleep. Gentle mental exercises like puzzles or reading can also keep your mind sharp.
Changes in Blood Counts
Chemotherapy can lower your white blood cells (making you more prone to infection), your red blood cells (causing anemia and fatigue), and your platelets (leading to easier bruising or bleeding).
- Management Tip: Your team will be watching your blood counts like a hawk. You can help by practicing excellent hand hygiene, avoiding big crowds during flu season, and calling your doctor right away if you develop a fever or any other sign of infection.
In the U.S. alone, where an estimated 316,950 women and 2,800 men will face invasive breast cancer this year, treatment is constantly evolving. We're seeing more low-dose chemo options designed to minimize these very side effects—a patient-first philosophy we embrace at Hirschfeld Oncology here in Brooklyn. For a broader look at the rising incidence of breast cancer, you can find global estimates here.
Effectively managing side effects is a pillar of successful cancer treatment. To dive deeper, take a look at our guide on 5 essential strategies for managing side effects and improving quality of life during cancer treatment.
Thinking Beyond Traditional Chemo: Gentler, More Targeted Options
The world of cancer treatment is always moving forward. While standard breast cancer chemotherapy is still a critical weapon in our arsenal, we're constantly finding smarter, more precise ways to fight the disease. These newer approaches can be used right alongside chemo or sometimes as an alternative.
The goal is to move from a broad, systemic attack to something more like a targeted strike. It’s about fighting cancer with more finesse, hitting the cancer cells hard while doing our best to spare healthy tissue. This evolution in thinking opens up a whole new world of possibilities, especially for patients with advanced or hard-to-treat cancers.
Targeted Therapy: A Molecular Lock and Key
One of the biggest breakthroughs has been targeted therapy. Think of it this way: traditional chemo is like a bomb that affects all fast-growing cells, both cancerous and healthy. Targeted drugs, on the other hand, are engineered to hunt for specific markers—or "targets"—that are unique to the cancer cells.
Imagine a cancer cell has a special kind of lock on its surface that helps it grow and spread. Targeted therapies are like perfectly crafted keys designed to fit only that lock. Once the drug "key" connects with the cancer cell's "lock," it can block the signals that tell the cell to grow, or even flag it for destruction.
A classic example for breast cancer is Trastuzumab (Herceptin). This drug is designed to go after the HER2 protein, which acts like a stuck gas pedal in HER2-positive breast cancers. By blocking this protein, Herceptin essentially puts the brakes on cancer growth, often with far fewer of the side effects we see with conventional chemotherapy.
Immunotherapy: Unleashing Your Body's Own Defenses
Another fascinating strategy is immunotherapy. Instead of attacking the cancer directly with a drug, this approach wakes up your own immune system to do the job it was born to do: hunt down and destroy abnormal cells.
Cancer cells are tricky. They often find ways to put on a disguise, making themselves invisible to the body's natural defenses. Immunotherapy drugs, often called checkpoint inhibitors, work by ripping that disguise off.
This unmasking allows your T-cells—the 'soldiers' of your immune system—to finally see the cancer for what it is and launch a full-scale attack. We're essentially turning your own body into a powerful, cancer-fighting machine.
This approach has been a game-changer for certain types of triple-negative breast cancer, giving us an important new tool when other treatments might not be as effective.
Metronomic Chemotherapy: A Gentler, Steady Approach
We're even rethinking how we use traditional chemotherapy itself. Metronomic chemotherapy, sometimes called low-dose chemo, completely flips the old model on its head. Instead of giving a patient large, intermittent doses with long breaks, we administer much smaller doses more frequently over a continuous period.
It’s like the difference between flooding a garden with a harsh chemical once a month versus pulling a few weeds every single day. The metronomic approach aims to keep the cancer in check by steadily disrupting its blood supply (a process called angiogenesis), which tumors need to grow.
This constant, low-level pressure can control the cancer just as effectively but with significantly fewer and milder side effects. It’s a more sustainable way to manage the disease long-term, which can make a world of difference for a patient’s quality of life.
What to Expect on Infusion Day

Walking into your first breast cancer chemotherapy appointment can bring a wave of emotions. Knowing what the day actually holds can help turn that anxiety into a sense of control. The infusion suite is designed to be a quiet, supportive space where your only job is to sit back and let the medical team take care of you.
First, you’ll check in just like any other doctor's appointment. An oncology nurse will then get you settled into a comfortable recliner, take your vital signs—like blood pressure and temperature—and check in on how you've been feeling. This is the perfect time to bring up any new side effects or concerns you have.
Next, the nurse will need to access a vein to deliver the medicine. For most people, this means placing a small, temporary IV in the hand or arm. If you have a port, they’ll access that instead. These nurses are experts at this, so it’s usually a quick and routine step.
The Infusion Process Explained
Before any chemo drugs are started, you’ll get what we call "pre-medications." Think of these as a protective first step. They often include anti-nausea drugs and steroids to help prevent or lessen potential side effects before they even have a chance to start.
After the pre-meds are done, the main event begins: the chemotherapy infusion. The medication, mixed in an IV bag, will drip slowly through the line over a specific amount of time. Depending on your regimen, this could be less than an hour or it could take several hours. Your nurse will be checking on you the entire time to make sure you're doing okay.
Your oncology nurses are your lifeline during an infusion. They are highly skilled at administering treatment, but they are also there to manage your comfort. Never hesitate to speak up if you feel nauseous, cold, or just need something.
Making Your Time More Comfortable
Bringing a small “chemo comfort bag” can completely change your experience. You’ll be sitting for a while, so having a few things to help you relax and pass the time is a game-changer.
- Warmth and Comfort: Infusion centers can be chilly. A soft blanket, cozy socks, or a favorite sweater can make all the difference.
- Entertainment: A good book, a tablet with headphones for movies or music, or even a journal can help the hours fly by.
- Snacks and Drinks: Unless your team has told you otherwise, pack some light, bland snacks and a water bottle to stay hydrated.
Knowing the flow of the day helps, but there's more you can do to feel ready. For a deeper dive, read our guide on how to prepare for chemotherapy to walk in feeling even more confident.
Common Questions About Breast Cancer Chemotherapy
When you're facing breast cancer chemotherapy, it’s completely normal for your mind to be racing with questions. Getting clear, straightforward answers can help you feel more grounded and prepared for what’s to come. Let's walk through a few of the most common ones.
How Long Does a Chemotherapy Cycle Last?
Think of a chemotherapy "cycle" as a repeating block of time that includes your infusion day and the built-in recovery period afterward. It’s not just the time you spend in the treatment chair.
The exact length of a cycle really depends on your specific drug regimen, but they often last two, three, or four weeks. For instance, a common schedule might be getting infusions on day one and day eight of your cycle, followed by 13 days of rest to let your body recuperate. That adds up to a 21-day cycle, and a full course of treatment is usually made up of four to six of these cycles over several months.
Can I Work During Chemotherapy?
For many people, the answer is yes, though usually with some adjustments. Your ability to work really hinges on a few things: the physical demands of your job, the specific chemo drugs you're receiving, and most importantly, how you feel from one day to the next.
Some patients find that switching to part-time hours or arranging to work from home makes a world of difference. A popular strategy is to schedule infusions on a Friday, giving you the weekend to rest and manage any immediate side effects. The key is having an open conversation with your employer about needing a bit more flexibility.
Everyone’s experience is different. The most important thing is to listen to your body and not push yourself too hard. Your care team can also help with any paperwork or letters you might need for workplace accommodations.
How Will I Know if the Chemotherapy Is Working?
This is a big question, and thankfully, your oncology team has several reliable ways to monitor your progress and make sure the treatment is doing its job.
Your doctor will track the cancer’s response using a combination of methods:
- Imaging Scans: Tools like CT or PET scans are used periodically to get a clear picture of any tumors. The goal is to see them shrinking over time.
- Blood Tests: Certain blood tests can look for tumor markers—substances that some cancer cells release. A drop in these levels is often a good sign.
- Symptom Improvement: Simply feeling better is also a powerful indicator. Your oncologist will regularly check in to see if your cancer-related symptoms are easing up.
This consistent monitoring ensures your breast cancer chemotherapy is having the intended effect and allows your team to make adjustments if needed.
At Hirschfeld Oncology, we believe that feeling informed is a crucial part of feeling empowered. If you have more questions or are looking into treatment options in the Brooklyn area, our team is here to offer clear guidance and compassionate care. You can find more helpful information on our blog: https://honcology.com/blog.





.png)


.png)
.png)




