Hearing that your breast cancer has come back is a deeply unsettling moment. It's natural to feel like you're back at square one, but it's important to understand that this isn't a failure of your initial fight or a sign that you did something wrong.
Think of it this way: some of the original cancer cells were tough enough to survive the first round of treatment. They may have laid low, dormant and undetectable, for months or even years. A recurrence just means these cells have woken up and started to grow again. This isn't a repeat of your first journey; it’s a new chapter that calls for a different, often more targeted, plan.
Understanding Your Path Forward After a Recurrence

While the news is tough, you're not starting from a blank slate. You have the benefit of experience, and the field of oncology has made incredible strides. There are more advanced treatments and new avenues of hope available now than ever before. This guide is here to be your roadmap, helping you make sense of the path ahead.
Your medical team's first goal is to get a clear picture of this new growth—where it is, what its characteristics are—and then build a strategy to manage it as effectively as possible.
What This Guide Will Cover
We created this comprehensive resource to empower you with clear, compassionate information about every part of a breast cancer recurrence. We'll walk through:
- The different types of recurrence: We'll explain the difference between local, regional, and distant recurrence and what each one means.
- Key risk factors and symptoms: Knowing what to watch for is one of the most powerful tools for early detection.
- Modern, evidence-based treatments: We'll dive into everything from targeted therapy and immunotherapy to other innovative approaches.
- Emotional support and decision-making: You'll find guidance on navigating the emotional side of things and how to approach getting a second opinion.
The risk of recurrence is typically highest in the first few years right after your initial treatment, and it goes down over time. This is why your follow-up care and monitoring are so critical. For the 66% of patients diagnosed when the cancer is still localized, the five-year relative survival rate is an incredible 99%. It’s a powerful reminder of how much early detection matters.
A recurrence diagnosis is not a step backward. It's a pivot toward a new, more informed strategy. Your experience, your resilience, and the latest advancements in oncology are all powerful tools in your arsenal for this next phase.
Navigating this new path means building on what you already know. For a solid foundation on your initial diagnosis and treatment, you can explore our detailed guide to breast cancer. Arming yourself with this knowledge is the best way to prepare for productive, confident conversations with your oncology team about what comes next.
Identifying the Signs of Recurrent Breast Cancer

Once your initial treatment is complete, one of the most important things you can do is learn to listen to your body. Knowing the potential signs of a breast cancer recurrence makes you an active, empowered member of your own long-term health team.
Spotting a new change doesn't mean you should jump to the worst conclusion, but it's a clear signal that it's time to check in with your oncologist.
Think of it this way: your initial cancer was like a stubborn weed in a garden. Treatment was the process of removing it, but sometimes, tiny roots or seeds can get left behind. A recurrence is simply that weed trying to re-sprout.
This can happen in three main ways, and each has its own set of potential warning signs.
H3: Local Recurrence: Right Back in the Same Spot
A local recurrence is exactly what it sounds like—the cancer has reappeared in the same place it started. This could be in any remaining breast tissue or along the chest wall where a mastectomy was performed. It’s the most common form of breast cancer recurrence.
The symptoms often echo those of an initial diagnosis and can be found during a self-exam or on a routine follow-up scan.
- A new lump in the breast, on the chest wall, or near your mastectomy scar.
- Skin changes like thickening, redness, or dimpling over the breast or scar.
- Nipple changes, such as new discharge, turning inward (inversion), or skin that looks flaky or inflamed.
- Unexplained swelling of the breast or a part of it.
After surgery and radiation, your body has a "new normal." The key is to get familiar with it so you can spot any new, persistent changes that are worth a conversation with your doctor.
H3: Regional Recurrence: Spreading to Nearby Areas
With a regional recurrence, the cancer cells have moved into the "garden beds" next door. This means they've traveled to the lymph nodes closest to the original tumor, most often those under the arm (axillary nodes), around the collarbone, or in the neck.
The signs can be subtle at first, which is why any lasting changes in these areas need a professional look.
- A lump or swelling under the arm, above the collarbone, or in the neck.
- Constant pain in the arm or shoulder on the same side as the original cancer.
- Arm swelling (lymphedema) that is new or getting worse.
- Numbness or tingling that lingers in your arm or hand.
Catching a local or regional recurrence early gives you the best possible chance for successful retreatment. Your vigilance, paired with your oncologist's follow-up plan, creates a powerful safety net.
H3: Distant Recurrence: Settling in Far-Off Places
A distant recurrence, also known as metastasis, means the cancer "seeds" have traveled through the bloodstream or lymphatic system to a completely different part of the body. The cancer has set up shop in organs far from the breast.
While this is the most serious type of breast cancer recurrence, treatments for metastatic disease have come a long way. The focus now is often on managing it as a chronic condition and preserving your quality of life.
The symptoms of a distant recurrence depend entirely on where the cancer has landed. The most common sites are the bones, lungs, liver, and brain.
- Bones: New, persistent bone pain (especially in the back, hips, or ribs) or a fracture from a minor or unknown injury.
- Lungs: A nagging dry cough that won't go away, shortness of breath, or constant chest pain.
- Liver: Pain or swelling in the abdomen, yellowing of the skin and eyes (jaundice), loss of appetite, or nausea.
- Brain: Persistent headaches that feel different from your usual ones, vision problems, seizures, dizziness, or sudden confusion.
Here is a quick reference table to help keep these signs clear.
Symptoms of Breast Cancer Recurrence by Type
Knowing these signs is your first line of defense. If any of these symptoms appear and stick around, don’t wait. A quick call to your oncology team lets them investigate right away and start treatment when it can do the most good.
Why Does Cancer Come Back? A Look at Your Personal Risk
After finishing breast cancer treatment, the last thing anyone wants to think about is the cancer returning. So, when it does, the first question is almost always, "Why?" It’s a completely natural question, but it's important to know that a recurrence isn't anyone's fault. It doesn't mean your first treatment was wrong or that you did something to cause it.
The reality is that cancer treatment is incredibly powerful, but sometimes, a few hardy cancer cells can survive. Think of it like pulling weeds in a garden—no matter how thorough you are, a tiny root fragment might get left behind. These microscopic cells can lie dormant, invisible to scans and tests, for months or even years before they reawaken and start to multiply.
It All Starts with the Original Tumor
No two breast cancers are exactly alike, which means the risk of recurrence is different for everyone. Your risk is tied directly to the specific "personality" of the cancer you had initially. Your oncologist studies these details closely to build a follow-up plan that’s right for you.
Several key factors from your first diagnosis are crucial in figuring out this risk:
- Tumor Size and Grade: A larger tumor or one with a higher "grade" (meaning the cells look very different from normal cells and are dividing quickly) often carries a higher risk of coming back.
- Lymph Node Status: Finding cancer cells in the lymph nodes under your arm is a sign that the cancer had the potential to travel. This raises the possibility that some cells may have escaped to other parts of the body.
- Surgical Margins: After a lumpectomy, a pathologist checks the tissue edges. "Clear" margins are the goal, showing a healthy buffer around the cancer. If margins are "positive," it could mean some cancer cells were left behind, increasing local recurrence risk.
These details give your care team a baseline understanding of your risk and help determine how closely you need to be monitored in the years ahead.
Understanding Your Cancer’s Genetic ID
Beyond its size and location, the biology of the tumor itself is one of the most important predictors. Think of it like the cancer's genetic ID card—it tells us what makes it grow and what its weaknesses are.
The most critical markers are the hormone receptor status (estrogen/ER and progesterone/PR) and HER2 status. These effectively tell us what the cancer uses for fuel and guide our most powerful long-term treatments.
For instance, cancers that are ER-positive are fueled by estrogen. This is actually good news, as it means we can use hormone-blocking therapies, often for 5-10 years, to dramatically lower the risk of recurrence. On the other hand, triple-negative breast cancers (negative for ER, PR, and HER2) don't have these targets, which can give them a higher chance of returning, typically within the first few years after treatment.
Genomic Testing: A Deeper Look at Recurrence Risk
For an even more precise risk assessment, your oncologist might recommend a genomic test. Performed on the original tumor tissue, tests like Oncotype DX or MammaPrint analyze a specific set of genes to calculate a "recurrence score." This score is incredibly helpful for predicting the likelihood of a distant recurrence and can help decide if chemotherapy is truly necessary after surgery for certain types of early-stage, ER-positive cancers.
This detailed, personalized approach is vital. Breast cancer is a global health issue, with an estimated 2.3 million women diagnosed worldwide in 2022 alone. These staggering numbers, highlighted by organizations like the World Health Organization, underscore why expert, research-driven care is so critical. By understanding your cancer’s unique blueprint, you and your team can create a proactive plan that gives you the best chance for a healthy future.
Navigating Your Treatment Options for Recurrent Breast Cancer
Hearing that your breast cancer has come back can feel like a punch to the gut. It's completely understandable. But it’s crucial to know that this isn't the same fight you had before, and the tools we have today are in a different league entirely.
A recurrence doesn't mean starting over from square one. It means it’s time for a new game plan, armed with smarter, more sophisticated treatments that zero in on the cancer's unique characteristics. The first step is almost always a new biopsy, because the cancer you have now might be biologically different from the original. This gives us the precise intel we need to choose the most effective strategy for you.
Targeted Therapies: The "Smart Bomb" Approach
Think of traditional chemotherapy as a carpet bomb—it takes out fast-growing cells, but it can’t always distinguish between cancer cells and healthy ones. Targeted therapies, on the other hand, are like smart bombs or guided missiles. They are engineered to find and attack a specific feature on or inside cancer cells.
These treatments work by shutting down the specific pathways that cancer cells use to grow and spread, leaving most of your healthy cells untouched. It’s a much more precise and often kinder way to fight the disease.
- For HER2-Positive Cancers: If the cancer cells have too much of a protein called HER2, we can use drugs like trastuzumab (Herceptin) or pertuzumab (Perjeta). These drugs act like roadblocks, blocking the HER2 signals that tell the cell to divide.
- For Hormone Receptor-Positive Cancers: When cancer is fueled by hormones like estrogen, we can combine hormone therapy with a class of drugs called CDK4/6 inhibitors. These medications, like palbociclib, interrupt the cell's copy machine, stopping it from making more cancer cells.
- For BRCA Mutations: If you have an inherited BRCA gene mutation, your cancer cells have a built-in weakness in their DNA repair kit. PARP inhibitors are drugs that cleverly exploit this flaw, causing the cancer cells to break down and die.
This chart helps visualize how we use these biological clues to map out a treatment plan.
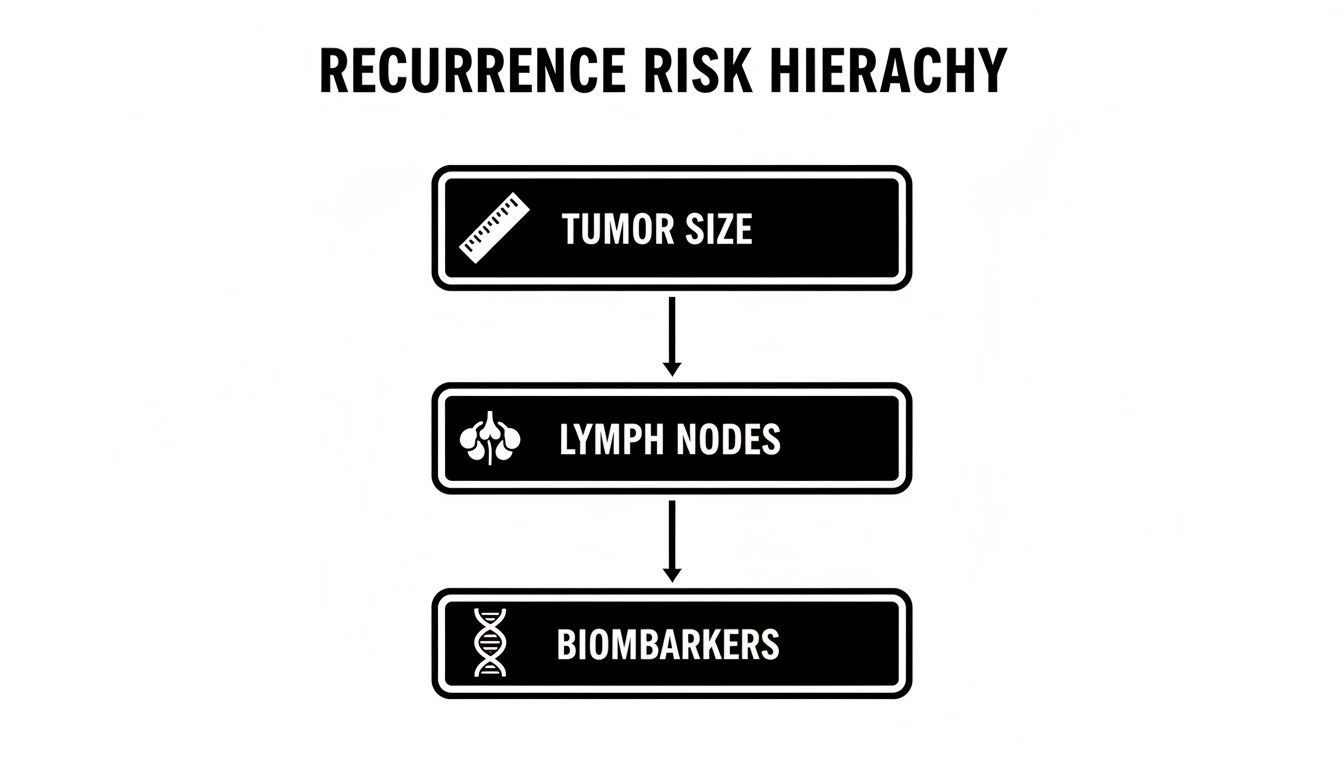
While things like tumor size still matter, the cancer's unique biomarkers are really the key that unlocks these modern, targeted treatments.
Immunotherapy: Taking the Brakes Off Your Immune System
Immunotherapy is one of the most exciting advances in cancer care. Instead of attacking the cancer directly with outside drugs, this approach rallies your body's own defense system to do the job.
Cancer cells are tricky; they can essentially wear a disguise that makes them invisible to your immune cells. They put up a "don't attack me" signal. Immunotherapy drugs, called checkpoint inhibitors, work by ripping off that disguise. They block the "off" signal, which effectively takes the brakes off your immune system and unleashes it to recognize and destroy the cancer.
Immunotherapy has been a true game-changer for certain aggressive types of recurrent breast cancer, especially triple-negative breast cancer (TNBC). It's given us a powerful new way to fight back when options used to be very limited.
To see how these cutting-edge therapies are being tested and refined, it's worth exploring ongoing https://honcology.com/blog/clinical-trials-for-breast-cancer.
Low-Dose Metronomic Chemotherapy: A Gentler, Steadier Fight
The old way of thinking about chemo was to hit the cancer with the highest dose possible, then take a break to recover from the side effects. Metronomic chemotherapy flips that idea on its head. It involves giving much lower doses of chemo more frequently, sometimes even daily in pill form.
The goal here isn't to obliterate the cancer in one fell swoop. Instead, this gentle, steady pressure works by cutting off the tumor's supply lines—it prevents the cancer from building new blood vessels to feed itself. By starving the tumor, we can often control its growth long-term, turning the cancer into a manageable chronic condition with far fewer side effects like nausea or hair loss.
Making the Right Choice for Your Future
Choosing a path forward is a decision you and your oncology team will make together. There's no one-size-fits-all answer. The best strategy will be tailored to your cancer's specific biology, where it has recurred, what treatments you've had before, and, most importantly, what your personal goals are.
It’s about finding the right balance—aggressively managing the cancer while protecting your quality of life. For patients in advanced stages where comfort becomes the top priority, options like compassionate in home hospice care can provide incredible support focused on dignity and well-being.
A recurrent breast cancer diagnosis is serious, but it is met with more hope, more science, and more options than ever before. The focus today is on creating a smart, sustainable plan that lets you live your life as fully as possible.
Finding Support and Expert Guidance for Your Journey
Navigating a breast cancer recurrence isn’t something you should ever have to do alone. While the medical treatments are the foundation of your plan, caring for your whole self—your mind, body, and spirit—is just as crucial. One of the most powerful things you can do is build a rock-solid support system.
A recurrence can unleash a whole new wave of emotions, from profound anger and fear to sheer exhaustion. The first step is simply to acknowledge that these feelings are real and valid. The emotional toll is significant, and having dedicated resources to help you process everything can make an enormous difference in your resilience and overall quality of life.
Assembling Your Emotional and Practical Support Team
Trying to manage the day-to-day logistics of treatment while also carrying the emotional weight of a recurrence is a monumental task. This is where leaning on others is a sign of incredible strength, not a burden. Many people I've worked with find that a mix of professional guidance and peer connection gives them the most complete and effective support.
You've got a lot of options for building this network:
- Support Groups: There's something incredibly validating about connecting with people who just get it. Whether you find a group in person here in NYC or connect with one online, these are safe spaces to share your fears, swap practical tips, and find genuine encouragement from those on a similar path.
- Professional Counseling: A therapist who specializes in oncology can give you concrete coping strategies for the anxiety, depression, and stress that often accompany a cancer diagnosis. It’s a private, dedicated space to work through it all.
- Patient Navigators: Think of these healthcare professionals as your personal guides through the maze of the healthcare system. They help coordinate appointments, translate complex medical jargon, and connect you with financial or logistical resources, lifting a huge practical weight off your shoulders.
A second diagnosis can be emotionally devastating. You have to make a conscious decision to lean on others for support. It’s okay to ask for help—it’s a necessary part of focusing on your healing.
Managing the physical side of things is also a huge piece of the puzzle. Pain, fatigue, and other side effects can be completely draining, but they don’t have to run your life. As you move through treatment, exploring options like palliative care services can provide essential relief, focusing on your comfort and improving your quality of life every step of the way.
The Power of a Second Opinion
Let's be clear: seeking a second opinion after a breast cancer recurrence is not about distrusting your current doctor. It’s an empowering, proactive step to make sure you have every piece of information possible to move forward with complete confidence. Cancer care is incredibly complex, and different experts often bring fresh perspectives or knowledge of different treatment approaches to the table.
A second opinion can accomplish several key things:
- Confirm Your Diagnosis: Just having another expert review your pathology reports and scans brings a huge amount of peace of mind that the diagnosis is 100% accurate.
- Broaden Your Treatment Options: Another oncologist might know about specific clinical trials or newer therapies—like targeted drugs or immunotherapy—that are a better match for your cancer’s unique biology.
- Align Care with Your Goals: This is your chance to make sure your treatment plan truly reflects what matters most to you, whether that’s pursuing the most aggressive options or prioritizing quality of life.
Ultimately, this whole process is about finding a care team you genuinely connect with and trust. For those of us in the New York City area, this might mean consulting with a practice like Hirschfeld Oncology, which specializes in crafting personalized plans for complex and recurrent cancers.
The goal is to build a true partnership with your medical team. You deserve to feel heard, respected, and absolutely confident that you are on the best possible path forward. Taking the time to gather information and find the right experts is a critical investment in your own well-being and an essential part of taking control of your journey.
Your Next Steps in New York City
If you're in the New York City area and facing a breast cancer recurrence, it's so important to know that exceptional, empathetic care is close by. Getting this news can feel like a huge step backward, but it’s really a sign that we need to shift our approach and build a new, highly specific strategy for you.
Here in Brooklyn, Dr. Azriel Hirschfeld and the Hirschfeld Oncology team specialize in just that—designing precise treatment plans for complex and recurrent cancers. We’re right here for our communities, from Williamsburg to Bushwick and all the neighborhoods in between.
Finding the Right Partner for Your Care
Our entire practice is built on a simple philosophy: use sophisticated, less-toxic treatments that target the cancer effectively while protecting your quality of life. We see this as a partnership. You are at the center of every decision we make together. The single most important thing you can do right now is take that next step.
Taking action is the first step toward regaining a sense of control. Exploring your options with a specialist provides clarity and replaces uncertainty with a concrete, hopeful plan.
We invite you to request a consultation to talk through your unique situation. This is a chance to understand the latest therapies available to you—from targeted drugs to immune-based treatments—and map out a clear path forward with a team that’s truly in your corner. If you want to understand more about how we use the body's own defenses against cancer, you can find more information in our detailed guide on immunotherapy.
You deserve a team that combines deep expertise with genuine compassion. Let us help you navigate what comes next with confidence.
Your Questions About Breast Cancer Recurrence, Answered
A recurrence can feel like you're starting all over again, and it’s natural for a wave of new questions to surface. Let’s walk through some of the most common concerns that come up when facing this next chapter.
Will My Treatment Be the Same as the First Time?
Almost certainly not. Think of it this way: the cancer you're facing today isn't necessarily the same one you fought before. Cancers can evolve, and the treatment plan has to evolve right along with it.
Your oncologist will insist on a new biopsy, and for good reason. The biological fingerprint of the cancer—its hormone receptor status (ER/PR) or HER2 status—may have changed. This fresh information, combined with where the cancer has returned, forms the blueprint for your new treatment strategy. You might find yourself on completely different chemotherapy drugs, or exploring targeted therapies and immunotherapies that weren't on the table the first time around.
Can Lifestyle Changes Prevent Another Recurrence?
While there's no magic diet or workout that can guarantee cancer won't come back, building a healthy lifestyle creates a much stronger foundation for your body to thrive. It's one of the things you can actively control.
Focusing on these key areas can make a real difference:
- Maintaining a healthy weight to keep your body's systems in balance.
- Getting regular physical activity to boost your immune function and energy levels.
- Eating a nutrient-dense diet packed with fruits, vegetables, and whole grains.
- Limiting alcohol, which is a known risk factor for breast cancer.
These choices aren't just about risk reduction; they're about improving your quality of life and helping you better tolerate treatment. Always run any major lifestyle changes by your oncology team to make sure they're right for you.
What Is the Difference Between Surveillance and Active Treatment?
It’s easy to mix these up, but they represent two very distinct phases of your care journey.
Surveillance is the "watchful waiting" phase after your first round of treatment is complete. It’s a proactive monitoring plan with regular check-ups, physical exams, and imaging tests, all designed to catch any sign of recurrence at the earliest possible moment.
Active treatment, on the other hand, kicks in only after a recurrence has been officially confirmed by something like a biopsy. This is when you start therapies—like radiation, chemotherapy, or targeted drugs—that are meant to directly fight and control the cancer that has returned. Simply put, surveillance is about watching, while active treatment is about fighting.
At Hirschfeld Oncology, we focus on developing clear, personalized roadmaps for complex and recurrent cancers. To learn about the most compassionate and advanced care options available for you here in New York City, we invite you to explore our approach on our blog.





.png)


.png)
.png)




