If you’re dealing with sudden, intense waves of heat during your cancer journey, you’re in very good company. These cancer hot flashes are a disruptive, yet common, side effect of many treatments. Think of it as a glitch in your body's internal thermostat—and understanding why it happens is the first step toward getting relief.
What Are Cancer Hot Flashes?
Your body has a sophisticated thermostat in the brain called the hypothalamus. Its main job is to keep your internal temperature perfectly balanced. But certain cancer treatments, especially those that mess with your hormones, can throw a wrench in the works.
This interference scrambles the signals, making your thermostat mistakenly think you're overheating. In response, it triggers a powerful, full-body emergency cool-down. That’s the hot flash.
The Physical Experience of a Hot Flash
While everyone experiences them a little differently, hot flashes tend to follow a familiar pattern. Knowing what to expect can make them feel a little less jarring when they strike.
- Sudden Heat: An abrupt, overwhelming feeling of warmth that seems to radiate from the inside out, typically starting in the chest and moving up to your neck and face.
- Flushing and Redness: Your skin may look visibly red or blotchy as blood vessels widen to release heat.
- Sweating: This can be anything from a light sheen of perspiration to drenching sweats as your body tries to cool itself down fast.
- Increased Heart Rate: It’s common to feel your heart pounding or beating more rapidly than usual.
- Post-Flash Chills: Once the heat subsides and the sweat evaporates, you can be left with a sudden, bone-deep chill that might even cause you to shiver.
The whole episode can be over in a few seconds or last for several minutes. It's incredibly unsettling, especially when it interrupts sleep or important moments in your day. Managing these symptoms is a crucial part of your overall care, and our guide on living well during cancer treatment offers more strategies.
More Than Just Menopause
It’s easy to dismiss these as just a version of menopausal hot flashes, but that isn't the full picture. While the underlying mechanism—hormonal shifts—is similar, the ones caused by cancer treatment are often much more intense and frequent. They represent a unique clinical challenge that requires a specialized approach.
A landmark study found that a staggering 76% of cancer survivors reported having hot flashes within a 24-hour period. Not only is this rate much higher than in the general population, but the symptoms are also consistently reported as being far more severe. Learn more about the unique challenges cancer survivors face.
This isn't just in your head. The data confirms what so many of our patients tell us: cancer-related hot flashes are a significant medical side effect, not a minor inconvenience. They deserve serious attention and a solid management plan from your oncology team.
Why Your Cancer Treatment Triggers Hot Flashes
Think of your body's internal thermostat, a little control center in your brain called the hypothalamus. It works around the clock to keep your temperature just right. The key to its smooth operation? Hormones, especially estrogen and testosterone, which act as its most trusted messengers.
When hormone levels are stable, your internal thermostat has a wide, comfortable range to work with. But many cancer treatments cause a sudden, sharp drop in these hormones. It's like the thermostat’s sensitivity gets cranked to the max—suddenly, even a tiny, normal shift in body temperature is misinterpreted as a major overheating event. This false alarm triggers the intense, all-hands-on-deck cool-down response we know as a hot flash.
This is what that chain reaction looks like—from the initial trigger to the physical response.
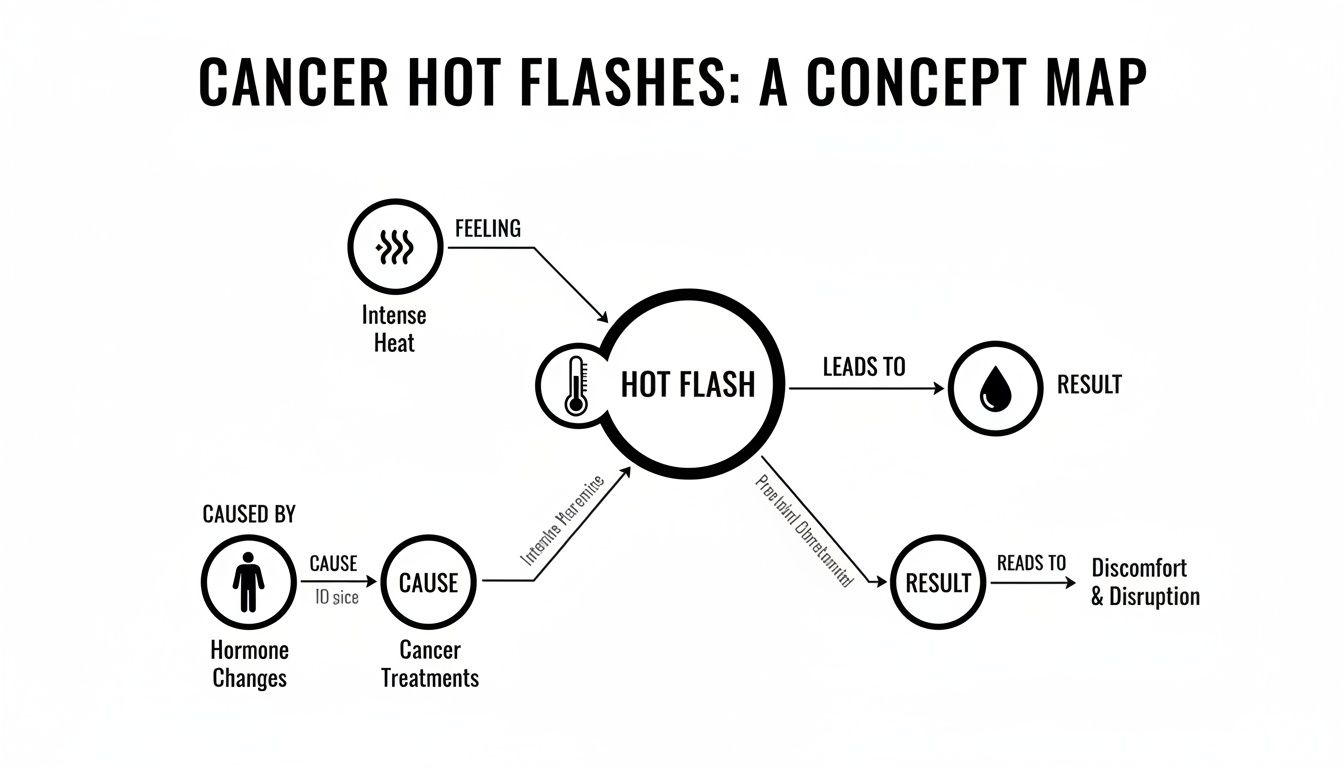
As the visual shows, a disruption to your body's temperature regulation (the cause) creates that sudden wave of heat (the feeling), which then kicks off physiological responses like sweating and flushing (the result).
Is It the Treatment or the Disease?
Many people understandably worry that hot flashes are a sign of the cancer itself. The good news is, that's incredibly rare. The vast majority of the time, hot flashes are a direct side effect of the very treatments working to fight the cancer. This is an important distinction because it helps us connect the symptom to a specific cause, which is the first step toward managing it.
So, how exactly do these treatments throw the system off-kilter?
- Chemotherapy: Some chemo drugs can affect the ovaries or testes, causing hormone production to plummet. This can happen temporarily or permanently, triggering what’s often called "treatment-induced menopause" or "andropause."
- Hormone (Endocrine) Therapy: This is one of the biggest culprits, particularly for breast and prostate cancers. Treatments like tamoxifen for breast cancer or androgen deprivation therapy (ADT) for prostate cancer are designed to block or lower hormones. An unavoidable side effect of this life-saving action is the disruption of your body’s temperature controls.
- Ovarian Suppression or Removal: For some women, surgically removing the ovaries (oophorectomy) or using medications to shut them down is part of the treatment plan. This causes an immediate and dramatic drop in estrogen, often leading to sudden, intense hot flashes.
- Targeted Therapies & Immunotherapies: While it’s less common, some newer, more advanced treatments can also interfere with hormonal pathways in ways that lead to these symptoms.
Just how common is this? For patients on hormone therapies, it's incredibly prevalent. Studies on breast cancer survivors, for example, show that hot flash rates can range anywhere from 32.5% to 82.9%, depending on the specific drug. You can see the detailed research on treatment-induced symptoms to get a clearer picture of this variation.
How Different Therapies Interfere with Hormones
Let's take a closer look at how some of these therapies trigger hot flashes. Understanding the "why" behind your symptoms can make them feel less random and give you more confidence when you talk to your oncology team.
Here’s a quick breakdown connecting common treatments to their impact on hormones.
Common Cancer Treatments and Their Link to Hot Flashes
Knowing which treatment is causing the issue is key, as it allows your care team to suggest management strategies tailored to your specific situation.
Hot flashes are not just a minor annoyance; they are a direct physiological consequence of your cancer therapy doing its job on a hormonal level. Recognizing this link is the first step toward finding effective relief and reclaiming your quality of life.
Your oncology team has guided countless patients through this exact experience. By pinpointing the cause, you and your doctor can work together to explore solutions. Understanding the "why" empowers you to ask the right questions and advocate for the symptom relief you deserve.
Practical Strategies for Managing Hot Flashes

Knowing why you're having cancer hot flashes is one thing, but getting real relief is what truly gives you your life back. This is your practical toolbox, packed with proven strategies to cool things down and help you feel more in control. We'll walk through everything from non-hormonal medications your oncologist might recommend to powerful lifestyle shifts you can start making today.
The whole idea is to either help your body’s internal thermostat find its balance again or to manage the triggers—both internal and external—that set off an episode. The end goal is to build a personalized plan that works for you, giving you a range of solid options to discuss with your care team.
Non-Hormonal Prescription Medications
For many people, especially those with hormone-sensitive cancers where Hormone Replacement Therapy (HRT) is off the table, non-hormonal medications can be a game-changer. These aren't just covering up the symptoms; they work on the same nerve pathways that your scrambled thermostat is using.
Your oncologist might bring up a few different options:
- Certain Antidepressants (SSRIs/SNRIs): Medications like venlafaxine are often a first-line choice. They influence brain chemicals like serotonin and norepinephrine, which have a hand in regulating body temperature. Think of them as helping to recalibrate your internal thermostat, making it less prone to overreacting.
- Gabapentin: While it was first developed for nerve pain and seizures, gabapentin has proven to be surprisingly effective at dialing down the frequency and intensity of hot flashes. It essentially helps to quiet the faulty nerve signals that create that sudden wave of heat.
- Clonidine: This is actually a blood pressure medication, but it can help by keeping blood vessels more stable, so they're less likely to dilate suddenly and cause that intense flushing.
- Oxybutynin: More commonly used for an overactive bladder, this drug can also reduce sweating and, for some people, provides relief from hot flashes.
It is absolutely crucial that you never start a new medication without getting the green light from your oncologist. They are the only ones who can weigh your specific cancer type, current treatments, and overall health to find the safest, most effective choice for you.
Lifestyle and Behavioral Adjustments
Beyond medication, you have an incredible amount of power to manage cancer hot flashes through your daily habits. This is all about creating a cooler, more stable personal environment to head off triggers before they start and lessen the intensity of a hot flash when one does hit. These adjustments are the foundation of any good symptom management plan.
And for so many, these symptoms are a constant presence. For breast cancer survivors on endocrine therapy, hot flashes are one of the most common side effects. One study found that about 45% of survivors had a hot flash in the last 24 hours, and 52% experienced them in the past week—averaging nearly two episodes a day. It’s no wonder that finding ways to proactively manage them is so important.
Creating Your Cooling Toolkit
Think of this as assembling your personal anti-hot-flash arsenal.
- Dress in Layers: Stick with lightweight, breathable fabrics like cotton, bamboo, or linen. When you feel a flash coming on, you can quickly shed a layer to cool down fast.
- Stay Hydrated with Cool Drinks: Sipping on iced water or other cold drinks all day helps keep your core body temperature lower. It’s also a good idea to steer clear of triggers like hot coffee or tea.
- Master Paced Breathing: The moment you feel a hot flash starting, try slow, deep belly breathing. Inhale slowly through your nose for a count of five, then exhale just as slowly through your mouth. This simple act can calm your nervous system and sometimes take the edge off the episode.
- Optimize Your Sleep Environment: Night sweats are more than just annoying; they can completely wreck your sleep. Keep your bedroom cool with a fan or an open window. Investing in moisture-wicking pajamas and bedding can also make a world of difference. You might even want to look into the best bed sheets for hot sleepers designed specifically to regulate temperature.
Your environment is a powerful tool. By proactively managing room temperature, clothing, and bedding, you are reducing the number of potential triggers your body is exposed to, giving your internal thermostat a much-needed break.
Complementary Therapies and Mind-Body Practices
Finally, many people find that adding complementary approaches to their routine provides another layer of relief. These methods tap into the mind-body connection, helping to lower stress and potentially dial down the physiological response that triggers a hot flash.
Acupuncture: Some solid studies suggest acupuncture can help reduce how often cancer survivors get hot flashes and how bad they are. The thinking is that it helps influence neurotransmitters and promotes a deep sense of relaxation.
Cognitive Behavioral Therapy (CBT): This type of therapy helps you change how you think about and react to hot flashes. While it won't make them disappear, CBT can dramatically reduce the anxiety and distress they cause, which makes them feel far more manageable. You can learn more about improving quality of life during cancer treatment in our related guide.
As always, chat with your oncology team before starting any complementary therapies to make sure they're a safe and smart choice for your situation. By mixing and matching these practical strategies, you can build a strong defense against hot flashes and get back to feeling more comfortable and in control.
Navigating Safety with Hormone-Sensitive Cancers

When you're dealing with a hormone-receptor-positive cancer, managing cancer hot flashes requires an extra layer of caution. It's a critical point, because many of the go-to remedies for menopausal symptoms—things that might seem helpful at first glance—can actually be unsafe in this situation.
The core issue is that some cancers are "fed" by hormones. Think of estrogen-receptor-positive (ER+) breast cancer or certain types of prostate cancer. The very goal of your treatment is to block or lower the specific hormones that are fueling their growth. This is precisely why some hot flash remedies can be so risky.
The Problem with Adding Fuel to the Fire
Imagine your hormone-sensitive cancer is a small, smoldering fire. Your treatment, like hormone therapy, is designed to cut off the fire's fuel supply (estrogen or testosterone). It's a life-saving strategy that effectively starves the cancer cells.
Now, what happens if you introduce an outside source of hormones? Common remedies like Hormone Replacement Therapy (HRT), which puts estrogen right back into your system, are like pouring gasoline on that fire. It directly undermines what your cancer treatment is trying to accomplish and could potentially encourage cancer cells to grow.
This is exactly why HRT is almost always off the table for anyone with a history of hormone-sensitive cancer. The risk of recurrence is just too great.
Why Even "Natural" Supplements Can Be Risky
That "fuel to the fire" analogy doesn't stop with prescription hormones. Many over-the-counter supplements and herbal remedies marketed for hot flashes contain phytoestrogens—plant-based compounds that can mimic the effects of estrogen in your body.
Here are a few common ones to watch out for:
- Black Cohosh: While often used for menopause, its exact mechanism isn't fully understood, and there's concern it may have hormone-like effects.
- Soy Isoflavones: These are concentrated soy supplements that contain high levels of phytoestrogens.
- Red Clover: Another popular herbal remedy that's rich in phytoestrogens.
- Dong Quai: An herb frequently used in traditional medicine for hormonal balance.
Just because they're "natural" doesn't mean they're safe. Their weak estrogen-like activity might still be enough to interfere with your treatment or stimulate cancer cell activity. If you're interested in the specifics, you can learn more about the principles of cancer hormone therapy in our detailed guide.
The golden rule for managing cancer-related hot flashes is safety first. Never assume that a "natural" product is a safe product. The only way to know for sure is to get explicit approval from your oncologist for any new medication, vitamin, or supplement.
Your Oncologist Is Your Safety Net
It's easy to feel overwhelmed when trying to manage side effects, but you are not in this alone. Your oncology team is your most valuable resource and your ultimate safety net. They have a deep understanding of your specific cancer, your treatment plan, and which interventions are truly safe for you.
Before you try anything new—whether it's a tea, a supplement, or something a friend recommended—run it by your doctor. This simple conversation empowers you to be an active partner in your care. It ensures your efforts to find relief don't accidentally undermine the effectiveness of your cancer treatment.
When to Talk to Your Oncology Team About Hot Flashes
Going through cancer treatment can feel overwhelming, and it’s tempting to brush off cancer-related hot flashes as just one more thing you have to put up with. But let’s be clear: managing your symptoms isn’t a luxury. It's a fundamental part of your care that directly impacts your quality of life and even your ability to stick with your treatment plan.
Knowing when to speak up is the first step toward feeling better. Most hot flashes are frustrating but not dangerous, yet there are a few situations that should be considered red flags.
Don't Wait—Call Your Team If You Experience These Symptoms
Think of these as your "stop and call" signals. If your hot flashes come with any of the following, get in touch with your care team right away:
- A fever of 100.4°F (38°C) or higher, as this could signal an infection.
- Chest pain or sudden shortness of breath, which always needs to be checked out immediately.
- Severe, uncontrollable chills or shaking, which might point to a more serious issue.
- Feeling dizzy or like you might faint, as this could be a sign of dehydration or blood pressure changes.
- A sudden, severe headache that feels different from your usual headaches.
When it comes to these symptoms, it’s always better to be safe than sorry. Your team wants to hear from you.
How to Have a More Productive Conversation
For the more routine, ongoing hot flashes, a little preparation before your appointment can make a world of difference. Walking in and saying, "I'm having hot flashes," is a starting point, but it doesn't give your team much to work with.
When you come in with specific details, you’re no longer just a patient with a complaint; you’re a partner in your own care. You're providing the clues your oncologist needs to pinpoint the best solution for you.
Think of a symptom diary as your secret weapon. It transforms your appointment from a simple report into a collaborative strategy session, helping your team understand exactly what you’re going through day to day.
This doesn't have to be complicated. A simple notebook or a note on your phone is all you need to start connecting the dots.
Tracking Your Symptoms: What Really Matters
So, what information is actually helpful? The goal is to paint a clear picture of how these hot flashes are showing up in your life. The more specific you can be, the more targeted the solutions will be.
To help you get organized, here’s a simple tracker you can fill out and bring to your next visit. It’s designed to help you communicate your experience clearly and efficiently.
Symptom Tracker for Your Next Oncology Visit
Bringing this kind of detailed information to your appointment elevates the conversation. It shows your team that hot flashes aren't just a minor annoyance—they're a real problem getting in the way of your well-being, and it’s time to find a solution together.
Let's Work Together on Your Symptom Management

As we've explored, getting a handle on side effects like cancer hot flashes isn't just an afterthought—it's a critical part of high-quality cancer care. Here at Hirschfeld Oncology, that patient-first mindset is at the heart of everything we do. We firmly believe that protecting your quality of life is just as vital as treating the cancer itself.
We start from the simple truth that no two cancer journeys are the same. A symptom that one person barely notices can completely derail another's daily life. That’s why we don’t rely on generic protocols; we focus on crafting a care plan that is truly yours.
A Team That Puts You First
Under the guidance of Dr. Azriel Hirschfeld, our team specializes in looking at the whole picture—you as a person, not just a diagnosis. From day one, we are committed to actively managing side effects like hot flashes, fatigue, or nausea. Our mission is to help you feel well enough to stay on track with your treatment and, just as importantly, live your life.
Facing these kinds of complex symptoms can feel incredibly isolating. For our neighbors in Brooklyn, Williamsburg, and Bushwick, our clinic is designed to be a local, accessible, and compassionate resource. We're here to listen, understand what you’re going through, and find real solutions that fit your life.
At Hirschfeld Oncology, we believe symptom management should be proactive, not reactive. We don't wait for side effects to become overwhelming. We work to anticipate them and get ahead of them, making your treatment journey as comfortable as we can.
This means we take the time to learn how symptoms are truly affecting you—your sleep, your work, your mood. Once we understand the impact, we can explore all the evidence-based tools available to bring you relief.
Request a Consultation and Start Feeling Better
If you're dealing with cancer hot flashes or other side effects from your treatment, please know you don't have to just push through it. There are effective strategies available, and the first step is a simple conversation. We invite you to request a consultation with our team.
Let's build a plan together that puts your comfort first. Your well-being is our priority, and we're ready to be your partner on this journey.
A Few More Questions About Cancer-Related Hot Flashes
Even after digging into the science and management strategies, you probably still have a few practical questions. That’s completely normal. Let's tackle some of the most common ones we hear from our patients every day.
Our aim here is to give you straightforward answers so you can feel more in control of what you’re experiencing.
Will My Hot Flashes Ever Go Away After Cancer Treatment?
This is the million-dollar question, and honestly, the answer is different for everyone. How long they stick around really depends on the treatment that caused them in the first place.
- If you’ve gone through chemotherapy, there's a good chance your hot flashes will slowly fade in the months after you finish. It’s a sign your body is finding its way back to its normal rhythm.
- However, if you're on a long-term endocrine therapy like tamoxifen or an aromatase inhibitor, the hot flashes are likely to be your companion for as long as you take the medication.
For some people, the symptoms can hang around even after all treatments are done. This is why it’s so important to keep an open line of communication with your oncology team. They can give you a better idea of what to expect and help you manage the symptoms for the long haul, protecting your quality of life.
Are Over-The-Counter Supplements Safe to Take?
This is a big one, and it’s a critical safety issue. Please be incredibly careful with any over-the-counter supplements marketed for hot flashes. Many of these products contain phytoestrogens—plant-based compounds that can mimic the effects of estrogen in your body.
You should NEVER take a new supplement, vitamin, or herbal remedy without getting a clear "yes" from your oncologist first. They are the only ones who can vet the ingredients and confirm they won't interfere with your treatment or your specific type of cancer.
Some common supplements that could be risky, especially if you have a hormone-sensitive cancer like ER-positive breast cancer, include:
- Black Cohosh
- Dong Quai
- Red Clover
- Soy Isoflavones
Don't let the "natural" label fool you. It doesn't automatically mean "safe." Your care team is your best resource for navigating this, so always, always ask first.
Can Men Get Hot Flashes From Cancer Treatment?
Yes, they absolutely can. It’s actually a very common side effect for men on certain treatments, especially androgen deprivation therapy (ADT) for prostate cancer.
ADT is designed to drastically lower testosterone levels. This sudden hormonal shift messes with the brain's internal thermostat in almost the exact same way a drop in estrogen does for women. The experience itself—that sudden wave of intense heat, sweating, and flushed skin—is virtually identical.
The good news? The same strategies that work for women often work just as well for men. Lifestyle changes and non-hormonal medications can be incredibly effective at managing these cancer hot flashes.
If you are struggling with hot flashes or any other side effects from your treatment, please know that you don't have to just "tough it out." At Hirschfeld Oncology, our team is built around proactive and compassionate symptom management. We invite you to explore our approach and learn more about how we prioritize patient well-being on our blog.





.png)


.png)
.png)




