When you first hear that your cancer treatment will involve both chemotherapy and radiation, it’s natural to feel overwhelmed. We find it helps to think of this approach as a strategic, coordinated attack—a "one-two punch"—designed to fight the cancer on multiple fronts.
Let's break down what each treatment does.
A Coordinated Strategy to Fight Cancer
Understanding your treatment plan is the first step toward feeling more in control of your journey. Chemotherapy and radiation are two of the most established and effective tools we have in oncology, and using them together is a powerful strategy refined over decades of research and clinical experience.
Think of chemotherapy as a systemic treatment. It travels throughout your entire bloodstream, acting like a patrol that seeks out and destroys rapidly dividing cells. Since cancer cells grow and divide much faster than most normal cells, they are especially susceptible to these drugs. This body-wide approach is vital for tackling any cancer cells that might have broken away from the original tumor.
Radiation therapy, on the other hand, is all about precision. It’s a localized treatment that uses high-energy beams, like a highly focused spotlight, to damage cancer cells in one specific area. By zeroing in on the tumor itself, we can deliver a powerful, destructive dose while doing our best to spare the healthy tissue surrounding it.
Here’s a quick look at how they differ:
Chemotherapy vs. Radiation At a Glance
This table highlights the core differences between these two powerful treatments, showing how their unique strengths complement each other.
By combining a systemic treatment with a localized one, we can attack the cancer from the inside out and the outside in, leaving it with fewer places to hide.
Why Two Treatments Are Better Than One
So, why not just use one or the other? Combining chemo and radiation isn't just about doubling up on the attack; it's about creating a synergistic effect where each treatment makes the other work better. A key goal here is something we call radiosensitization.
In simple terms, certain chemotherapy drugs can make cancer cells more sensitive and vulnerable to radiation. This means the radiation can do a better job of destroying the tumor than it ever could on its own.
This one-two punch can lead to significantly better results. It can shrink tumors more effectively, wipe out microscopic cancer cells that might otherwise be left behind, and ultimately improve the chances of a successful outcome.
These combined strategies are more critical than ever. In 2022, there were an estimated 20 million new cancer cases worldwide. With that number expected to climb in the coming decades, refining and mastering effective combination treatments is a global priority. You can learn more about the global cancer burden from the World Health Organization.
The Strategy Behind Combining Treatments
When your oncology team suggests combining chemotherapy and radiation, the thinking behind it is simple: synergy. We're not just throwing two different treatments at the cancer; we're using them in a coordinated way to make each one more powerful than it could be on its own. The idea is to create a one-two punch that cancer cells can't withstand.
This combination is often called chemoradiotherapy or chemoradiation. The strategy works because each treatment has a unique job. Chemotherapy is a systemic treatment, meaning it travels through your bloodstream to weaken cancer cells wherever they are. Radiation, on the other hand, is a highly focused, local treatment that delivers a powerful blow directly to the tumor.
This infographic helps visualize how these two very different approaches work together.
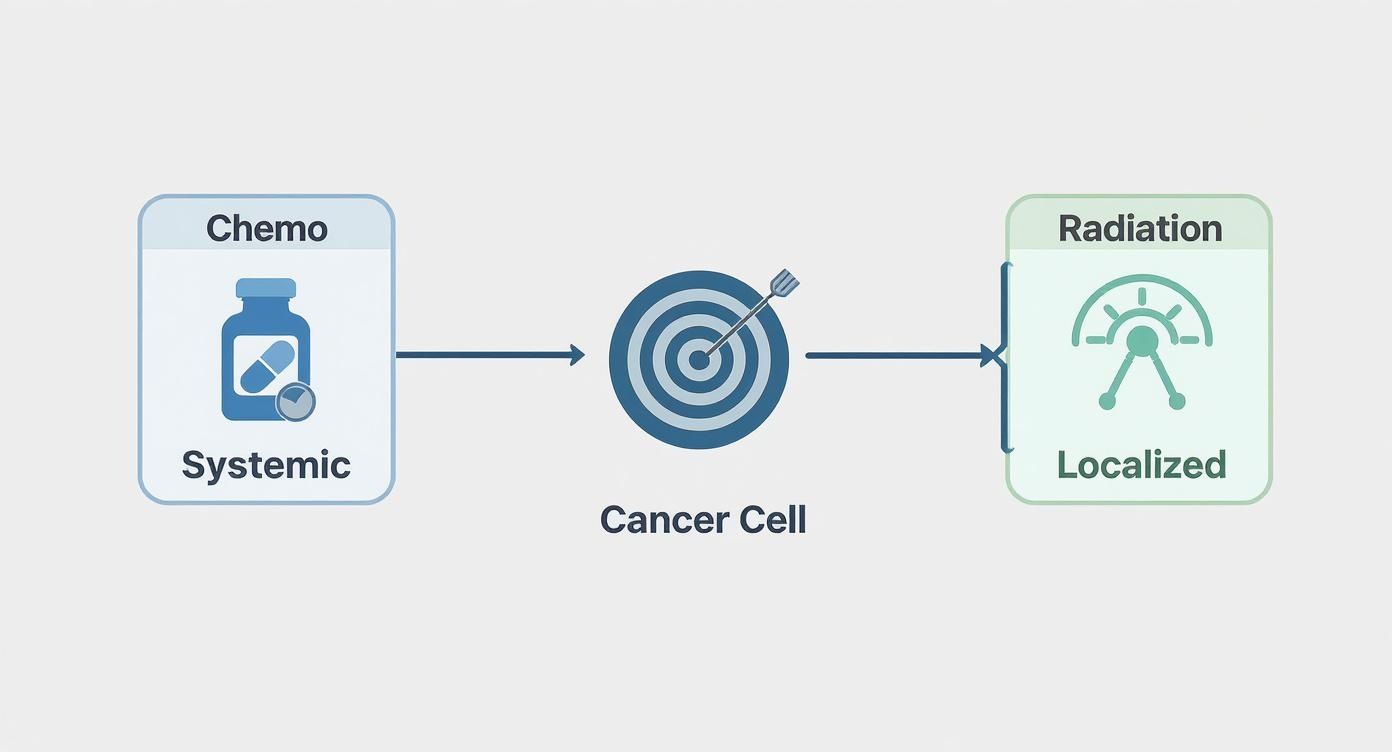
As you can see, the chemo provides a body-wide net, while the radiation acts like a sniper, hitting the main target with precision. Together, they leave the cancer with nowhere to hide.
Concurrent vs. Sequential Approaches
So, how is this actually scheduled? Your care team will map out the timing in one of two ways, and the choice depends entirely on what will be most effective for your specific situation.
- Concurrent Therapy: This is when we give you both treatments at the same time. You might have radiation therapy every weekday for several weeks, with chemotherapy infusions scheduled on certain days within that same period. The big advantage here is that the chemo drugs can make cancer cells more sensitive to the radiation, essentially priming them for the hit. It's a more intense approach, but for many cancers, it's also more effective.
- Sequential Therapy: Here, we do one treatment first, then the other. For instance, you might go through a full course of chemotherapy over a few months to shrink the tumor and hit any stray cells. After you’ve had some time to recover, you’ll start your course of radiation to finish the job on the main tumor site.
The decision between these two timing strategies is carefully considered based on the type of cancer you have, its stage, and our overall goals for your treatment.
Defining the Goal of Your Treatment
The "why" behind combining chemo and radiation is just as important as the "how." The purpose can change depending on where you are in your cancer journey. Your treatment plan will be designed to achieve one of three main objectives.
The purpose of combining therapies is to achieve a specific outcome. This could be shrinking a tumor to make it operable, destroying any cancer cells left after surgery, or serving as the primary curative treatment itself.
Knowing the intent behind your treatment is empowering. Here’s what these goals look like in practice:
- Neoadjuvant Therapy: Think of this as treatment before the main event, which is usually surgery. The goal is to shrink a tumor to make it smaller and more manageable for the surgeon to remove. This can lead to a more successful surgery and sometimes even a less invasive procedure.
- Adjuvant Therapy: This is treatment given after surgery. Even after a tumor is removed, microscopic cancer cells can be left behind. Adjuvant chemoradiation is designed to hunt down and destroy these remaining cells to lower the chances of the cancer coming back.
- Primary or Definitive Therapy: For some cancers, especially those in difficult-to-reach places, combined chemo and radiation is the main treatment. The goal here is to cure the cancer without any surgery at all.
These strategies are powerful, but they’re just one part of the modern cancer-fighting toolkit. If you're curious about how they stack up against other modern treatments, our guide on the differences between targeted therapy and chemotherapy offers some great perspective.
The most important thing is to talk with your Hirschfeld Oncology team. We will always walk you through the logic behind your personal care plan, making sure you understand every step we take together.
Cancers Often Treated with Combined Therapy

It’s one thing to understand the theory behind combining chemo and radiation, but it really clicks when you see how this strategy is used for specific diagnoses. This powerful combination is a true cornerstone of modern cancer care. It's become the standard of care for many cancers where we need to fight on two fronts—locally and system-wide—to achieve the best possible outcome.
This combined approach, which we often call chemoradiation, has led to huge leaps in survival rates and treatment success. With projections showing over 2 million new cancer cases in the U.S. by 2025, having proven, effective combination therapies is more critical than ever. We’ve seen this approach make a profound difference for cancers of the cervix, head and neck, and certain lung cancers, significantly improving 5-year survival for patients with locally advanced disease. You can explore more on the progress in cancer treatment.
Let's walk through some of the specific cancers where we frequently rely on this dual-action therapy.
Head and Neck Cancers
When cancer develops in the mouth, throat, sinuses, or voice box, we often turn to combined therapy. These are incredibly complex areas packed with critical structures, making surgery difficult—and sometimes impossible—without impacting a person's ability to function normally.
For many head and neck cancers, combined chemoradiation is the primary, definitive treatment. The goal is to wipe out the cancer completely while preserving vital functions like speech and swallowing, which major surgery might compromise.
The chemotherapy works to weaken cancer cells and shrink the tumor, which essentially sets them up for the radiation to deliver a more powerful, lethal blow. This approach gives us a much better chance at preserving crucial organs and function, leading to a better quality of life after treatment.
Lung Cancer
For certain types of lung cancer, especially non-small cell lung cancer (NSCLC) that hasn’t spread to distant parts of the body but can’t be removed surgically, concurrent chemoradiation is the gold standard.
Here’s why it works so well:
- Targeting the Main Tumor: Radiation delivers a high-energy, focused attack directly on the tumor sitting in the lung.
- Catching Any Escapees: Meanwhile, chemotherapy travels through the bloodstream to hunt down and destroy any cancer cells that might have broken off and traveled to nearby lymph nodes.
- A Synergistic Punch: When you give both treatments together, the effect is greater than the sum of its parts. They amplify each other's power.
The goal with this strategy is to cure the cancer in patients who have locally advanced disease.
Cancers of the Digestive System
Several gastrointestinal (GI) cancers respond incredibly well to the one-two punch of chemo and radiation. This is particularly true for tumors that are embedded in tissues where it's tough for a surgeon to get clean margins.
Esophageal Cancer
For cancer in the esophagus, we often use chemoradiation before surgery (a neoadjuvant approach) to shrink the tumor. This can make the surgeon's job easier and more effective. In some situations, this combined treatment is powerful enough to be the definitive therapy, allowing a patient to avoid surgery altogether.
Rectal Cancer
Similarly, rectal cancer is very frequently treated with chemoradiation before surgery. The pelvic region is a tight space, and shrinking the tumor first gives the surgeon a better shot at removing it completely while sparing the delicate nerves that control bladder and sexual function. It also dramatically lowers the chances of the cancer coming back in that area.
Anal Cancer
For anal cancer, combined therapy is now the primary treatment. The results are so effective that it has largely replaced surgery as the first line of defense, curing the majority of patients while preserving normal sphincter function—a huge win for long-term quality of life.
At Hirschfeld Oncology, we customize every treatment plan, ensuring the strategy we choose is the right fit for your specific diagnosis, your overall health, and your personal goals.
Managing Your Well-Being During Treatment

Let's be direct: combining chemo and radiation is a powerful one-two punch against cancer, but it's also demanding on your body. Our absolute priority is to help you maintain your comfort and quality of life throughout the process.
Feeling in control starts with knowing what to expect and having a plan. Remember, you are the most important person on your care team. The more openly you can communicate how you're feeling, the better we can support you every step of the way.
Taming Treatment-Related Fatigue
Fatigue during cancer treatment isn't just regular tiredness. It's a deep-seated exhaustion that sleep doesn't always fix, and it's incredibly common—affecting around 80% of people. This is a sign that your body is working hard, so the best thing you can do is listen to it.
Fighting it rarely works. Instead, we encourage you to work with it. It might sound strange, but a short, slow walk can often be more energizing than staying in bed all day.
Here are a few practical ways to manage your energy:
- Prioritize Ruthlessly: What really needs to get done today? Let the rest go. This is the time to lean on your support system for help with groceries, chores, or errands.
- Schedule Your Downtime: Plan for short naps or quiet rest periods throughout your day, especially on days you have treatment.
- Fuel and Hydrate: Dehydration is a huge energy drain. Keep a water bottle with you at all times and focus on small, nutrient-rich meals and snacks to keep your tank from running on empty.
Soothing Your Skin After Radiation
Radiation is precisely targeted, but the skin in the treatment area often becomes red, sensitive, or irritated—much like a sunburn. This is a completely normal reaction. Starting a gentle skincare routine from day one can make a world of difference.
Your radiation oncology nurse will give you very specific instructions, and those are your most important guide.
Our Golden Rule for Skincare: Treat the skin in the treatment area as if it were brand new baby skin. That means no harsh soaps, no scrubbing, no extreme hot or cold water, and no tight clothing.
For a deeper dive, our guide on the adverse effects of radiation therapy offers more detailed tips for proactive management.
Proactively Managing Nausea
Chemotherapy has a reputation for causing nausea, but modern medicine has given us excellent tools to manage it. While over 70% of patients still experience some nausea, we can usually stay ahead of it.
The key is prevention. Take your anti-nausea medications exactly as prescribed, even when you’re feeling fine. It is always easier to prevent nausea than it is to stop it once it has started.
A few dietary adjustments can also help:
- Graze, Don't Gorge: An empty stomach can make nausea worse. Try five or six small snacks or mini-meals throughout the day instead of three big ones.
- Keep it Bland: When you feel queasy, stick to simple foods like toast, rice, crackers, or chicken broth. Greasy, spicy, or very sweet foods can be triggers.
- Sip Slowly: Soothing liquids like ginger ale, peppermint tea, or plain water can help. Try drinking between meals rather than with them so you don't get too full.
Caring For Your Mouth and Throat
Both chemo and radiation (especially to the head and neck) can lead to mouth sores, dryness, or changes in taste. This condition, called mucositis, can make eating a real challenge. Your best defense is a great oral hygiene routine.
Use a toothbrush with very soft bristles to gently clean your teeth and gums after you eat and before bed. Rinsing your mouth several times a day with a simple saltwater or baking soda solution (ask us for the recipe) can also keep it clean and moist, which helps prevent sores from forming.
If you start to feel any significant pain, tell your team at Hirschfeld Oncology right away. We have prescription mouthwashes and other treatments that can bring you relief.
This table gives a quick overview of some common challenges and how you can get ahead of them.
Common Side Effects and Management Strategies
Remember, these are just general guidelines. Your experience will be unique, and your care team is here to tailor a specific plan to keep you as comfortable as possible.
What to Expect on a Typical Treatment Day

Heading into your first combined chemo and radiation treatment can feel daunting, but knowing what the day will look like can make a world of difference. It helps replace the unknown with a predictable rhythm. While your schedule is tailored specifically to you, most treatment days follow a similar pattern of check-ins, appointments, and coordination. Let's walk through it together, so you can focus your energy on what truly matters—your health.
Your care team will be your partner in scheduling. For concurrent therapy, it’s common to have radiation much more often (usually daily, Monday through Friday) while chemotherapy is less frequent (maybe once a week or every few weeks). It sounds like a lot to juggle, but our patient navigators are experts at creating a schedule that’s as smooth and manageable as possible for you.
You're not alone on this path. In fact, by 2025, it's estimated that nearly 19 million people in the U.S. will be cancer survivors, a testament to the effectiveness of modern treatments like this. Incredible advances have made combined therapies more precise and the patient experience more supported than ever before. You can read more about the evolution of multimodal cancer treatment plans and the progress we've made.
Arriving for Your Appointments
Your day will start with a simple check-in at the front desk. From there, you'll likely meet with a nurse who will take your vital signs—your temperature, blood pressure, and weight—and, most importantly, ask how you’re feeling.
This check-in is your time to speak up. It’s the perfect moment to share any new or changing side effects you've noticed, no matter how small they seem. Honest, open communication is your best tool for staying ahead of symptoms. If chemotherapy is on the agenda, you might also have a quick blood draw to make sure your blood counts are in a safe range for treatment.
The Chemotherapy Infusion Process
If it’s an infusion day, you’ll be welcomed into our comfortable infusion center. A highly skilled oncology nurse will either place a small IV in your arm or hand or access your existing port. The chemotherapy medicine is then delivered slowly and carefully through the IV.
The length of an infusion isn't one-size-fits-all. It can range from just 30 minutes to several hours, depending entirely on the specific medications in your personalized plan.
Our goal is to keep you comfortable during this time. Feel free to read a book, listen to music, or just rest. Your nurse will be keeping a close eye on you throughout the entire process. For more ideas on how to make this time easier, take a look at our guide on how to prepare for chemotherapy.
Your Radiation Therapy Session
Compared to an infusion, the radiation session itself is quite fast. A radiation therapist will greet you and help you get into the precise position on the treatment table. They’ll use the small, tattoo-like marks made during your planning session to align the machine perfectly.
Once you're ready, the team will step out of the room, but they will be watching and listening the entire time. The machine will then deliver the radiation beam—it’s completely invisible and painless. While the whole appointment might take 15 to 20 minutes, the actual radiation is only on for a few minutes of that time.
What to Bring for Your Treatment Day
A little preparation goes a long way in making your treatment days less stressful. Think about packing a small "comfort bag" with a few things to help you feel more at ease.
- Comfort Items: A soft blanket, warm socks, or a favorite scarf can make the clinic feel a bit more like home.
- Entertainment: A good book, a tablet with movies, or headphones for music can help the time fly by during infusions.
- Snacks and Water: It's smart to pack light, bland snacks (like crackers or pretzels) and a water bottle to stay hydrated and ward off nausea.
- A Notebook: Use it to jot down questions as they come to you or to track symptoms you want to discuss with your team.
- A Friend or Family Member: Bringing a loved one for company and support can make a huge difference in how you feel.
Questions to Ask Your Oncology Team
One of the most powerful things you can do is take an active role in your own care. Your appointments are more than just a time for treatment; they are a dedicated time for conversation. Coming prepared with questions is the best way to make sure you leave feeling clear, confident, and in control of your journey with chemo and radiation.
Think of us as your partners in this process. The more you ask, and the more you share, the better we can support you. Remember, when it comes to your health and peace of mind, there's no such thing as a small or silly question.
Questions About Your Treatment Plan
It’s so important to understand the “why” behind your care plan. These questions can help shed light on the goals and the specific details of your combined therapy.
- What is the main goal of combining chemo and radiation for my cancer? Are we aiming for a cure, or is the focus on managing symptoms?
- Will my treatment be concurrent or sequential? I'm curious why that specific approach was chosen for me.
- Could you tell me the names of the chemotherapy drugs I'll be receiving and how they'll be administered?
- How many weeks will this treatment last, and what will my day-to-day schedule look like?
Having these conversations ensures that you and your care team are perfectly aligned on the goals of your treatment. This shared understanding is the foundation of a strong patient-doctor partnership.
Questions About Managing Side Effects
Getting ahead of side effects is one of the best ways to protect your quality of life during treatment. Knowing what to watch for—and when to speak up—can make a world of difference in how you feel from one day to the next.
Ask your nurse or doctor:
- Based on my specific chemo and radiation plan, what are the most common side effects people experience?
- Which symptoms are urgent? What should I look for that would require me to call the office right away, even after hours?
- Are there any specific creams, mouth rinses, or over-the-counter medications you recommend I have at home before I even start?
Questions About Daily Life and Logistics
Treatment will naturally become a big part of your daily routine, so it helps to know how it might affect your life outside the clinic. Asking these questions can help you and your family plan for the weeks ahead.
- Are there any dietary restrictions I need to know about? On the flip side, are there any foods I should try to eat more of?
- Can I continue to work, exercise, or enjoy my hobbies during this time? What changes might I need to make?
- Between my appointments, who is the best person on the team to contact if I have a non-urgent question?
Your Treatment Questions, Answered
Going through combined chemo and radiation understandably brings up a lot of questions about what to expect day-to-day. We've gathered some of the most common concerns we hear from our patients to give you straightforward answers and help you prepare for the road ahead.
Can I Still Work During Chemo and Radiation?
Many people do, but it nearly always involves making some changes. Whether you can keep up with your usual work routine really depends on a few things: how physically demanding your job is, how intense your treatment schedule is, and—most importantly—how you're feeling. Fatigue is a very real side effect, and it can make a full-time schedule feel impossible some days.
It’s a great idea to have an open conversation with your employer ahead of time. You might discuss a more flexible schedule, working from home, or reducing your hours. Letting us, your oncology team, know about your job also helps us manage side effects that could get in the way of you performing at your best.
How Long Until I Feel "Normal" Again After Treatment?
Recovery doesn't happen overnight; it’s a gradual process that is unique to every single person. Some side effects, like nausea, tend to clear up within a few days or weeks of your last treatment. Fatigue, however, is a different story. It can stick around for weeks or even months as your body puts all its energy into healing.
"Feeling normal" is a deeply personal benchmark. Your health before treatment, the specific drugs and radiation doses you received, and your body's own pace of healing all factor into how quickly you'll bounce back.
We can give you a more personalized timeline based on your specific treatment plan. We might also suggest supportive care like physical therapy, nutritional counseling, or survivorship programs to help you get your strength and energy back.
What Is the Difference Between Curative and Palliative Care?
The main difference comes down to the primary goal of the treatment itself.
- Curative Treatment: The aim here is to get rid of the cancer entirely, hoping for a long-term remission or a cure. To do this, we often use more intensive doses of chemo and radiation to give us the best chance of destroying all the cancer cells.
- Palliative Treatment: This approach is all about improving your quality of life by managing symptoms. The goal isn’t to cure the cancer, but to relieve pain, pressure, or other problems a tumor is causing. For example, palliative radiation might use lower doses for a shorter time just to shrink a tumor and make you more comfortable, which usually comes with fewer side effects.
Will I Definitely Lose My Hair?
This is one of the first things people worry about, but hair loss doesn't happen to everyone. It completely depends on the specifics of your treatment.
Some chemotherapy drugs are known to cause hair loss all over your body—head, eyebrows, the works—because they affect all fast-growing cells. But many other chemo drugs don't have this effect at all.
Radiation is much more localized. It only causes hair loss in the specific, targeted area being treated. If you’re receiving radiation to your hip, the hair on your head will be completely unaffected. The best thing to do is ask your oncologist directly about the likelihood of hair loss with your specific drugs and radiation plan.
At Hirschfeld Oncology, we know that clear, honest communication is the foundation of great care. If other questions come to mind or you'd like to discuss a treatment strategy designed just for you, we encourage you to request a consultation through our official blog.





.png)


.png)
.png)




