Receiving a stomach cancer diagnosis is overwhelming, and one of the first questions that usually comes to mind is, "What does chemotherapy really mean for me?" Simply put, chemo for stomach cancer is a cornerstone of treatment that uses powerful drugs to find and destroy cancer cells throughout your body.
It’s the main line of attack against cancer cells, no matter where they might be hiding.
Understanding Chemotherapy's Role in Stomach Cancer Treatment
Chemotherapy is what we call a systemic treatment. This means the medicine travels through your bloodstream to reach cancer cells that may have spread far from the original tumor in the stomach.
Think of it like tending to a garden. Surgery is like pulling the biggest, most obvious weed—the main tumor. Chemotherapy, on the other hand, is like a specialized treatment that works through the soil to get rid of any stray roots or seeds left behind that could sprout new weeds later on.
This is so important because stomach cancer cells are defined by their ability to grow and divide uncontrollably. Chemotherapy drugs are designed to hunt down and shut down these rapidly growing cells.
The Three Main Goals of Chemotherapy
Your oncology team will design a chemotherapy plan with one of three main goals in mind, all based on your specific cancer stage and overall health. The goal really determines when and why you'll receive chemo.
Neoadjuvant Therapy: This is chemo given before surgery. The main aim here is to shrink the tumor, which can make the surgeon's job easier and more effective. For cancers that are more advanced but haven't spread widely, this approach can dramatically improve the chances of a successful surgery.
Adjuvant Therapy: This is chemo given after surgery. The goal is to wipe out any microscopic cancer cells that might have been left behind. It acts as an insurance policy, significantly lowering the odds of the cancer coming back.
Palliative Therapy: When stomach cancer is advanced or has spread to other parts of the body (metastasized), the focus shifts. Palliative chemo is all about controlling the cancer's growth, easing symptoms like pain, and helping you maintain the best possible quality of life.
To make this clearer, let's look at how these goals fit into the treatment timeline.
The Goals of Chemotherapy for Stomach Cancer at a Glance
As you can see, chemotherapy isn't a single event but a strategic tool used at different points for very specific reasons.
The old "one-size-fits-all" model of cancer care is long gone. Your treatment is a personalized strategy, often blending several chemo drugs into a specific "regimen" and layering in other advanced therapies to build the strongest possible plan for you.
A Personalized and Evolving Field
Oncology is a field that moves incredibly fast, and research is constantly uncovering more effective ways to combine treatments. The global stomach cancer treatment market is expected to grow from USD 5.40 billion to USD 17.60 billion by 2034, a clear sign of the massive investment and innovation happening right now.
This means your care plan is more tailored than ever before. It's not about a single drug; it's about creating a smart, multi-pronged attack on the cancer. To see the bigger picture of how chemotherapy works alongside other treatments, you can explore our detailed guide on gastric cancer treatment options. This integrated approach is what truly moves the needle in improving outcomes for patients.
Common Chemotherapy Drugs and Regimens Explained
Think of chemotherapy for stomach cancer not as a single drug, but as a strategic recipe, or regimen. Each regimen is a combination of medications hand-picked for their specific strengths, designed to work in concert to attack cancer cells from different angles. The right recipe for you depends on your cancer’s stage, your overall health, and the unique biological markers on the tumor itself.
For very early-stage stomach cancers that haven't burrowed deep into the stomach wall, surgery alone might be all that's needed. In these situations, your team might decide chemotherapy isn't necessary. But once the cancer becomes more advanced, combination chemotherapy is a critical part of the game plan.
Chemo for Locally Advanced Stomach Cancer
When stomach cancer is locally advanced—meaning it has grown into deeper layers of the stomach wall or nearby lymph nodes but hasn't spread to distant organs—we often use chemotherapy both before and after surgery. The goal is twofold: shrink the tumor to make surgery cleaner and more effective, then hunt down any microscopic cells left behind.
Two of the most common and powerful regimens we use in this setting are:
- FLOT: This is a potent combination of three chemo drugs (Fluorouracil, Leucovorin, Oxaliplatin) plus a fourth drug, Taxotere (docetaxel). This four-drug "quadruplet" therapy is often considered the standard of care for patients who are healthy enough to tolerate its intensity.
- XELOX (or CAPOX): This regimen combines an oral chemotherapy pill called XELoda (capecitabine) with intravenous OXaliplatin. It’s a bit more convenient since one of the main drugs can be taken at home, which many patients find improves their quality of life during treatment.
We know these approaches work. Landmark research like the CLASSIC trial70473-5/fulltext) showed that using capecitabine and oxaliplatin after surgery significantly boosted three-year disease-free survival rates for patients with stage II-III gastric cancer. Today, chemo is a standard component in over 41.2% of hospital-based treatment plans in the US, often paired with radiation. For a closer look at these figures, you can explore the full research on stomach cancer treatment trends.
This decision tree helps visualize how oncologists map out the primary goal of chemotherapy based on a patient's specific situation.
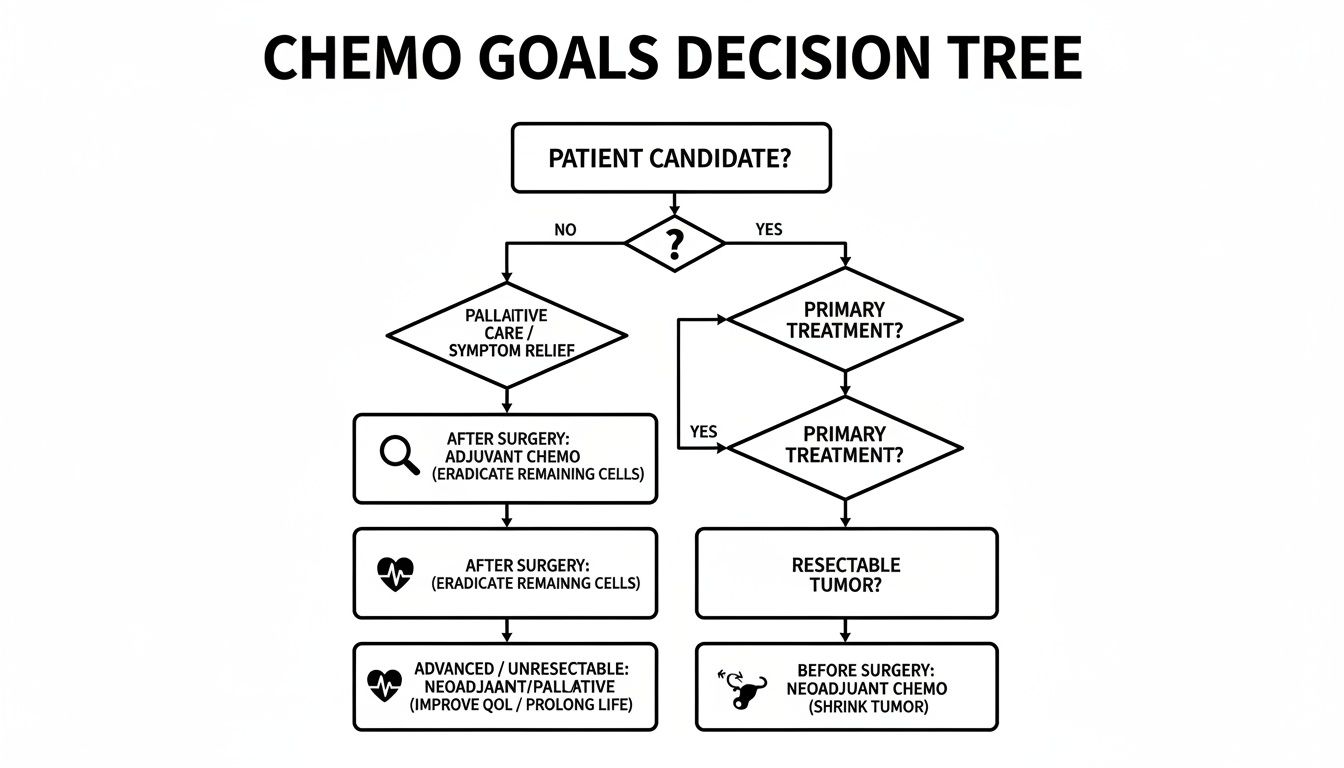
As you can see, the "why" behind chemo shifts dramatically, from getting you ready for a curative surgery to managing the disease for the long haul.
Chemo for Metastatic or Advanced Disease
When stomach cancer has spread to distant parts of the body (a process called metastasis), the primary goal of chemotherapy changes. We shift from aiming for a cure to focusing on control. This is often called palliative chemotherapy, and the goal here is to slow the cancer's growth, manage symptoms like pain or fatigue, and extend life while preserving the best quality of life possible.
Regimens for advanced disease often use platinum-based drugs like cisplatin or oxaliplatin combined with a fluoropyrimidine like 5-FU or capecitabine. We carefully balance the intensity of the regimen against its potential side effects.
The key in advanced cancer is sustainability. We need a treatment that's strong enough to keep the cancer in check but gentle enough for you to continue living your life with quality and dignity.
The Role of Biomarkers in Personalizing Chemo
Modern stomach cancer treatment goes way beyond just looking at the stage. Your oncologist will test your tumor for specific biological "flags" known as biomarkers. These flags give us crucial clues about what's fueling the cancer's growth and point us toward more effective treatments.
Think of it this way: standard chemotherapy is a general-purpose tool. Biomarkers allow us to add a specialized, high-precision instrument to the mix. Two of the most important biomarkers in stomach cancer are:
- HER2 (Human Epidermal Growth Factor Receptor 2): About 10-20% of stomach cancers make too much of a protein called HER2, which acts like a gas pedal for cancer cell growth. If your tumor is HER2-positive, we can add a targeted therapy drug to your chemotherapy.
- PD-L1 (Programmed Death-Ligand 1): This protein is a cloaking device that helps cancer cells hide from the immune system. If your tumor has high levels of PD-L1, we can combine chemotherapy with an immunotherapy drug to "unmask" the cancer, allowing your own immune system to find and attack it.
By identifying these markers, your treatment plan becomes far more personal. Instead of just getting standard chemo for stomach cancer, you might get chemotherapy plus a targeted therapy or immunotherapy. This combination strategy is often more effective than chemo alone and represents a huge step forward in how we fight this disease.
Pairing Chemo with Targeted Therapy and Immunotherapy
While chemotherapy is a foundational treatment for stomach cancer, we've learned that we can hit cancer much harder—and smarter—by not relying on chemo alone. The real breakthroughs in recent years have come from combining treatments. By pairing the broad-acting power of chemotherapy with the precision of targeted therapy and the cleverness of immunotherapy, we create a multi-pronged attack that can be far more effective, especially for advanced disease.

Targeted Therapy: The "Smart Bomb" Approach
Think of chemotherapy as a conventional bomb—it’s powerful against fast-growing cells, but it can cause collateral damage to healthy tissues nearby. Targeted therapy, in contrast, is like a smart bomb. These drugs are engineered to find and attack cancer cells based on specific molecular "markers" they possess, leaving most of your healthy cells alone.
In stomach cancer, one of the most significant markers we look for is a protein called HER2. Roughly 10-20% of stomach cancers produce far too much of this protein. When that happens, HER2 acts like a gas pedal that's stuck to the floor, telling the cancer cells to grow and divide out of control.
If testing reveals your tumor is HER2-positive, we can add a targeted drug like trastuzumab (Herceptin) to your chemotherapy. Trastuzumab is designed to hunt down the HER2 protein. It latches on, blocking the growth signal and essentially painting a target on the cancer cell for the immune system to see. This makes the accompanying chemotherapy much more effective. You can learn more about the specifics of targeted therapy and how these drugs function in our detailed guide.
By identifying these unique vulnerabilities, we can move beyond a one-size-fits-all approach. Targeted therapy allows us to design a treatment that is aimed at the specific biology of your cancer.
This precision does more than just boost chemotherapy's effectiveness; it often leads to more manageable side effects, since fewer healthy cells get caught in the crossfire.
Immunotherapy: Unleashing Your Body's Own Defenses
Another incredible tool we now have is immunotherapy. Your immune system is your body’s own security force, constantly on patrol for invaders like viruses and bacteria. The problem is that cancer cells are masters of disguise. They develop clever tricks to hide from this security force, allowing them to multiply without interference.
Immunotherapy drugs called immune checkpoint inhibitors are designed to foil these disguises. For instance, many cancer cells cover themselves with a protein called PD-L1. This protein acts as a "do not attack" signal, telling your immune cells to stand down and move along.
Drugs like nivolumab (Opdivo) and pembrolizumab (Keytruda) work by blocking that signal. They effectively unmask the cancer cells, making them visible to your immune system once again. This allows your own T-cells—the highly trained soldiers of the immune system—to finally recognize the tumor as a threat and launch a full-scale attack.
When we combine this with chemotherapy, the one-two punch is powerful:
- Chemotherapy delivers the first blow, damaging and weakening the cancer cells.
- Immunotherapy then unleashes your own immune system to move in and finish the job.
This dynamic duo is now a cornerstone of treatment for many patients with advanced stomach cancer, particularly those whose tumors show high levels of the PD-L1 marker. The combination often produces a stronger and longer-lasting response than either treatment could on its own, offering real hope and better outcomes.
Managing Common Side Effects of Chemotherapy
Let's be honest: the idea of chemotherapy side effects can be daunting. But thinking about managing them isn't about bracing for the worst—it's about being prepared and taking control. My goal, and the goal of our entire team, is to create a proactive plan that keeps you as strong and comfortable as possible, so you can stick with your treatment schedule.
Your most important tool in this process is open communication. Never hesitate to tell us what you're feeling. Nearly every side effect is temporary and can be managed with the right support, and we're here to provide that every single step of the way.

Tackling Nausea and Fatigue
Nausea and vomiting used to be the most feared parts of chemo, but thankfully, things have changed dramatically. Modern anti-nausea medications, called antiemetics, are incredibly effective. We’ll prescribe them for you to take both before and after your infusion to get ahead of any potential queasiness. The key is to prevent it, not just treat it.
Fatigue is another beast entirely. This isn't just feeling tired; it’s a profound exhaustion that a good night's sleep won't fix. It’s your body’s signal that it’s working overtime to fight cancer and heal healthy cells.
Here’s how you can push back against these two common issues:
- Graze, Don't Gorge: Try eating six to eight small snacks or mini-meals throughout the day. This keeps your stomach from getting too empty or too full, both of which can trigger nausea.
- Hydration is Non-Negotiable: Sipping on clear liquids—water, broth, even ginger ale—all day long is crucial. Dehydration is a fast track to feeling worse.
- Listen to Your Body's Cues: Some days you'll have more energy. Use them. On other days, you'll need to rest. Grant yourself that permission without any guilt.
- Embrace Gentle Movement: It sounds counterintuitive, but a short, slow walk can often do more to boost your energy than staying on the couch.
Staying on top of side effects isn't just for comfort—it's a critical part of a successful treatment plan. It helps you complete your prescribed therapy, which gives you the best possible chance at a positive outcome.
A Quick-Reference Guide to Side Effects
To help you feel more prepared, we've put together this quick-reference table. It covers the most common side effects you might experience, what they actually feel like, and some practical ways to manage them at home.
Remember, this is a general guide. Your experience will be unique, and your oncology team will be there to create a personalized plan just for you.
Addressing Mouth Sores and Taste Changes
Because chemotherapy targets fast-growing cells, the sensitive lining of your mouth can be affected. This can lead to painful sores (mucositis) or cause your sense of taste to go haywire. It's not uncommon for favorite foods to suddenly taste metallic, bland, or just plain off. This is almost always temporary.
Being proactive with your oral care can make a huge difference:
- Be Gentle: Switch to a soft-bristle toothbrush to avoid irritating your gums.
- Rinse Often: A simple rinse made with 1/2 teaspoon of salt and 1/2 teaspoon of baking soda in a cup of warm water can keep your mouth clean and soothe irritation.
- Avoid Triggers: Stay away from spicy, acidic, or hard, crunchy foods that can make sores worse. Alcohol-based mouthwashes are also a no-go.
- Get Creative: If things taste metallic, try plastic forks and spoons. If food is bland, liven it up with marinades, herbs, and spices.
For an even deeper dive, our guide on managing side effects of cancer treatment offers additional tips for patients.
Coping with Hair Loss and Neuropathy
Hair loss, or alopecia, can be one of the most emotionally difficult side effects. While not every chemotherapy drug causes it, many used for stomach cancer do. The process usually starts a few weeks after your first treatment. The good news? It's almost always temporary. Your hair will grow back.
Another potential issue is peripheral neuropathy, which is common with drugs like oxaliplatin. You might feel tingling, numbness, or a "pins and needles" sensation, usually in your hands and feet. It is absolutely crucial that you tell your care team about these symptoms right away. We can often adjust your dose to prevent the problem from becoming a long-term one. Simple things, like protecting your hands and feet from the cold, can also help.
Navigating these challenges is a team effort, and your quality of life is always our top priority as we move through your chemo for stomach cancer together.
What to Expect During Your Chemotherapy Sessions
Walking into an infusion center for the first time can be a bit overwhelming. Let’s be honest, it’s a new environment filled with unfamiliar sights and sounds. Our goal is to pull back the curtain on the process, so your treatment days feel as predictable and manageable as possible.
It all starts well before your first appointment, during a detailed chat with your oncology team. We'll lay out your entire treatment schedule—how often you’ll come in, roughly how long each session will take, and the total number of cycles you can expect. This is a great time to get practical and ask how treatment might fit in with your work, family commitments, and day-to-day life.
A Walkthrough of Your Infusion Day
While every clinic has its own rhythm, most infusion days follow a similar, well-practiced flow. Knowing the steps ahead of time can make the whole experience feel much less mysterious.
Check-In & Vitals: It starts simply at the front desk. A nurse will then get you settled, check your weight, and take your temperature, blood pressure, and pulse. Your weight is a key detail, as many chemotherapy drug doses are calculated specifically for you.
Blood Work: The next step is a quick blood draw, usually from a port if you have one, or from a vein. This isn’t just routine; it’s a critical safety measure. We’re checking your blood counts to make sure your white blood cells, red blood cells, and platelets are at a healthy enough level for you to safely receive treatment.
Oncologist Huddle: Once your lab results are back, you’ll sit down with your oncologist. This is your dedicated time to talk about how you’ve been feeling since your last visit. We need to hear about any side effects you’re experiencing, and it's the perfect chance to ask any new questions that have been on your mind.
The Infusion: With the all-clear from your doctor, you’ll be brought to a comfortable recliner in the infusion suite. A nurse who specializes in this will access your port or place an IV line. Often, you’ll receive “pre-meds” first—things like anti-nausea medication or steroids—to help head off side effects. Then, the chemotherapy infusion begins. The actual infusion time can be as short as an hour or last for several, all depending on your specific drug regimen.
Your comfort and safety are our absolute top priorities. Nurses are always nearby, keeping a close eye on everything. Never hesitate to speak up if you feel off or just need something. Think of the infusion suite as a space designed entirely for your care.
How to Prepare for a Comfortable Session
A little bit of planning can make a world of difference on infusion days. Packing a small "chemo bag" with some comforts from home can help you feel more relaxed and in control.
Here are a few things patients tell us they're glad they brought:
- Comfortable Clothes: Think soft, loose-fitting, and easy. Dressing in layers is a great strategy, since infusion centers can sometimes feel cool. A cozy sweater, warm socks, or a personal blanket can make you feel much more comfortable.
- Snacks and Drinks: We’ll have things available, but nothing beats your own favorites. Bringing a water bottle is a must, and easy-on-the-stomach snacks like crackers or pretzels are always a good bet.
- Something to Do: An infusion can take a while, making it the perfect time to get lost in a good book, listen to a podcast, or watch a movie on a tablet. Some people even bring quiet hobbies like knitting or sketching.
- A Friend or Family Member: You don’t have to do this alone. Bringing someone along provides great company and emotional support. They can also be a second set of ears, help take notes, and make sure you get home safely.
Lastly, please plan for a ride home. You’ll likely feel tired after your treatment, and it’s much safer not to drive. Arranging your transportation ahead of time means you can just focus on resting and recovering. Preparing for your chemo for stomach cancer is all about giving yourself the knowledge and tools you need to navigate the road ahead with confidence.
Your Questions Answered: Navigating Chemo for Stomach Cancer
It’s completely normal to have a million questions when you're facing a new diagnosis and treatment plan. To help you feel more confident and prepared, let's walk through some of the most common things patients and families ask about chemotherapy for stomach cancer.
How Long Does a Typical Chemotherapy Cycle Last?
The timing of your chemotherapy really comes down to the specific drug combination, or regimen, your oncologist prescribes for you. Most often, a single cycle will last anywhere from two to three weeks. For instance, a very common regimen called FLOT is given on a two-week cycle.
A "cycle" isn't just one long treatment. It usually means you'll have an infusion on one or more days, followed by a planned rest period. This break is crucial—it gives your body the time it needs to bounce back and rebuild healthy cells before the next round. A full course of treatment typically involves several of these cycles, often lasting between three and six months in total, depending on whether the goal is to shrink a tumor before surgery or manage more advanced cancer.
Can I Keep Working and Living My Normal Life During Treatment?
Many people do find a way to continue working and handling their daily routines during chemo, but it almost always requires some changes. How much it affects you depends on the drugs you're getting, your general health, and simply how your body reacts. You can pretty much count on fatigue being a major factor; it’s one of the most common side effects across the board.
It's a good idea to talk with your employer early on. Discussing the potential for a more flexible schedule, remote work options, or planned time off around your infusion and recovery days can make a huge difference.
The secret to maintaining your quality of life is learning to prioritize rest, being willing to accept help from friends and family, and keeping an open line of communication with your medical team.
What Happens If the First Chemo Regimen Doesn’t Work?
If the first combination of drugs—what we call "first-line" therapy—isn't shrinking the cancer as much as we’d like, or if the cancer starts growing again, it’s not a dead end. Not by a long shot. This is a signal for your oncologist to re-evaluate and pivot. That usually involves new scans and sometimes re-testing the tumor for biomarkers to see if its biological profile has changed.
Luckily, we have a number of other avenues to explore. These often include:
- Second-Line Therapy: We switch to a different set of chemotherapy drugs that work in a different way, giving us a fresh angle of attack.
- Third-Line Therapy: If the cancer is particularly stubborn, there are sometimes third-line drug combinations that can be effective.
- Clinical Trials: This is a fantastic option to consider. You may be a great candidate for a clinical trial testing newer drugs, novel combinations, or innovative approaches that aren't yet widely available.
When dealing with advanced or resistant stomach cancer, the treatment plan becomes incredibly personal. Your care team will constantly adjust the strategy based on how the cancer is responding, how you're feeling, and what the latest research shows is most promising for your specific situation.
At Hirschfeld Oncology, our focus is on creating sophisticated and individualized treatment plans for stomach cancer, from advanced targeted therapies to gentler, low-dose chemotherapy options. If you're looking for a second opinion or want to explore every possibility, we invite you to schedule a consultation with our dedicated team. You can learn more about our approach and get in touch on our blog.





.png)


.png)
.png)




