When you first hear the words "stomach cancer," it's completely normal to feel like your world has been turned upside down. But knowledge is power, and getting a firm grasp on the road ahead can bring a sense of clarity and control back into your life.
The main gastric cancer treatment options are surgery, chemotherapy, radiation, targeted therapy, and immunotherapy. Think of these as the primary tools in your oncologist's toolkit. The specific plan they create for you won't be a one-size-fits-all approach; it will be a personalized roadmap designed around your unique diagnosis.
Navigating Your Gastric Cancer Diagnosis
A gastric cancer diagnosis is the start of a new journey—one that demands courage, a strong support system, and, above all, clear information. This guide is meant to be your first step, a map to help you and your loved ones make sense of the path forward by breaking down complex medical ideas into plain English.

Those first few weeks after a diagnosis are often a whirlwind of questions and uncertainty. Our goal here is to cut through the noise, explaining the medical terms you'll encounter and the "why" behind each potential treatment. We’ll walk through the mainstays of cancer care so you can see how they work together to fight the disease.
Understanding the Core Treatment Pillars
Your oncology team has several powerful methods for treating gastric cancer. Each has a specific job, and they are often combined to give you the best possible outcome. Understanding these pillars is the first real step toward feeling more in control during conversations about your care.
The primary approaches include:
- Surgery: The goal here is the physical removal of the tumor. It’s often the go-to treatment when the cancer is caught early and hasn't spread.
- Chemotherapy: These are powerful drugs that work throughout your entire body to find and destroy cancer cells, wherever they may be.
- Radiation Therapy: This treatment uses focused, high-energy rays to target and kill cancer cells in a very specific location.
- Targeted Therapy: These are smarter drugs that are designed to zero in on specific weaknesses found in cancer cells, leaving healthy cells mostly alone.
- Immunotherapy: A groundbreaking approach that essentially "teaches" your own immune system how to recognize and attack cancer cells.
A diagnosis isn't just a label; it's the starting line for a strategic, personalized plan. When you know what each treatment does and why it's being recommended, you can become a confident and active partner in your own care.
This guide will dive deeper into each of these options, explaining how doctors choose them based on the cancer’s stage and its unique molecular signature. For a broader look, you can learn more about gastric cancer and its fundamentals. We're here to give you the essential knowledge you need to ask smart questions, understand the answers, and work hand-in-hand with your medical team.
The Building Blocks of Gastric Cancer Treatment
When we map out a plan to fight gastric cancer, we start with a set of powerful, well-established treatments. Think of these as the building blocks of your care. Each one has a specific job, but they work best when used together, creating a comprehensive strategy to attack the cancer from different angles.

This isn't a one-size-fits-all approach. The sequence and combination of treatments are carefully timed to give you the best possible outcome. Getting familiar with these core methods—surgery, chemotherapy, and radiation—will help you understand the logic behind your personal treatment plan.
Surgery: The First Line of Defense for Localized Cancer
For gastric cancer that hasn’t spread to other parts of the body, surgery is our primary tool. The goal is direct and effective: physically remove the tumor, a small border of healthy tissue around it, and nearby lymph nodes to make sure we get every last cancer cell.
The type of surgery depends entirely on the tumor's size and location in the stomach:
- Partial Gastrectomy: If the cancer is limited to a small area, the surgeon can remove just that part of the stomach. The remaining portion is then carefully reattached to the esophagus or small intestine.
- Total Gastrectomy: When the cancer is more widespread, the entire stomach needs to be removed. In this case, the surgeon connects the esophagus directly to the small intestine, creating a new pathway for food.
In early-stage disease, surgery offers the greatest hope for a cure. But it's a major operation and often just the first step in a broader treatment journey.
Chemotherapy: A Full-Body Approach
While surgery is a local fix, chemotherapy works on a systemic level. It involves powerful drugs that circulate throughout your bloodstream to find and destroy cancer cells, which are known for their rapid growth. You can think of it as a security patrol for your entire body, hunting down any cells that may have broken away from the original tumor.
Chemotherapy is incredibly versatile and can be used at different points in your treatment:
- Neoadjuvant Chemotherapy: Given before surgery. The goal is to shrink the tumor, which can make the operation safer and more effective.
- Adjuvant Chemotherapy: Given after surgery. This is done to wipe out any stray, microscopic cancer cells that might have been left behind, lowering the chance of the cancer coming back.
- Primary Treatment: For advanced or metastatic cancer, chemotherapy often becomes the main treatment to control the disease, ease symptoms, and maintain a good quality of life.
The specific drug combination and treatment schedule are chosen based on your unique cancer profile and overall health. To see how this approach compares to newer methods, take a look at our guide on targeted therapy versus chemotherapy.
Radiation Therapy: Pinpoint Precision
Radiation therapy, or radiotherapy, is another essential tool. It uses high-energy beams, similar to X-rays, to damage the DNA inside cancer cells, which either kills them or stops them from growing. It’s like a highly focused flashlight beam that can be aimed with incredible precision at the tumor, minimizing harm to the healthy tissues around it.
A powerful strategy we often use is combining radiation with chemotherapy, a technique called chemoradiation. The chemotherapy makes the cancer cells more vulnerable to the radiation, boosting its effectiveness.
The table below summarizes how these core treatments are typically used.
Standard Gastric Cancer Treatment Modalities
These foundational therapies are the bedrock of modern gastric cancer care.
Historically, the biggest leaps in survival have come from intelligently combining these pillars. Landmark studies have shown that adding chemotherapy both before and after surgery can raise 5-year survival rates from 23% to 36%. Even with these gains, treating locally advanced disease is still a major challenge, which is why a carefully planned, multi-faceted approach is absolutely critical.
Personalized Medicine and Emerging Therapies
The old guard of cancer treatment—surgery, chemotherapy, and radiation—are still workhorses in our field, but the future of treating gastric cancer is looking much more specific. We’re moving away from a one-size-fits-all approach and into an era of personalized medicine, where the treatments we choose are guided by the unique genetic blueprint of your cancer.
This shift is fundamentally changing how we fight the disease, especially for cancers that are advanced or have come back. It all boils down to a simple but powerful idea: no two stomach cancers are exactly alike. By figuring out what makes a particular tumor tick, we can select treatments that are not only more effective but often kinder to the rest of your body.
Targeted Therapy: The "Smart Bomb" Approach
Think of traditional chemotherapy as a carpet bomb—it hits all fast-growing cells, both cancerous and healthy. Targeted therapy, on the other hand, is more like a "smart bomb." It's engineered to find and attack specific molecular flags, or biomarkers, that are on cancer cells but mostly missing from your healthy cells.
How is this possible? Scientists have zeroed in on certain genes and proteins that act like gas pedals for gastric cancer growth. If your tumor has one of these specific markers, we can use a drug designed to hit the brakes.
One of the most important biomarkers we look for in gastric cancer is HER2 (human epidermal growth factor receptor 2).
- What it is: HER2 is a protein that can show up in excessive amounts on the surface of some cancer cells, sending them a constant, overwhelming signal to grow and divide.
- Who it affects: Roughly 10-20% of gastric cancers are what we call HER2-positive.
- How we treat it: Drugs like trastuzumab (Herceptin) are designed to block the HER2 protein, essentially cutting off the cancer's growth signal at the source.
This strategy depends on testing a sample of your tumor tissue to see if these targets exist. A positive result can open up a whole new set of powerful, personalized treatments that we might not have considered otherwise.
By homing in on the cancer's specific vulnerabilities, we can often get better results with fewer of the widespread side effects that come with traditional chemotherapy. It’s a strategic move, turning the cancer's own biology against itself.
Immunotherapy: Unleashing Your Body's Own Defenses
Another incredible leap forward is immunotherapy, which works on a completely different principle. Instead of using drugs to attack the cancer directly, immunotherapy helps your own immune system do the job it was designed to do.
Cancer cells are tricky. They often find ways to hide from the immune system, almost like they’re wearing a disguise to avoid being seen as a threat. Immunotherapy drugs, especially a type called immune checkpoint inhibitors, work by ripping that disguise off.
These drugs block proteins like PD-1 or PD-L1, which act as "brakes" on your immune system. By releasing those brakes, the drugs free up your T-cells—the soldiers of your immune system—to recognize and destroy the cancer cells. This has become an essential treatment option for many patients whose tumors have high levels of these checkpoint proteins.
These modern therapies have made a real difference in patient outcomes. For instance, adding trastuzumab to chemotherapy for HER2-positive advanced gastric cancer was a major milestone, boosting median overall survival from around 11 months to nearly 14 months. You can explore more about these evolving treatment landscapes and the ongoing clinical trials shaping the future of care. To dig deeper, you can learn more about the shift toward personalized medicine on Nature.com.
The Critical Role of Biomarker Testing
None of these advanced treatments would even be on the table without biomarker testing, which you might also hear called molecular or genetic testing. This is simply the process of analyzing a piece of your tumor to identify the specific genetic mutations, proteins, and other features that make your cancer unique.
This isn't an optional step anymore; it’s a cornerstone of creating a smart, effective treatment plan for advanced gastric cancer. It gives your oncologist the critical intelligence needed to know if you're a candidate for a targeted therapy or immunotherapy. Think of it as gathering intel on the enemy before you plan the attack. The more we know, the smarter we can fight.
How Your Treatment Plan Is Shaped by Cancer Stage
There’s no such thing as a one-size-fits-all treatment plan for gastric cancer. Every strategy is highly personalized, and the single most important factor guiding that strategy is the cancer’s stage.
Staging essentially creates a detailed map of the cancer, telling us exactly how far it has grown and whether it has spread. Just like a GPS gives you different routes depending on your final destination, your cancer's stage determines the most effective path forward. The gastric cancer treatment options for a small, localized tumor are worlds away from the plan for cancer that has traveled to other organs.
Early-Stage Gastric Cancer (Stage 0 and Stage I)
When we catch gastric cancer very early (Stage 0 or I), the tumor is typically still contained within the inner layers of the stomach wall. At this point, the goal is a cure—the complete removal of the cancer before it gets a chance to go anywhere else. The focus is squarely on local treatments that can eliminate the tumor with precision.
For the smallest, most superficial tumors (Stage 0), a surgeon may not even be needed. A minimally invasive procedure called an endoscopic resection allows a gastroenterologist to remove the cancerous tissue through a flexible tube passed down the throat.
For most Stage I cancers, however, surgery is the cornerstone of treatment.
- Surgery (Gastrectomy): A surgeon will perform a partial or total gastrectomy, removing the part of the stomach with the tumor and nearby lymph nodes to check for any spread. For many people with early-stage disease, surgery alone can be curative.
- Adjuvant Therapy: Think of this as an insurance policy. After surgery, your doctor might recommend chemotherapy or a combination of chemo and radiation (chemoradiation) to wipe out any microscopic cancer cells left behind and reduce the chances of the cancer returning.
Locally Advanced Gastric Cancer (Stage II and Stage III)
By Stage II or III, the cancer has dug deeper into the stomach wall and may have invaded nearby lymph nodes. The key here is that it has not yet reached distant organs. Because the cancer is more established, the treatment strategy has to be more complex. A single approach just isn't enough.
While the goal is still a cure, getting there requires a multi-pronged attack. Combination therapy—using chemotherapy or chemoradiation alongside surgery—is the standard of care.
This layered approach is critical. For instance, giving chemotherapy before surgery (neoadjuvant therapy) can shrink the tumor, making it easier for the surgeon to remove it completely. Giving it after surgery (adjuvant therapy) helps destroy any remaining cancer cells.
This strategic sequencing is designed to hit the cancer from every possible angle, maximizing the chances of a successful outcome. It's a vital step, because even after a successful surgery, up to 84% of patients with Stage II or III disease can see their cancer come back. This comprehensive approach is our best weapon against recurrence.
The infographic below shows how we can further refine treatment by looking at the tumor's specific biological markers.
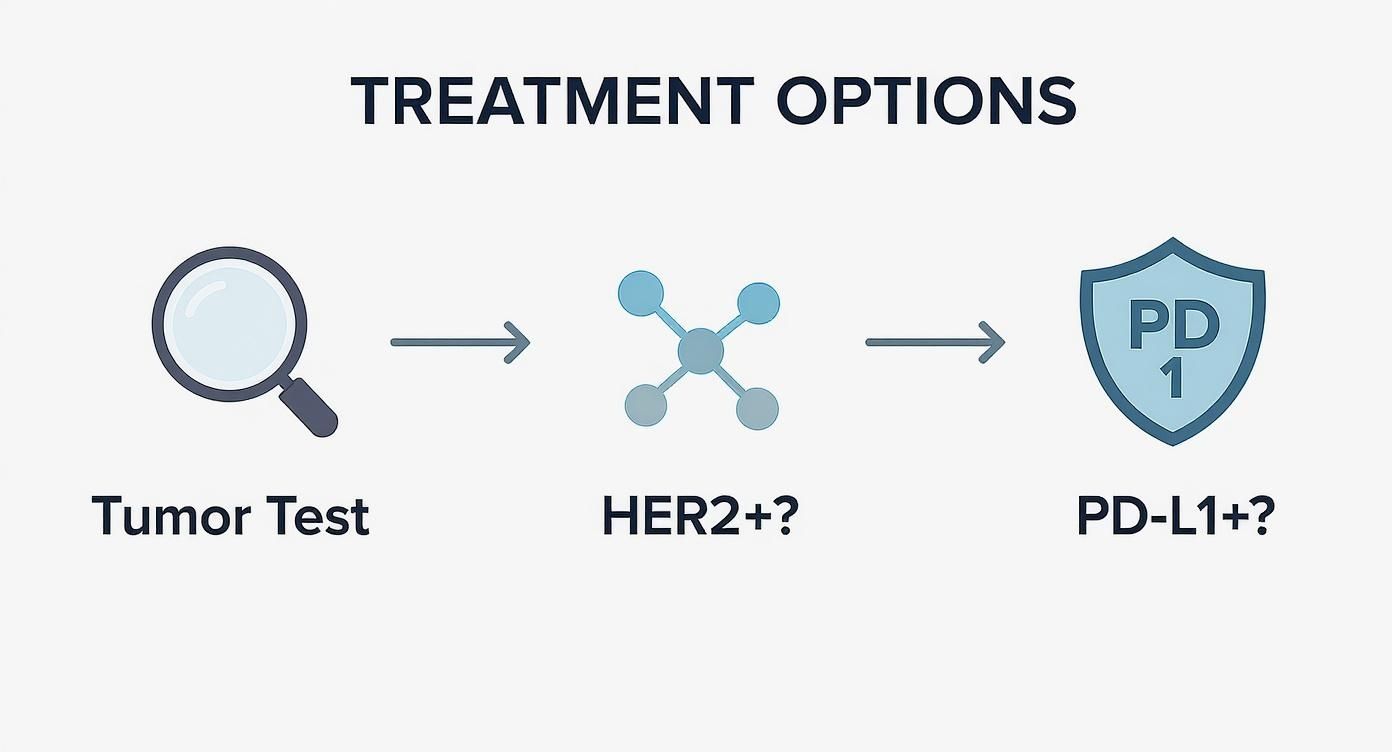
As you can see, it's not just about the stage. The molecular details of the tumor itself help us select the most powerful therapies available.
Metastatic Gastric Cancer (Stage IV)
If gastric cancer is diagnosed at Stage IV, it means the disease has metastasized—it has spread to distant parts of the body, such as the liver, lungs, or far-off lymph nodes. At this point, a cure is generally not possible with the treatments we have today. The entire focus of treatment shifts.
The goal moves from eliminating the cancer to controlling it. We aim to:
- Slow the cancer's growth and spread.
- Manage symptoms caused by the tumors.
- Improve and maintain your quality of life for as long as possible.
Surgery is rarely the main event for Stage IV cancer, though it might be used to relieve a blockage or control bleeding. Instead, the foundation of treatment becomes systemic therapies—drugs that travel through the bloodstream to fight cancer cells wherever they are in the body.
These options include:
- Chemotherapy: This is often the first-line treatment to get the disease under control.
- Targeted Therapy: If the cancer cells have specific molecular "flags" like HER2, we can use drugs designed to attack that specific target.
- Immunotherapy: This approach helps your own immune system recognize and fight the cancer. It's an option for tumors with certain biomarkers, like PD-L1.
Your oncology team will work with you to find the right balance between fighting the cancer aggressively and managing side effects, always keeping your well-being as the top priority.
Managing Treatment Side Effects and Quality of Life
Going through gastric cancer treatment is about more than just fighting the disease—it's about protecting your quality of life every step of the way. The best gastric cancer treatment options don't just target the cancer; they also support your strength and overall well-being. This requires a proactive plan for managing side effects right from the start.

It’s helpful to think of managing side effects as a core part of your treatment, not an afterthought. By getting ahead of these challenges, you can stay stronger, handle your treatments better, and keep more control over your daily life. It’s a true team effort between you, your family, and your entire healthcare team.
Navigating Nutrition After Surgery
After a partial or total gastrectomy, the way you eat will change significantly. Because the stomach's ability to hold food is either smaller or gone completely, you'll need new strategies to get the nutrition your body desperately needs for healing.
Your care team will reintroduce food very carefully, usually starting with clear liquids and slowly building from there. A temporary feeding tube might be used to make sure you’re getting enough calories and protein as your digestive system adjusts. This phase requires patience, but it’s a crucial part of recovery.
Once you’re ready for more solid foods, you’ll need to adjust your habits:
- Eat Smaller, More Frequent Meals: Forget three big meals a day. The new goal is five to six small, nutrient-packed mini-meals.
- Focus on Protein and Healthy Fats: These are vital for tissue repair and keeping your muscle mass up.
- Chew Thoroughly and Eat Slowly: Taking your time helps your body digest food more easily and prevents discomfort.
- Avoid High-Sugar Foods: Sugary foods can trigger "dumping syndrome," a common issue where food rushes into the small intestine too quickly. This can cause cramps, dizziness, and diarrhea.
Coping with Chemotherapy and Systemic Therapies
Chemotherapy, targeted therapy, and immunotherapy are powerful weapons, but they can affect your whole body. The most common hurdles patients face are nausea and fatigue. It’s absolutely critical to talk openly with your oncology nurse and doctor, because there are many excellent ways to manage these symptoms.
For nausea and vomiting, your team will prescribe anti-sickness medications that you should take before you feel sick. Staying ahead of it is the key. For more tips on eating during this time, our guide on the best foods for chemotherapy patients is a great resource.
Managing fatigue is a delicate balance between rest and activity. It sounds strange, but light exercise, like a short walk, can often do more to boost your energy than staying in bed all day.
Side effects from targeted therapies and immunotherapies often look different—think skin rashes, diarrhea, or symptoms related to inflammation. Always report new or worsening side effects to your team immediately. These issues need specific management plans, and prompt attention makes all the difference.
Your Essential Quality of Life Support Team
You don't have to face this alone. A whole team of specialists is ready to help you handle the physical and emotional side of treatment, working right alongside your oncologist to keep your well-being front and center.
- Registered Dietitian: An oncology dietitian is an invaluable partner. They can help you create a personalized eating plan to navigate post-surgery changes, maintain a healthy weight, and deal with issues like taste changes or a poor appetite.
- Physical and Occupational Therapists: These experts help you safely build back your strength, manage fatigue, and find ways to adapt to physical challenges so you can stay as independent as possible.
- Palliative Care Specialist: This is a widely misunderstood specialty. Palliative care isn't just for the end of life; it’s for anyone with a serious illness. The goal is to provide relief from symptoms and stress, and it can be started right at diagnosis.
- Counselors and Social Workers: A cancer diagnosis is stressful for the whole family. These professionals offer crucial emotional support and can connect you with practical resources like support groups and financial aid programs.
Key Questions to Ask Your Oncology Team
That first appointment with the oncologist can feel like a blur. There's so much information coming at you, and it's easy to feel overwhelmed. But being prepared with a few key questions can change everything. It helps you take an active role in your own care, making you a partner with your doctor, not just a patient.
Think of this as your starting point for a conversation. These questions are designed to help you and your oncology team get on the same page, ensuring you have the information you need to make decisions you feel good about.
First, Get a Handle on Your Diagnosis
Before you can even start thinking about treatment, you need to understand exactly what you’re dealing with. The specifics of your cancer are the roadmap for your entire treatment journey. Don't be shy about asking your doctor to break it down for you until it makes sense.
Here's what to ask to get started:
- What is the exact stage of my cancer? What does that mean for my outlook?
- Has it spread anywhere, like to the lymph nodes or other parts of my body?
- Have you tested the tumor for specific markers, like HER2 or PD-L1?
- How do those test results change our treatment options?
- Could you walk me through my pathology report in plain English?
These aren't just technical details; they are the most important clues that will guide your doctor's recommendations.
Weighing Your Treatment Options
With a clear diagnosis in hand, the conversation will turn to the plan of attack. Your doctor will suggest a course of treatment, but you need to understand why they're recommending it and what other options might be on the table. This is your time to explore every path.
"The goal of any good treatment plan isn't just to target the cancer. It's to do it in a way that fits your life and what's most important to you."
Consider asking these questions to understand the big picture:
- What are we trying to achieve with this treatment? Is the goal a cure, to control the cancer, or to manage my symptoms?
- What are the biggest benefits of this plan, and what are the most serious risks?
- Are there any other standard treatments we could consider?
- Why do you believe this specific approach is the right one for me, right now?
- How will we know if the treatment is actually working?
Life During Treatment: Side Effects and Support
A treatment plan on paper is one thing, but actually living through it is another. Knowing what to expect can help you prepare for the road ahead—physically and emotionally. This part of the discussion is all about being realistic and lining up the support you'll need.
Be sure to cover these practical points:
- What are the most common side effects I should watch out for, both now and in the long run?
- How is this going to affect my daily life—my job, my appetite, my energy levels?
- Who do I call if I have a problem or a scary side effect, especially if it's after hours or on a weekend?
- Are there other experts who should be part of my team, like a nutritionist or a palliative care specialist?
Looking Ahead: Clinical Trials and Next Steps
Finally, it’s always a good idea to ask what might be next. Cancer research is moving incredibly fast, and clinical trials often provide access to new therapies before they become widely available. This is particularly important if your cancer is advanced or isn't responding to standard treatments.
Don't leave without asking:
- Are there any clinical trials that could be a good match for my type of cancer?
- What are the pros and cons of joining a clinical trial?
- If this first treatment stops working, what would we try next?
A simple tip: bring a notebook and a friend or family member to your appointments. Having a second set of ears and someone to take notes can make a huge difference. Your oncology team is your greatest ally—use these questions to build a strong partnership grounded in open communication.
Common Questions About Gastric Cancer Treatment
When you're facing a gastric cancer diagnosis, a lot of questions come up. It's completely normal. Here, we'll walk through some of the things patients and families often ask, providing clear answers to help you feel more informed and prepared.
What’s the Difference Between Neoadjuvant and Adjuvant Therapy?
You'll hear these terms a lot, and they simply refer to the timing of treatments like chemotherapy in relation to your surgery. It’s a bit like renovating a house.
Neoadjuvant therapy is the work you do before the main event. It's given before surgery to shrink the tumor. A smaller tumor is often easier for the surgeon to remove completely, which can lead to a better outcome.
Adjuvant therapy is the work you do after the main event. This treatment comes after surgery and acts like a final deep clean, aiming to wipe out any stray cancer cells that might be lingering. The goal here is to reduce the risk of the cancer coming back.
Deciding whether to use one, both, or neither really depends on the cancer's stage. For many locally advanced stomach cancers, using a combination of neoadjuvant and adjuvant therapy around surgery is a powerful and standard approach.
Will I Need a Feeding Tube After My Surgery?
It's very common to need a temporary feeding tube after a gastrectomy, and it's a critical part of your recovery. Think of it as a nutritional support system that gives your body the fuel it needs to heal while your digestive system gets a much-needed rest.
How long you'll need it is tied to the type of surgery you have:
- Partial Gastrectomy: Since a portion of your stomach is still there, you might be able to start eating by mouth again a bit sooner.
- Total Gastrectomy: Recovery from this surgery is more involved, so a feeding tube is often needed for a longer period to ensure you stay strong.
Your surgical team and a nutritionist will work together to create a plan just for you. They'll guide you step-by-step as you safely and gradually return to eating on your own.
How Do I Know if a Clinical Trial Is Right for Me?
Clinical trials can be a fantastic pathway to new treatments, but they aren't for everyone. Whether you're a candidate depends on a whole host of factors—your cancer's specific stage, its molecular profile, treatments you've had in the past, and your overall health.
Your oncologist is the best person to start this conversation with. They’ll know about trials that could be a good match and can help figure out if you're eligible. It’s also a great idea to do your own research on sites like ClinicalTrials.gov and bring anything you find to your doctor to discuss.
At Hirschfeld Oncology, we are committed to helping our patients explore every possible option, from standard-of-care to emerging therapies and clinical trials. If you're looking for a more personalized, lower-toxicity strategy, we invite you to learn more on our blog at https://honcology.com/blog.





.png)


.png)
.png)




