Navigating a cancer diagnosis means making some complex choices, and a big one is understanding your treatment options. At the heart of it, the difference between immunotherapy and chemotherapy comes down to how they fight cancer. Chemotherapy is a direct assault, using powerful drugs to kill fast-growing cancer cells. Immunotherapy, on the other hand, is more of a strategic move—it helps your own immune system do the job it was designed to do.
Understanding Your Cancer Treatment Options
When you or a loved one is diagnosed with an advanced cancer, whether it's pancreatic, colorectal, or breast cancer, the road ahead can feel uncertain. You'll likely hear two terms a lot: chemotherapy and immunotherapy. While both are pillars of modern cancer care, they work in fundamentally different ways. You could almost think of it as a controlled demolition versus training an elite special forces team.
Chemotherapy has been a go-to treatment for decades. It works systemically, meaning the drugs travel throughout your entire bloodstream to kill cells that are dividing rapidly. This is great for targeting fast-growing tumors, but it’s not very selective. Chemo can't always tell the difference between a cancer cell and a healthy, rapidly dividing cell, like those in your hair follicles, bone marrow, or digestive tract. This collateral damage is what causes many of its well-known side effects.
Immunotherapy is a newer, more targeted approach. It doesn't attack cancer cells on its own. Instead, it acts as a trainer for your immune system, teaching it to recognize and eliminate cancer. Cancer cells are notoriously good at hiding from the body's natural defenses, and immunotherapy essentially pulls off their camouflage so your immune system can see them and go on the attack.

Making an Informed Decision
Grasping these core differences is the first step in having a productive conversation with your oncology team. The decision isn't just about choosing one over the other; often, the best strategy involves using them in sequence or even together. It all hinges on the specific type of cancer you have, its unique genetic markers, and your overall health.
Here at Hirschfeld Oncology, our entire philosophy is built on this kind of personalized care. We dive deep into your unique biology to match the treatment not just to the cancer, but to your personal quality-of-life goals.
To make things a bit clearer, here’s a quick breakdown of the key distinctions between these two powerful treatments.
At-a-Glance Comparison: Immunotherapy vs. Chemotherapy
This table gives you a starting point, but the real conversation happens between you and your oncologist. The best choice is always the one that’s tailored specifically for you.
How Each Treatment Fights Cancer
To really get to the heart of the difference between immunotherapy and chemotherapy, you have to understand their fundamental strategies. While both are powerful weapons in our arsenal against cancer, they fight on completely different fronts. One wages a direct chemical assault on cancer cells, while the other trains your body’s own defense forces to carry out a precise, targeted mission.

Chemotherapy: A Direct Cellular Attack
Chemotherapy works by flooding the body with cytotoxic (cell-killing) drugs that get in the way of cell division. By their very nature, cancer cells are defined by runaway growth and division, so this approach is designed to stop that process dead in its tracks. I often explain it to my patients as being like a broad-spectrum antibiotic—it's built to eliminate anything that multiplies quickly.
This is a proven, effective way to shrink tumors. But this broad, sweeping attack is also why chemotherapy’s side effects are so well-known. It simply can’t tell the difference between a rapidly dividing cancer cell and other healthy cells in your body that also happen to divide quickly.
This collateral damage tends to show up in a few key areas:
- Hair Follicles: These cells divide constantly, which is why hair loss is a common side effect for about 65% of patients.
- Bone Marrow: This is your body’s factory for new blood cells. Chemo can slow production, leading to fatigue from low red blood cells and a higher risk of infection from low white blood cells.
- Digestive Tract Lining: The cells lining your mouth and intestines turn over rapidly, which can cause mouth sores, nausea, and diarrhea.
The core principle of chemotherapy is to disrupt the cell cycle of any rapidly dividing cell. Its strength—widespread action—is also its primary source of side effects, as it doesn't differentiate between cancerous and healthy tissue.
Different chemo drugs accomplish this in different ways. Some work by directly damaging the DNA inside the cell’s nucleus so it can’t make copies of itself. Others interfere with the chemical signals that tell a cell it's time to divide. But no matter the specific drug, the end goal is the same: halt uncontrolled growth head-on.
Immunotherapy: Unmasking the Enemy Within
Immunotherapy takes a completely different path—a more indirect, strategic one. It doesn’t actually kill cancer cells on its own. Instead, it re-educates and empowers your own immune system, specifically your T-cells, to finally recognize and destroy cancer cells that have been hiding in plain sight.
Cancer is incredibly cunning. It figures out ways to fly under the immune system's radar, much like a fugitive using a disguise to blend into a crowd. One of its most effective tricks is to exploit the natural "brakes" on the immune system, known as checkpoints.
These checkpoints, like PD-1 on T-cells and its partner PD-L1 on other cells, are there for a good reason: they keep the immune system from going haywire and attacking healthy tissue. They’re a safety mechanism. Cancer cells hijack this system by plastering their surface with PD-L1, essentially hitting the brakes on any approaching T-cell and telling it, "I'm one of you, move along." For a deeper dive, you can explore our detailed guide on how immunotherapy works for cancer.
Immunotherapy drugs, especially a class we call checkpoint inhibitors, work by cutting off that deceptive signal. They act as a shield, physically blocking the cancer cell’s PD-L1 from connecting with the T-cell’s PD-1.
With this brake released, the T-cell is free to do its job. It can now see the cancer cell for the threat it is and launch a full-scale, targeted attack. It's not about poisoning the cancer cell; it's about ripping off its invisibility cloak so your body's own expert soldiers can take over. This targeted approach is a key reason why immunotherapy’s side effect profile is so different from chemotherapy’s—the goal is to leave healthy cells out of the fight.
Comparing Side Effects and Quality of Life
When patients and their families weigh treatment options, one of the first and most important questions is always, "How is this going to make me feel?" It's a critical piece of the puzzle. Both chemotherapy and immunotherapy are powerful treatments, but they work in fundamentally different ways, which leads to very different experiences and side effect profiles.
Chemotherapy's side effects are what most people picture when they think of cancer treatment. Because chemo is designed to attack any rapidly dividing cell, it can't tell the difference between a tumor cell and a healthy cell in your hair, stomach lining, or bone marrow. The side effects are a direct consequence of that action.
Immunotherapy, on the other hand, works by taking the brakes off your own immune system. So, its side effects—what we call immune-related adverse events (irAEs)—happen when that newly revved-up immune system accidentally targets healthy tissues.

Common Chemotherapy Side Effects
The side effects from chemotherapy are generally more predictable and tend to happen on a known schedule during your treatment cycles. While we have excellent ways to manage them, they can still take a toll on your quality of life.
Some of the most common effects include:
- Fatigue: This isn't just feeling tired; it's a deep exhaustion that rest doesn't always fix.
- Nausea and Vomiting: Modern anti-nausea drugs have made a world of difference, but this is still a primary concern we work hard to prevent.
- Hair Loss: Affecting about 65% of patients, this is a direct result of the treatment targeting fast-growing hair follicle cells.
- Increased Risk of Infection: Chemo can lower your white blood cell count, making your body more vulnerable to germs.
Chemotherapy has been a cornerstone of cancer care since the 1940s, but we've always been aware of the significant toxicity that can come with it. To give you an idea, in a major lung cancer trial, a staggering 90% of patients on standard platinum-based chemotherapy had treatment-related side effects, with over half experiencing severe issues.
Understanding Immunotherapy Side Effects
Immunotherapy side effects are a completely different animal. Since the treatment is "unleashing" the immune system, the side effects are inflammatory in nature and can pop up in almost any organ. They are often less frequent than chemo's side effects, but they can be unpredictable and sometimes more complex.
These immune-related adverse events can include:
- Skin Reactions: Rashes and itching are very common early signs that the immune system is activated.
- Colitis: This is inflammation in the colon, which can cause diarrhea.
- Pneumonitis: Inflammation in the lungs, which might present as a cough or shortness of breath.
- Endocrinopathies: The immune system can sometimes affect hormone-producing glands like the thyroid.
Interestingly, while immunotherapy side effects can be serious, their appearance is often a sign that the treatment is successfully waking up the immune system. The absolute key is catching them early and managing them proactively, often with medications like steroids that can calm the overactive immune response without stopping the attack on the cancer.
A Proactive Approach to Management
No matter which path we take, our goal is the same: control the cancer while protecting your quality of life as much as possible. This isn't something you go through alone; it's a partnership between you and your oncology team, built on clear communication and careful monitoring.
Here at Hirschfeld Oncology, we make this a priority. For our patients on chemotherapy, that means getting ahead of nausea with premedication and keeping a close eye on blood counts. For our immunotherapy patients, it means educating you on exactly what to watch for and being available to address any new symptom right away.
Navigating treatment is a team effort. We provide extensive support and resources, and you can find more of our practical advice in our guide to managing the side effects of cancer treatment. By working together, we can stay ahead of these effects and help you feel your best throughout your treatment journey.
How Do We Measure Success? A Look at Treatment Effectiveness
When we talk about whether immunotherapy or chemotherapy is "better," it's not a straightforward comparison. There's no single winner. The right choice depends entirely on the type of cancer, its specific genetic makeup, and the individual patient sitting in front of me. What works wonders for one person might do very little for another, which is why we've moved so far beyond a one-size-fits-all approach.
Chemotherapy has long been a cornerstone of cancer treatment, and for good reason. It's often the most reliable first-line defense, especially for cancers that grow aggressively. Its main strength is its ability to get a quick response—shrinking tumors and easing symptoms relatively fast. For many advanced cancers, like certain pancreatic or ovarian cancers, chemotherapy is still the most effective tool we have to start with.
Immunotherapy, on the other hand, is a different ballgame. It doesn't work for everyone, but when it does, the results can be life-changing and incredibly long-lasting. This is what we oncologists call a "durable response." We're not just shrinking the tumor for now; we're teaching the body's own immune system to keep the cancer in check for months, or even years, down the road.
The real difference in effectiveness comes down to the pattern of response. Chemotherapy is like a broad attack designed to get an immediate reduction in tumor size. Immunotherapy is more of a strategic, targeted mission to create a lasting "immune memory" that provides long-term surveillance against the cancer.
It's All in the Biology
The decision between these two powerful treatments often hinges on biomarkers—specific molecular flags found on or inside the tumor cells. These markers are like signposts that tell us which therapy is more likely to work.
A great example is in certain colorectal cancers that have a feature called microsatellite instability-high (MSI-H). This essentially means the cancer’s DNA repair system is broken, causing tons of mutations. These mutations make the cancer cells look very strange to the immune system, almost like a foreign invader. For these patients, immunotherapy can be remarkably effective, often outperforming chemotherapy by a long shot.
On the flip side, many pancreatic cancers are what we call "cold" tumors. They don't have many immune cells hanging around and lack the biomarkers that immunotherapy drugs look for. In these situations, chemotherapy is usually the more effective path forward to control the disease.
A Look at Outcomes in Specific Cents
Let's break down how these treatments stack up for a few common advanced cancers we see here at Hirschfeld Oncology. This really highlights how nuanced the decision-making process is.
- Breast Cancer: For triple-negative breast cancer, which is notoriously difficult to treat, combining chemotherapy with immunotherapy has become a game-changer for patients whose tumors express a biomarker called PD-L1.
- Gastric & Esophageal Cancers: We've seen a similar story here. Adding immunotherapy to a standard chemotherapy regimen for patients with PD-L1 positive tumors is now the standard of care, leading to significantly better survival rates.
- Cholangiocarcinoma (Bile Duct Cancer): This has always been a tough one, relying heavily on chemotherapy. But recent breakthroughs show that adding immunotherapy can extend survival for some patients, which is a major step forward for this rare cancer.
The Power of a Durable Response
That idea of a "durable response" is probably the biggest advantage immunotherapy brings to the table. Chemotherapy can be great at shrinking tumors, but over time, the cancer can become resistant and start growing again. Because immunotherapy creates an immune memory, it can offer ongoing protection.
We’ve seen this most dramatically in advanced non-small cell lung cancer (NSCLC). Immunotherapy drugs like pembrolizumab have completely rewritten the survival playbook. In key clinical trials for patients with high levels of the PD-L1 biomarker, pembrolizumab nearly doubled the median overall survival to 26.3 months compared to just 14.2 months with chemotherapy alone. That’s a massive shift. Historically, the 5-year survival rate for this stage of lung cancer was a dismal 5.5%. For the right patients, modern immunotherapy can push that figure up to around 25%. You can read more about these long-term survival findings here.
This data proves a critical point: even if a smaller group of patients responds to immunotherapy, those who do can achieve a level of long-term control that was simply unimaginable a decade ago. Here at Hirschfeld Oncology, our job is to perform a deep biological analysis of your cancer to figure out if you're one of the patients who can benefit from this powerful and lasting response.
How to Decide on Your Treatment Path
Choosing between immunotherapy and chemotherapy—or figuring out how to use them together—is one of the most important conversations you'll have with your oncologist. There’s no single "best" answer. The right path is the one that fits your specific cancer, your body, and what you want out of treatment.
This decision is always a partnership. At Hirschfeld Oncology, Dr. Hirschfeld works closely with every patient right here in our Brooklyn office to weigh all the factors. We want to make sure your treatment plan is not only medically sound but also aligns with your priorities for quality of life.
The Role of Biomarkers in Your Treatment Plan
Modern oncology is all about the data, and the most important data comes from the tumor itself. We use sophisticated tests to look for biomarkers—think of them as molecular signposts on your cancer cells that point us toward the most effective treatment.
These aren't just vague clues; they're specific features that predict how a cancer will respond to a certain therapy.
Two of the most critical biomarkers we test for are:
- PD-L1 Expression: This is a protein that cancer cells use to hide from the immune system. If your tumor has high levels of PD-L1, it’s often a strong signal that it will respond well to immunotherapy drugs designed to block that "hiding" mechanism.
- Microsatellite Instability (MSI) Status: Cancers with high microsatellite instability (MSI-High) have a broken DNA repair system, which leads to a ton of mutations. All those mutations make the cancer cells look very strange to the immune system, essentially painting a giant target on their backs for immunotherapy.
The presence of a key biomarker like high PD-L1 can completely change the treatment conversation. A patient with MSI-High colorectal cancer, for instance, might be an ideal candidate to start with immunotherapy, which can offer a more durable and targeted response than traditional chemotherapy for that specific subtype.
This decision tree gives you a great visual of how a single biomarker, like MSI status, can create two completely different treatment pathways right from the get-go.
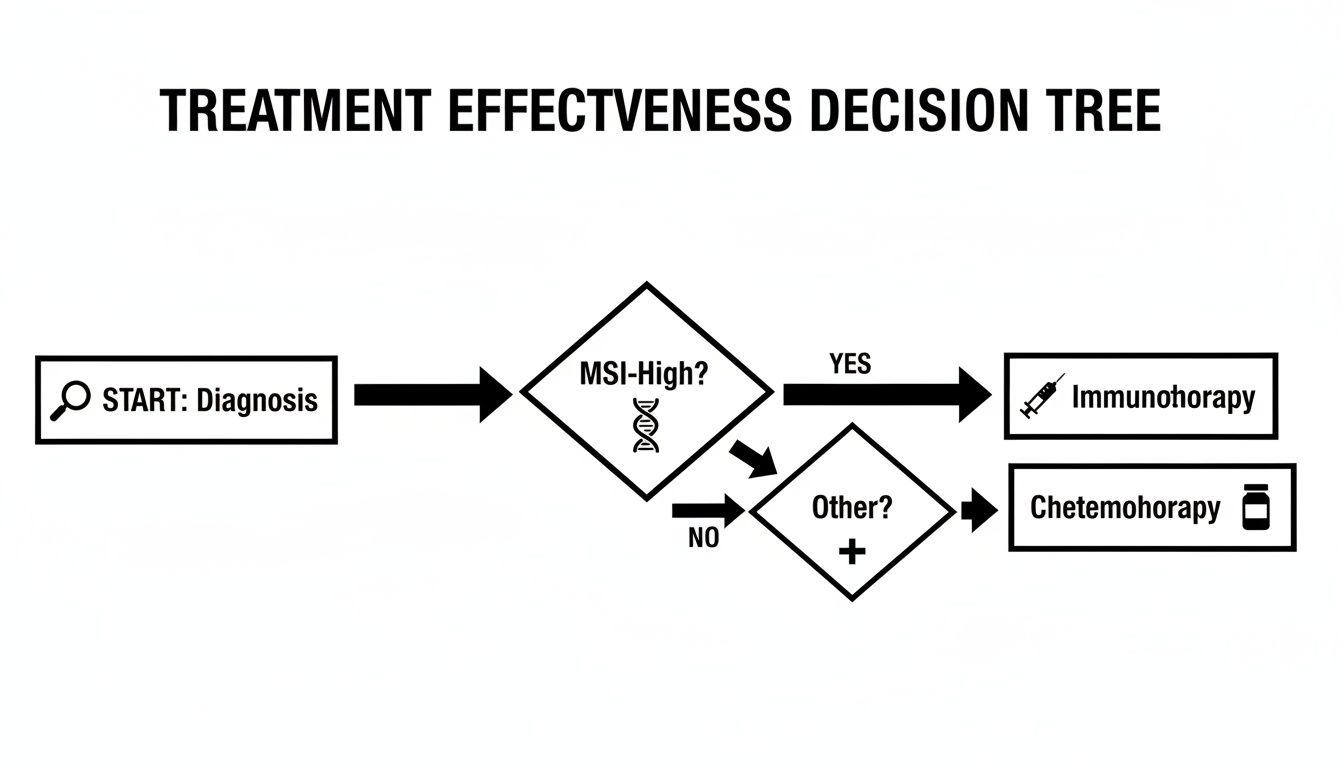
It really shows the power of personalized medicine in action: your tumor’s unique biology directly tells us whether immunotherapy or chemotherapy makes more sense as the first step.
Considering Your Health and Treatment Goals
Beyond the tumor's biology, your overall health and personal preferences are just as important. We take a careful look at your performance status—a measure of your physical fitness and ability to handle treatment—as well as any other health conditions you might have.
For example, a patient struggling with symptoms from a large tumor might benefit from the fast-acting, tumor-shrinking power of chemotherapy first, even if their cancer has biomarkers for immunotherapy. The immediate goal there is to bring relief and get things under control. On the other hand, if a patient has a pre-existing autoimmune condition, we have to be much more cautious with immunotherapy, as it could potentially flare up their condition.
Ultimately, your goals are what guide the plan. Do you need to prioritize keeping your energy up for work or family? Are you willing to manage more complex side effects for the chance of a longer-lasting remission? These are the real-world questions we talk through to build a plan that truly fits your life.
Combining and Sequencing Therapies for Better Outcomes
The decision isn't always an "either/or" choice. In many cases, the most effective strategy is to use both treatments together or in a specific order.
- Combination Therapy: For many advanced cancers, like certain types of lung or gastric cancer, we now combine chemotherapy and immunotherapy right from the start. Chemotherapy kills cancer cells in a way that releases tumor fragments (antigens), which can act like a "wake-up call" for the immune system, making the immunotherapy work even better.
- Treatment Sequencing: In other scenarios, we might begin with chemotherapy to shrink the tumor and then switch to immunotherapy as a second-line or maintenance therapy. This is a common approach if the first treatment stops working or if we want to lock in the progress made with chemo.
Understanding your cancer's genetic blueprint is the key to making these strategic decisions. By analyzing the tumor’s mutations, we can design a much more precise and effective plan. To get a better sense of how this works, you can explore the applications of genomic profiling in cancer treatment decisions in our detailed guide. This in-depth approach is how we at Hirschfeld Oncology offer truly personalized care, moving beyond one-size-fits-all protocols to find the right sequence for you.
Common Questions We Hear About Immunotherapy and Chemotherapy
When you're trying to understand your cancer care, a lot of practical questions come up. As you weigh the differences between immunotherapy and chemotherapy, you’re likely wondering about the nitty-gritty details—things like scheduling, long-term effects, and the reasoning behind a particular treatment plan. Here are some straightforward answers to the questions we hear most often from patients and their families at our Brooklyn oncology center.
Can I Receive Immunotherapy After Chemotherapy?
Absolutely. This is a very common sequence, and for many patients, it can be highly effective. When we use immunotherapy after a patient has already gone through chemotherapy, we refer to it as a second-line therapy. This is actually the standard of care for many advanced cancers, including certain lung, bladder, and head and neck cancers, especially if the initial chemotherapy has stopped working.
Of course, the decision to start immunotherapy depends on a few key things. We’ll look at the specific type of cancer you have, its unique biology, and whether it has crucial biomarkers (like PD-L1). Just as important is your overall health and strength after finishing your chemo regimen. For many people, making this switch offers a completely new way to fight the cancer by activating the immune system when chemotherapy's direct attack has run its course.
Why Would My Doctor Combine Both Treatments?
Pairing chemotherapy with immunotherapy right from the beginning can be an incredibly powerful strategy because it plays to the strengths of both. This isn't just about fighting the cancer from two different directions; it's about creating a special kind of synergy where each treatment makes the other one work better.
Here’s a simple breakdown of how they work together:
- Chemotherapy Does the Groundwork: As chemotherapy kills cancer cells, they break apart and release proteins called antigens.
- The Cancer Becomes Visible: This flood of antigens essentially acts like a flare, lighting up the tumor and making it much more obvious to your immune system.
- Immunotherapy Unleashes the Attack: With the cancer now exposed, immunotherapy steps in to take the brakes off your T-cells, allowing them to find and destroy the cancer cells much more effectively.
This one-two punch has become the go-to approach for several advanced cancers, like many non-small cell lung cancers and gastric cancers. By using them in tandem, we often see better response rates and can keep the disease under control for longer than we could with either treatment on its own.
Think of it this way: Chemotherapy can effectively 'unmask' a tumor, allowing immunotherapy to guide the immune system to a clearer, more recognizable target.
How Long Does a Treatment Session Take?
The amount of time you'll spend in the infusion chair can differ quite a bit, and it's one of the practical differences between the two therapies that will directly affect your day-to-day life.
Chemotherapy infusions can last anywhere from 30 minutes to several hours. The exact duration depends on the specific drug combination, whether you need pre-medications to manage side effects, and if you require extra hydration. Some of the more complex chemo regimens might mean a longer day at the clinic.
On the other hand, immunotherapy infusions are usually much shorter and more predictable. Most of these drugs are given over 30 to 90 minutes. The scheduling is different, too. Infusions are typically spaced out every two, three, four, or even six weeks, which often feels more manageable than some weekly chemo cycles. Here at Hirschfeld Oncology, we make sure you have a crystal-clear understanding of your treatment schedule well in advance.
Are There Long-Term Side Effects I Should Know About?
Yes, both treatments can have side effects that linger long after you’ve finished, but they tend to be very different in nature. Getting a handle on these potential long-term impacts is key to making informed choices and managing your health for the long haul.
Chemotherapy's lasting effects are usually a result of its impact on healthy, fast-dividing cells. Some common ones include:
- Peripheral Neuropathy: Nerve damage that causes ongoing numbness, tingling, or pain, often in the hands and feet.
- Cognitive Changes: Sometimes called "chemo brain," this can show up as trouble with memory or staying focused.
- Fertility Issues: The treatment can sometimes damage reproductive organs, affecting the ability to have children.
Immunotherapy's long-term side effects come from a permanently revved-up immune system. While most immune-related issues can be managed and resolved, a few can become chronic conditions. These might include:
- Endocrinopathies: If the immune system attacks a gland (like the thyroid or pituitary), it can cause a permanent hormone deficiency that requires lifelong replacement therapy.
- Type 1 Diabetes: In rare instances, an immune attack on the pancreas can trigger this condition.
No matter the treatment, proactive monitoring is our best tool for minimizing the long-term impact of therapy and protecting your quality of life for years to come.
At Hirschfeld Oncology, we believe that taking the time to answer your questions is a vital part of your care. Dr. Hirschfeld and our entire team are here to provide the clarity and support you need to feel confident in your treatment path. To learn more or to schedule a consultation at our Brooklyn center, feel free to explore our blog for further insights and patient stories.





.png)


.png)
.png)




