At its core, immunotherapy is a treatment that helps your own immune system do its job better—recognizing and fighting cancer. Think of it as taking the handcuffs off your body's natural defenses, allowing them to see and attack cancer cells that were previously hiding in plain sight.
This is a fundamentally different way of thinking about cancer treatment. Instead of bringing in an outside force to kill cancer cells, we’re empowering your own biology to win the fight.
Unlocking Your Body's Power to Fight Cancer

Your immune system is a sophisticated team of defenders, constantly on patrol for threats like viruses and bacteria. When it finds one, it quickly learns to identify and eliminate it. The problem is that cancer cells are tricky. Because they start as normal, healthy cells, they have an uncanny ability to masquerade as "self" and evade this natural security detail.
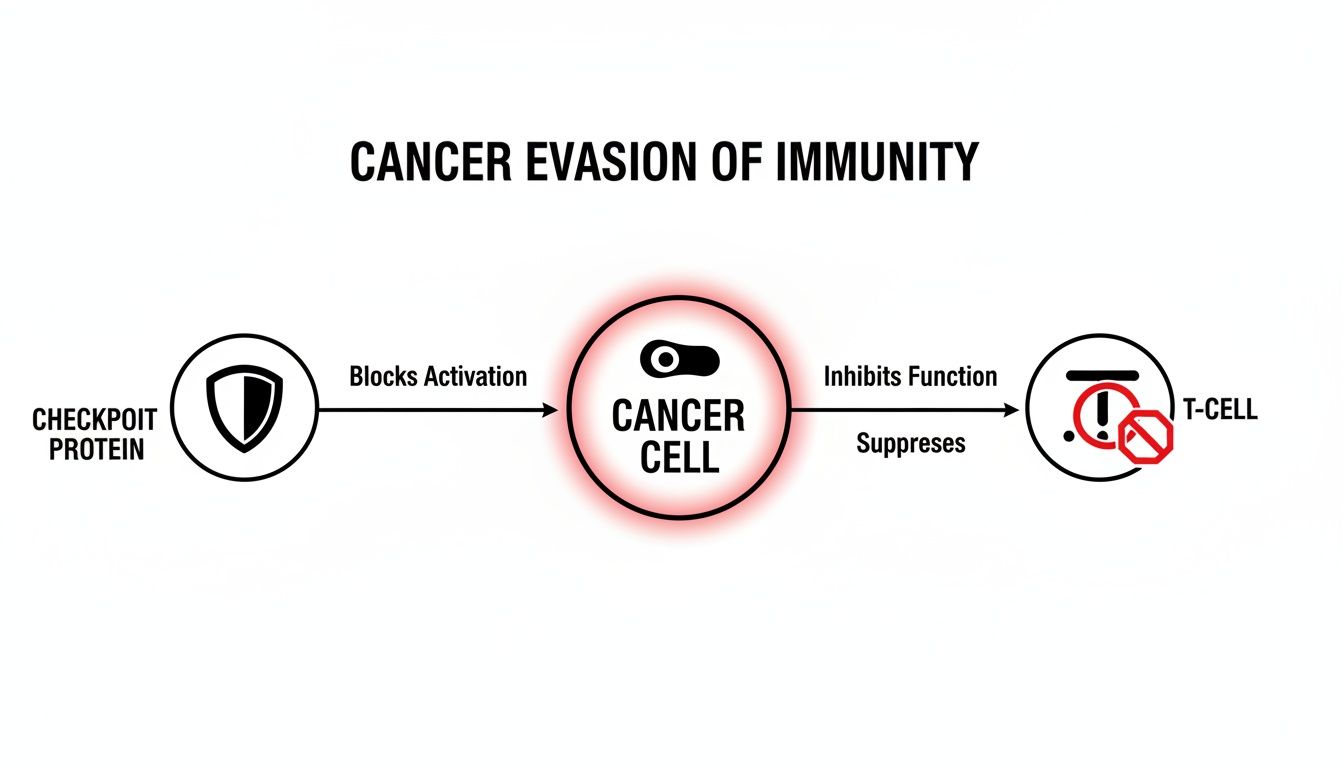
Cancer cells develop clever tactics to fool the immune system into ignoring them. One of their most effective strategies is to manipulate the natural "off switches," or checkpoints, that keep immune cells in check. These checkpoints are there for a good reason—to stop your immune system from going haywire and attacking your own healthy tissues.
But cancer cells hijack this safety feature. For example, many tumors display a protein called PD-L1. When this protein binds to the PD-1 receptor on your T-cells (your immune system's elite soldiers), it slams on the brakes, telling the T-cell, "Move along, nothing to see here." This deception allows the tumor to grow completely unchallenged.
A New Strategy in Cancer Treatment
This is where immunotherapy comes in. Instead of attacking cancer cells directly with chemicals, it outsmarts their defenses. Drugs like checkpoint inhibitors work by blocking that deceptive signal between the tumor cell and the T-cell. They essentially put a shield over the T-cell's "off switch," preventing the cancer cell from pressing it.
By "releasing the brakes," these treatments free your immune system to do what it was designed to do. The core principles are elegant and powerful:
- Boost Recognition: It helps the immune system finally see the cancer cells for what they are—a dangerous threat.
- Activate the Attack: It unleashes your T-cells to hunt down and destroy tumors throughout the body.
- Create Lasting Memory: In many cases, the immune system can develop a long-term "memory" of the cancer, helping it guard against a recurrence down the road.
Immunotherapy doesn't introduce a foreign substance to kill cancer; it enhances your body's innate ability to do the job. It’s a treatment that works with your body, not just on it.
To help clarify this difference, let's compare immunotherapy to more traditional cancer treatments.
Immunotherapy Compared to Traditional Cancer Treatments
This table offers a quick comparison, showing the fundamental differences in how these major treatment types work.
This fundamental shift from directly targeting the tumor to empowering the immune system is what makes immunotherapy so promising. It explains why its effects, timelines, and even side effects are so different from what many people expect from cancer therapy. By working with the body’s own defenses, we've opened up entirely new possibilities for patients, even those with advanced cancers that were once considered untreatable.
Why Your Immune System Sometimes Misses Cancer
To really grasp how immunotherapy works, we first need to look at the problem it's designed to solve. Your immune system is a brilliant, highly effective security force, constantly on patrol for threats inside your body. So, why does this elite team sometimes fail to take out cancer cells?
The answer is surprisingly simple: cancer is a master of disguise.
Unlike a virus or bacteria, which the immune system immediately flags as a foreign invader, cancer starts with your own cells. Because of this, cancer cells don't initially trip any alarms. They look and act a lot like the healthy cells they grew from, which gives them a crucial head start to multiply before anyone notices. It's a bit like a spy who blends in perfectly, making it nearly impossible for security to spot them in a crowd.
As tumors grow, they get even better at hiding.
Putting on an Invisibility Cloak
One of cancer's most cunning tricks is to turn the immune system's own safety features against it. Your immune system is equipped with natural "brakes" known as checkpoints. These are absolutely essential. They stop powerful immune cells, like T-cells, from going rogue and attacking your own healthy tissue. Think of it as the body's built-in "friend or foe" recognition system.
Cancer cells figure out how to slam on these brakes themselves. Many tumors cover their surface with a protein called PD-L1. When an immune T-cell shows up to do its job, the tumor's PD-L1 connects with a receptor on the T-cell called PD-1. This is like hitting an off-switch. The connection sends a false "all clear" signal, tricking the T-cell into thinking the cancer cell is friendly and should be left alone.
By hijacking these natural checkpoints, cancer cells essentially wrap themselves in an invisibility cloak. They can grow and spread without a fight because they’ve convinced the body's security guards that there is no threat.
Other Evasion Tactics
Manipulating checkpoints is just one of the ways cancer stays hidden. Tumors have a whole bag of tricks to avoid being destroyed.
- Weakening the Signals: Cancer cells can remove the very markers (called antigens) on their surface that T-cells need to recognize them. It’s like a burglar wiping their fingerprints from a crime scene.
- Creating a Hostile Environment: Some tumors release substances that create a "force field" around them, suppressing any immune cells that get too close and making the area hostile to an attack.
- Rapid Mutation: Cancer cells are genetically unstable, meaning they change and mutate fast. Even if the immune system starts to recognize one version of a cancer cell, a new, slightly different one can pop up that it no longer recognizes.
Understanding these escape tactics is everything. It’s not that your immune system is weak—it’s that cancer is an incredibly clever and resourceful enemy. Each of these tricks gives us a potential target for a specific type of immunotherapy designed to counter that exact move.
The more we learn about a tumor's unique genetic and molecular profile, the better we can predict which immunotherapies will successfully unmask it. This personalized strategy is at the heart of modern oncology, which you can read more about in our guide on combining genomic data with immunotherapy for better outcomes. This is exactly why figuring out how immunotherapy works for cancer is so vital for today's treatments.
Understanding the Main Types of Cancer Immunotherapy
Now that we have a clearer picture of how cancer cleverly dodges the immune system, we can dive into the specific strategies immunotherapy uses to fight back. It isn't a single, one-size-fits-all treatment. Instead, think of immunotherapy as a diverse arsenal of sophisticated therapies, each designed to empower your body's natural defenses in a very specific way.
It’s a bit like a mechanic's toolbox. You wouldn't use a wrench to do a hammer's job. In the same way, we oncologists select the right immunotherapy based on the unique biological fingerprint of your cancer.
Let's break down the main categories. I’ll use some simple analogies to help explain how each one works to turn your immune system back into the powerful cancer-fighting force it was meant to be.
Immune Checkpoint Inhibitors: Releasing the Brakes
This is easily the most well-known form of immunotherapy today. As we covered, cancer cells can be sneaky, using "checkpoint" proteins like PD-L1 to essentially slam the brakes on T-cells, telling them to back off and leave the tumor alone.
Immune checkpoint inhibitors are a class of drugs that physically block this very interaction. They act like a shield, getting between the cancer cell and the T-cell so that the "off" signal never gets through. By releasing this brake, the T-cell is set free to recognize the cancer cell as a threat and attack it.
This approach doesn't create new immune cells; it simply unleashes the power of the ones you already have. It has been remarkably effective for a growing list of cancers, including melanoma, lung cancer, and kidney cancer.
The diagram below shows exactly how a cancer cell uses a checkpoint protein to shut down a T-cell—the precise mechanism these drugs are designed to disrupt.
The real-world results can be dramatic. For instance, the CheckMate 77T trial for non-small cell lung cancer showed what happens when you combine the checkpoint inhibitor nivolumab with chemotherapy before surgery. The rate of pathological complete response (meaning no detectable cancer left at the time of surgery) jumped to 25.3%, a massive leap from just 4.7% with chemotherapy alone. That’s more than five times as many patients becoming cancer-free.
CAR T-Cell Therapy: Engineering Supercharged Soldiers
Sometimes, the immune system needs more than just a green light. It needs a high-tech upgrade. That's where CAR T-cell therapy, a type of adoptive cell transfer, comes in. It represents one of the most personalized and powerful forms of cancer treatment available.
The process is like turning your own T-cells into elite, GPS-guided soldiers. Here’s a step-by-step look:
- Collect: We start by drawing your blood and collecting your T-cells.
- Reprogram: In a specialized lab, these cells are genetically engineered. We give them new, custom-built receptors on their surface called Chimeric Antigen Receptors (CARs).
- Multiply: The newly engineered CAR T-cells are grown and multiplied until there are millions of them.
- Infuse: Finally, this army of supercharged cells is infused back into your body. Their new receptors guide them directly to your cancer cells to launch a precise and devastating attack.
CAR T-cell therapy is often called a "living drug" for good reason. The engineered cells can continue to multiply in your body, creating a long-lasting, vigilant defense against the cancer. This approach has produced incredible results, particularly for patients with certain blood cancers like leukemia and lymphoma.
Cancer Vaccines: Teaching the Immune System What to Hunt
When we think of vaccines, we usually think of preventing diseases like the flu or measles. Cancer vaccines are different; they are typically used to treat a cancer that's already there. Their job is to teach your immune system what the enemy looks for.
Think of a cancer vaccine as a "most-wanted poster" that we show to your immune cells. The vaccine introduces a specific cancer protein, known as an antigen, training your immune system to recognize and hunt down any cell that displays that same protein. This helps your body mount a highly targeted attack squarely on the tumor.
These vaccines can even be personalized by creating them from a patient's own tumor tissue. This ensures the immune system is trained on the most relevant and specific targets for their cancer. This field is advancing quickly and holds incredible promise for creating durable, custom-tailored immune responses. You can explore more about the latest advances in cancer immunotherapy techniques in our dedicated article.
Monoclonal Antibodies: Marking Cancer for Destruction
Monoclonal antibodies are proteins created in a lab that are engineered to attach to specific targets on cancer cells. They can work in a few different ways, but one of their primary functions is to act like a bright red flag.
When these antibodies latch onto a cancer cell, they make it incredibly visible to the rest of the immune system. This "marking" makes it much easier for your body's natural killer cells to find and destroy the tumor. Some monoclonal antibodies are also designed to block the signals cancer cells need to grow, effectively cutting off their lines of communication.
Other Key Immunotherapy Approaches
The world of immunotherapy is broad and continues to expand. Beyond the major categories we've discussed, several other strategies are showing great promise.
- Oncolytic Viruses: These are viruses that have been modified in a lab so they preferentially infect and kill cancer cells, while leaving healthy cells alone. When a virus causes a cancer cell to burst open, it releases new tumor antigens, which can trigger an even broader immune attack against any remaining cancer.
- Cytokines: These are messenger proteins that the immune system uses to regulate its own activity. We can administer lab-made versions of cytokines, like interleukins and interferons, to stimulate a more aggressive, system-wide immune response against the cancer.
Each of these therapies uses a different tactic, but they all share the same fundamental goal: to re-engage your body’s powerful, natural defenses in the fight against cancer.
CAR T-Cell and Other "Living Drug" Therapies
If checkpoint inhibitors work by taking the brakes off your immune system, another groundbreaking approach basically builds you a brand-new, supercharged engine. These treatments are called cellular therapies, or sometimes adoptive cell transfer.
The core idea is both simple and incredibly sophisticated: we collect your own immune cells, give them a major upgrade in the lab, and then infuse them back into your body as a living, cancer-hunting army.
This is about as personal as medicine gets. We’re not using a drug made for thousands of people; the treatment itself is created from you, for you. It’s often called a "living drug" for a good reason—once these modified cells are back inside you, they can multiply and stand guard against cancer for months, or even years.
How We Engineer Your T-Cells with CAR T-Cell Therapy
The most famous example of this is CAR T-cell therapy. It's a stunning piece of bioengineering that turns your natural T-cells into precision-guided weapons pointed directly at your cancer.
You can think of it as giving your body's security guards a high-tech GPS that only locks onto cancer cells. Here’s how it unfolds:
- Collection: It starts with a process called apheresis, which is a bit like donating blood. We draw your blood, a machine separates out the T-cells, and the rest of the blood is returned to your body.
- Reprogramming: Your T-cells are then sent to a highly specialized lab. There, scientists use a safe, disabled virus to insert a new gene into them. This gene tells the T-cells to grow a special new receptor on their surface, called a Chimeric Antigen Receptor (CAR).
- Multiplication: These newly engineered CAR T-cells are then grown in the lab for a few weeks until they've multiplied into an army of hundreds of millions.
- Infusion: Finally, this powerful new army of cells is infused back into your bloodstream, much like a standard IV drip.
Once they’re back in your body, the CARs act like a homing device. They enable the T-cells to find a specific protein (an antigen) on the surface of your cancer cells, lock on, and launch a devastating attack.
CAR T-cell therapy is a game-changer. It has led to deep, lasting remissions for people with certain blood cancers—like leukemia, lymphoma, and multiple myeloma—who had run out of other good options.
For instance, in studies of patients with heavily pretreated multiple myeloma, one type of CAR T-cell therapy produced a response in 73% of them. Amazingly, 33% of those patients achieved a complete response, meaning no detectable cancer remained. Those are incredible results for a group who had already been through multiple other treatments. You can learn more by exploring the latest findings on CAR T-cell therapy for multiple myeloma.
Finding the Right Soldiers Already Inside the Tumor
Another powerful type of cellular therapy is called Tumor-Infiltrating Lymphocyte (TIL) therapy. This approach is built on a simple yet brilliant observation: the best immune cells for fighting your tumor might be the ones that have already figured out how to get inside it.
These cells, the TILs, have already recognized the tumor as an enemy. The problem is, they're usually outnumbered and exhausted, unable to win the fight on their own. TIL therapy is all about giving them overwhelming reinforcements.
The process looks like this:
- A surgeon removes a small piece of your tumor.
- In the lab, scientists carefully extract the TILs from that tumor tissue.
- These specific T-cells, already primed to recognize your cancer, are grown into an army of billions.
- This massive force of tumor-specific cells is then infused back into your body.
Unlike CAR T-cell therapy, TIL therapy doesn’t involve any genetic engineering. Instead, it just amplifies the natural anti-cancer response your body already started. This makes it a very promising option for solid tumors like melanoma.
Both CAR T-cell and TIL therapies show just how far we've come in our ability to work with the immune system to create potent and deeply personal cancer treatments.
What to Expect During Your Immunotherapy Treatment

It’s one thing to understand the science behind immunotherapy, but it’s another to know what the day-to-day experience will actually feel like. Knowing what’s coming can go a long way in easing anxiety and setting realistic expectations. The whole process is quite different from what many people associate with cancer care, like traditional chemotherapy.
Your journey will start with a thorough consultation and some key tests. Before you begin, your oncologist will almost certainly order biomarker tests on a sample of your tumor tissue. This is to check for specific molecular flags, like PD-L1, that immunotherapy drugs are designed to target. The results help us predict how likely the treatment is to work for you.
Your Treatment Schedule and Infusion Day
Most immunotherapies, particularly checkpoint inhibitors, are administered through an IV in an outpatient infusion center. How often you come in for treatment can vary quite a bit, depending on the specific drug you're receiving and the type of cancer you have.
A typical schedule might look like one of these:
- An infusion once every two, three, four, or even six weeks.
- The infusion itself is usually pretty quick, often taking just 30 to 60 minutes.
- You probably won't need the pre-medications often used in chemo, like steroids or anti-nausea drugs.
When you arrive for your appointment, a nurse will place an IV, and the immunotherapy drug will be infused slowly. You can settle in, read a book, or chat with a friend or family member. It’s a calm and generally straightforward process. The total length of your treatment course can also vary—some people stay on immunotherapy for up to two years, while others might stop sooner if it’s working well or if side effects become a concern.
Understanding Immunotherapy Side Effects
This is where immunotherapy really parts ways with chemotherapy. Because these drugs work by ramping up your immune system, the side effects aren't caused by direct damage to healthy cells. Instead, they stem from an overactive immune response.
We call these immune-related adverse events (irAEs). You can think of them as a sign that your immune system is fired up and doing its job—sometimes a little too enthusiastically. The issue is that instead of only attacking cancer cells, it can sometimes cause inflammation in healthy organs and tissues.
The key takeaway is that almost any "-itis" (meaning inflammation) can be a side effect. This includes colitis (inflammation of the colon), pneumonitis (lungs), hepatitis (liver), and dermatitis (skin).
Some of the more common, milder side effects include:
- Fatigue
- Skin rash or itching
- Diarrhea
- Flu-like symptoms
It is absolutely crucial that you report any new or worsening symptoms to your care team right away, no matter how minor they seem. Catching these side effects early is the best way to manage them, often with medications like steroids that can temporarily quiet the immune system.
New research is also looking at giving immunotherapy before surgery, an approach called neoadjuvant immunotherapy, to improve long-term outcomes. Some incredible trials have shown this can train T-cells to recognize tumor-specific targets, creating a lasting "memory" to help prevent the cancer from coming back. For example, at MSK, nearly 80% of patients with various cancers who had circulating tumor DNA (ctDNA) saw it cleared after receiving pembrolizumab before their surgery. You can read more about how liquid biopsies are guiding these promising cancer treatment advances on mskcc.org.
As you get started, you might also wonder how soon you'll see results. Our guide offers more detail on how long immunotherapy takes to work, as the timeline can be different from other cancer therapies.
Your Immunotherapy Questions, Answered
As you and your family think about starting immunotherapy, a lot of practical questions naturally come to mind. What’s the day-to-day really like? What can you expect? Let’s walk through some of the most common questions we hear from patients.
How Quickly Will I See Results?
This is a big one, and it's important to set the right expectations. Immunotherapy isn’t like chemotherapy, which can sometimes produce a rapid response. Instead, it works more deliberately by waking up and training your immune system—a process that simply takes time.
While every person’s journey is different, we typically don't expect to see significant changes on scans for several weeks to a few months. Your care team will be watching you closely during this initial phase, not just for signs of response but also to manage any side effects that pop up. Patience is a virtue here; the real goal isn't a quick fix but a deep, lasting response.
Can This Really Lead to Long-Term Remission?
Yes, it absolutely can. This is perhaps the most incredible aspect of immunotherapy. When it works, it doesn't just attack the cancer; it teaches your immune system how to recognize and control it for the long haul. This creates a powerful "immune memory."
What does that mean for you? It means your own body may be able to keep the cancer in check for years, sometimes even after you’ve finished active treatment. We’ve seen this happen for patients with advanced melanoma, lung cancer, and other diseases, achieving durable remissions that were almost unthinkable a decade ago. It’s a game-changer.
The true power of immunotherapy lies in its potential for long-term control. By turning your body's own defenses into a permanent surveillance system, we aim for a lasting shield against the cancer coming back.
Do You Use Immunotherapy with Other Treatments?
Definitely. In fact, combining therapies is often one of the smartest ways to fight cancer because it allows us to attack it from multiple directions at once. Immunotherapy is very frequently paired with other treatments to boost its effectiveness.
Some of the most common combinations include:
- With Chemotherapy: Chemo can break down cancer cells, causing them to release proteins (antigens) that basically act like a "wanted poster." This helps the newly activated immune cells find and destroy their targets more effectively.
- With Targeted Therapy: These drugs can hit specific weak spots in the cancer's defenses, making it much more vulnerable when the immune system comes knocking.
- With Radiation: Much like chemotherapy, radiation can damage tumors in a way that exposes them to the immune system, essentially "lighting up" the target for the T-cells.
Is Immunotherapy an Option for Everyone?
Not yet, but the list of cancers that can be treated with immunotherapy is growing all the time. Right now, it works best for tumors that have certain characteristics—or biomarkers—that make them more "visible" to the immune system. Things like high PD-L1 expression or a high tumor mutational burden (TMB) are good indicators.
It's become a frontline treatment for many people with melanoma, lung cancer, kidney cancer, bladder cancer, and certain lymphomas. For other cancer types, it's not yet a standard option. But clinical trials are constantly exploring new ways to make more tumors respond, and we expect its use to keep expanding for years to come.
At Hirschfeld Oncology, our focus is on building a plan that’s right for you. That might involve immunotherapy, low-dose chemotherapy, targeted agents, or a thoughtful combination designed to give you the best outcome with the fewest side effects. To talk about your specific situation, you can request a consultation with our team through our official blog.





.png)


.png)
.png)




