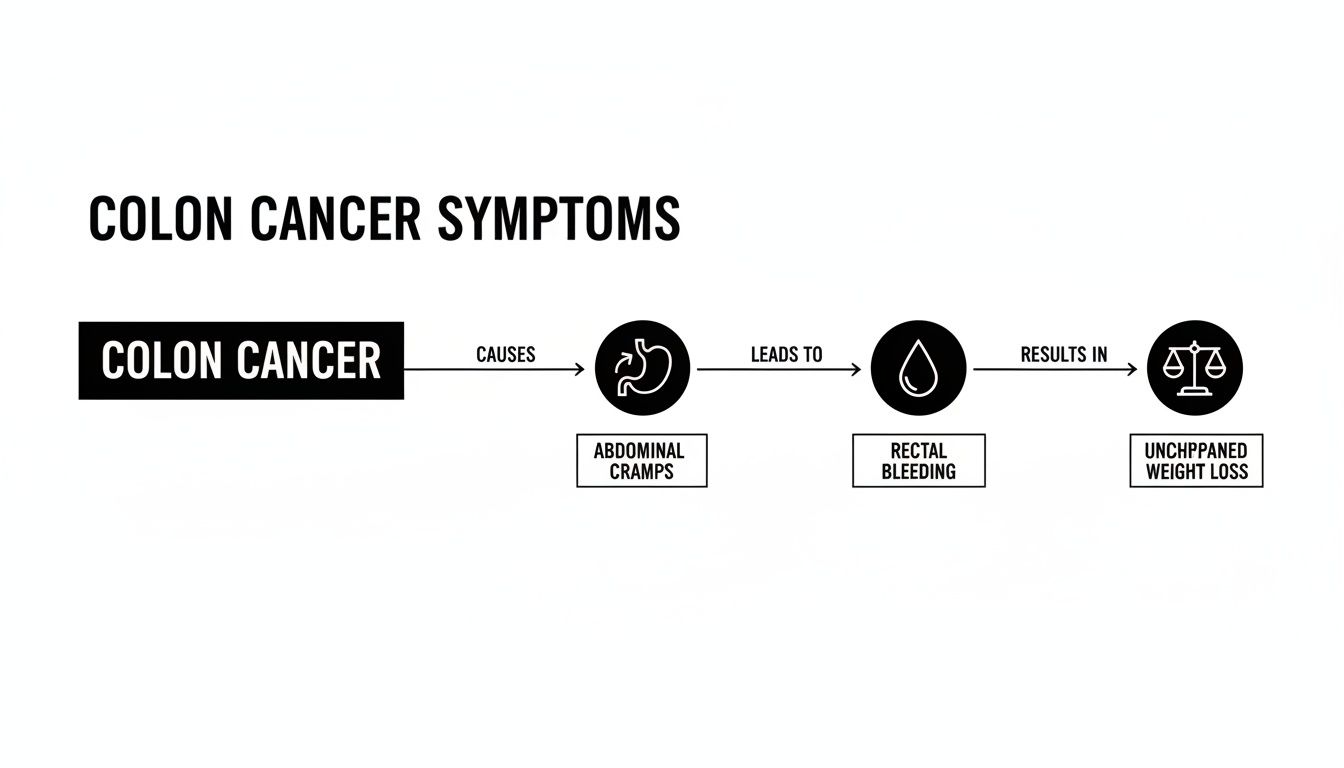
When it comes to colon cancer, the earliest signs are often subtle. They're easy to dismiss. We're talking about persistent changes in your bowel habits, like new diarrhea or constipation that just won't quit.
Other clues can include rectal bleeding, seeing blood in your stool, ongoing abdominal discomfort—think cramps, gas, or pain—and a nagging feeling that your bowel doesn't empty completely.
Understanding the First Clues Your Body Gives You
The tricky thing about colon cancer symptoms is that they often start as quiet whispers, not blaring alarms. It’s all too common for people to write them off as a minor stomach bug, stress, or something they ate.
But here’s the key: persistence. A single off day is normal. A pattern that lasts for weeks is not.
Think of your digestive system as a finely tuned pathway. When a growth, like a polyp, starts to develop in the colon, it can physically get in the way and disrupt the normal flow of things. This disruption is what triggers those early symptoms.
For instance, a change in your bowel habits isn't just random. It could be the direct result of a tumor creating a partial blockage, changing how stool moves through your colon.
Why Paying Attention Is More Important Than Ever
It’s a dangerous myth that colon cancer is just an "old person's disease." That's simply not true anymore. We're seeing a concerning rise in early-onset colorectal cancer, which means a diagnosis in people under 50.
In fact, a major study found that in 27 out of 50 countries, cancer rates in adults aged 25 to 49 are climbing, with some areas seeing annual increases as high as 4.0%. This shift makes it absolutely critical to pay attention to potential warning signs, no matter your age.
Here's a quick reference guide to help you recognize what to look for.
Quick Guide to Potential Early Signs of Colon Cancer
This table breaks down some of the most common early symptoms. While these can be caused by many other conditions, it's crucial to understand why they warrant a conversation with your doctor.
Remember, seeing one or more of these signs isn't a reason to panic, but it is a reason to act. Getting checked out is the only way to know for sure what's going on.
Key Takeaway: The most important thing to watch for is a persistent change from what's normal for you. An off day is one thing, but a new pattern that sticks around for several weeks is your body's signal to get it checked out by a healthcare professional.
A Deeper Look at Common Symptoms
It’s one thing to know what a symptom is, but it's another thing entirely to understand why it's happening. The early signs of colon cancer aren't random; they are the direct physical results of a growth interfering with how your digestive system is supposed to work.
Let's walk through the most common symptoms one by one. I'll use some simple analogies to connect the dots between what you might be feeling and what could be going on inside your colon.
Changes in Bowel Habits: The Roadblock Analogy
Think of your colon as a busy, one-lane highway where things usually move along smoothly. A colon tumor is like a partial roadblock that suddenly appears, disrupting the normal flow of traffic. This obstruction is the key to understanding why bowel habits can change so drastically and persistently.
- Constipation: When stool tries to get past this roadblock, it can get backed up, creating a traffic jam. The result is fewer bowel movements and stool that is harder and more difficult to pass.
- Diarrhea: Sometimes, the body tries to force liquid stool around the obstruction to clear the path. This can show up as sudden, watery diarrhea, which might even alternate with periods of constipation as the blockage continues to cause issues.
- Narrow Stools: If stool manages to squeeze past the tumor, it can be forced into a much thinner, pencil-like shape. This is a very specific sign that something is physically narrowing the passage inside your colon.
A single off day with your bowel movements is rarely cause for alarm. But if these changes stick around for several weeks and become your "new normal," it’s a clear signal that the highway isn't clear and needs to be checked out.
Rectal Bleeding: Why It Demands Attention
Seeing blood is always alarming, and it’s a symptom that should never be brushed aside. When it comes to colon cancer, bleeding happens because tumors are fragile, abnormal growths with their own delicate blood vessels.
As stool passes by, the friction can easily cause the tumor's surface to break and bleed. This can look a few different ways:
- Bright red blood: This usually means the bleeding is in the lower part of the colon or the rectum. The blood is fresh, so you might see it on the toilet paper or in the toilet bowl.
- Dark maroon or black stools: This suggests the bleeding is happening higher up in the colon. As the blood travels through your digestive system, it gets digested, turning it dark and tarry.
It’s tempting to blame rectal bleeding on something common like hemorrhoids. While that's often the cause, it's impossible to know for sure without a medical evaluation. Assuming it's nothing serious is a risk you shouldn't take.
Persistent Abdominal Discomfort
That ongoing cramping, gas, or pain in your belly? It’s often caused by that same roadblock effect. When a tumor partially obstructs the flow of stool and gas, it creates a backup. This buildup of pressure leads to bloating, cramping, and a general feeling of discomfort that just doesn't seem to quit.
You might also experience something called tenesmus—that nagging, persistent feeling that you need to have a bowel movement, even if you just went. This happens when a tumor in the rectum tricks the nearby nerves into thinking the bowel is still full.
These early signs of colon cancer can be difficult to recognize, contributing to often late diagnoses, especially in younger populations. Statistically, colorectal cancer among adults younger than 55 has increased from about 11% of all CRC cases in 1995 to an estimated 20% in recent years. Young adults frequently postpone seeking help because early symptoms like rectal bleeding or abdominal pain are often misattributed to benign conditions. To dive deeper into this trend, explore the findings from the American College of Surgeons about the dramatic rise in early-onset colorectal cancer.
Systemic Symptoms: Unexplained Weight Loss and Fatigue
Not all symptoms of colon cancer are in your gut. Some affect your entire body, and these are often the most subtle and easily overlooked.
Unexplained Weight Loss
Cancer cells are incredibly hungry. They grow and divide at a rapid pace, consuming a huge amount of your body's energy and calories. If you're losing weight without changing your diet or exercise habits, it could be a sign that these cells are burning through your body’s fuel reserves.
Constant Fatigue and Weakness
This symptom is very often tied to slow, chronic blood loss from the tumor. Over time, even a small, steady trickle of blood can lead to iron-deficiency anemia. Your body needs iron to make hemoglobin, the protein in red blood cells that carries oxygen.
Without enough iron, your body can't get the oxygen it needs to function, leading to a deep and persistent exhaustion that sleep just doesn't seem to fix.
Distinguishing Cancer From Common GI Issues
Let's be honest—when you're dealing with new or strange gut symptoms, it's easy to feel worried. A sudden bout of cramping or a change in your bathroom habits can send your mind racing. The reality is that many common, far less serious conditions can mimic the early signs of colon cancer. The trick is learning to spot the subtle but critical differences.
Things like Irritable Bowel Syndrome (IBS), Inflammatory Bowel Disease (IBD) like Crohn's or colitis, and even run-of-the-mill hemorrhoids can all cause abdominal discomfort or shifts in your bowel routine. But colon cancer often brings a distinct set of "red flag" symptoms that are less likely to show up with these other issues. This guide isn't for self-diagnosing, but for helping you have a smarter, more confident conversation with your doctor.
IBS vs. Colon Cancer Symptoms
Irritable Bowel Syndrome is a very common functional gut disorder. "Functional" just means the gut isn't working quite right, but there’s no physical damage or disease causing it. Both IBS and colon cancer can bring on cramping, bloating, gas, and cycles of diarrhea and constipation.
So, what's the difference? It really comes down to the presence of more alarming, systemic symptoms. While IBS can make you miserable, it doesn't cause you to lose blood, become anemic from iron deficiency, or drop pounds for no reason. These are signs that point to an actual disease process, not just a functional issue.
The Critical Difference: If your gut problems are paired with visible blood in the toilet, deep fatigue that could signal anemia, or weight loss you can't explain, the level of concern goes way up. This combination points beyond a typical IBS pattern and needs a doctor's attention right away.
The chart below lays out a few of the key symptoms that should absolutely prompt a call to your healthcare provider.
As you can see, symptoms like persistent cramps, any bleeding, and unexplained weight loss are interconnected red flags that point toward something more serious that needs to be checked out.
IBD And Hemorrhoids Compared To Colon Cancer
Inflammatory Bowel Disease (IBD), which includes Crohn's disease and ulcerative colitis, involves long-term inflammation of the GI tract. IBD shares a lot of symptoms with colon cancer, including rectal bleeding and abdominal pain, which can make it hard to tell them apart without a proper workup. In fact, having IBD for many years is a known risk factor for developing colon cancer, which is why people with an IBD diagnosis need regular screenings.
Hemorrhoids are just swollen veins in the rectum, and they are an incredibly common reason for seeing bright red blood on the toilet paper. This is probably the number one source of confusion and anxiety.
Here’s how a doctor starts to sort it out:
- The Color of the Blood: Bleeding from hemorrhoids is almost always bright red and happens right after you go. Blood from a tumor higher up in the colon has had more time to travel, so it can be darker—think maroon or even black and tarry. It can also be bright red if the tumor is low in the rectum.
- The Company It Keeps: Hemorrhoids don’t cause lasting changes in your bowel habits, ongoing belly pain, or weight loss. If you have bleeding plus any of those other symptoms, the suspicion for something more than hemorrhoids goes way up.
Symptom Comparison Colon Cancer vs Common GI Conditions
Sorting through these symptoms can be overwhelming, which is why we’ve put together this simple comparison table. It's designed to help you see the patterns and understand why a professional diagnosis is so essential.
The bottom line is that any new symptom that sticks around or just feels wrong deserves to be checked out. Knowing what to look for and how these conditions differ empowers you to seek help promptly and describe your concerns clearly to your doctor.
Understanding Your Risk and the Power of Screening
While knowing the early signs of colon cancer is incredibly important, the real goal is to stop it from ever starting. This means we need to shift our thinking from just reacting to symptoms to actively managing our risk. The first step is getting a clear picture of your own personal risk profile.
Colon cancer risks tend to fall into two buckets: things you can't change and things you can. It's vital to understand both so you can have a meaningful conversation with your doctor about how to best protect your health.

Unchangeable Risk Factors
Some risk factors are simply part of your personal story and genetic blueprint. You can't alter them, but knowing about them is powerful. It underscores why getting screened early and consistently is so critical for you.
- Age: Your risk for colon cancer climbs significantly after age 50. But we're seeing rates rise in younger adults, so age isn't the clear-cut line it used to be.
- Personal History of Polyps or Cancer: If you've had precancerous polyps or colorectal cancer in the past, your chances of it returning are higher.
- Family History: A first-degree relative—a parent, sibling, or child—with colon cancer or polyps raises your risk. This risk gets even higher if they were diagnosed before age 50 or if multiple family members are affected.
- Inherited Genetic Syndromes: Conditions like Lynch syndrome and Familial Adenomatous Polyposis (FAP) can dramatically increase your risk. Our guide on whether cancer can be genetic dives deeper into these connections.
- History of Inflammatory Bowel Disease (IBD): The chronic inflammation caused by conditions like Crohn's disease or ulcerative colitis can, over time, increase the risk of developing colon cancer.
Lifestyle Risk Factors You Can Influence
This is where you have the power to make a real difference. Your daily choices can significantly lower your risk profile.
Think of it like tending a garden. By controlling the soil, water, and sunlight, you create an environment where healthy plants thrive and weeds struggle to take hold. In the same way, a healthy lifestyle fosters an internal environment that is far less hospitable to cancer.
Here are the key lifestyle factors to focus on:
- Diet: A diet low in fiber but high in red and processed meats has been clearly linked to higher risk.
- Physical Inactivity: Living a sedentary lifestyle is a well-known risk factor.
- Obesity: Being significantly overweight increases the risk of both developing and dying from colon cancer.
- Smoking and Alcohol Use: Both habits are tied to a greater likelihood of the disease developing.
Screening: The Most Powerful Prevention Tool
If you take one thing away from this, let it be this: screening saves lives. It is the single most effective weapon we have against colon cancer. Why? Because it can find and remove precancerous polyps before they ever get the chance to turn into cancer. It's not just about early detection; it's about outright prevention.
Colorectal cancer is the third most common cancer globally and the second leading cause of cancer-related deaths. In 2020, there were approximately 1.9 million new cases and over 930,000 deaths worldwide. The good news is that effective screening programs have directly contributed to falling incidence and mortality rates in many countries. You can review the global statistics from the World Health Organization to understand the full impact.
The American Cancer Society now recommends that people at average risk start regular screening at age 45. This is a shift from the old guideline of 50, a direct response to the rising rates of colon cancer in younger people.
But "average risk" is the key phrase here. If you have any of the increased risk factors we just discussed—like a family history or a personal history of IBD—your doctor will almost certainly recommend you start screening much earlier, and possibly more often. There are several screening options available, from simple stool-based tests to visual exams like a colonoscopy. Your doctor is the best person to help you decide which is right for you.
Navigating the Diagnostic Journey
Knowing what to expect can take a lot of the fear out of the unknown. Once you’ve made that call to the doctor about your symptoms, you’ve already taken the most important step. You’re not just sitting with your worries anymore; you're taking action.
Let's walk through what the diagnostic process usually looks like. The goal here is to demystify everything, from that first conversation with your doctor to the definitive tests that give you clear answers. Understanding why each step is necessary can help you feel more prepared and in control.
Preparing for Your First Appointment
That first meeting with your doctor is the starting point for everything that follows. Coming in prepared can make a world of difference. Think of it like you're the lead detective on your own case, and you're bringing the first round of evidence to the expert.
The more specific you can be, the clearer the picture becomes for your doctor. Just saying "I've been feeling off" is a lot harder to work with than sharing documented observations.
Here’s how you can get ready:
- Track Your Symptoms: For a week or two before your visit, keep a simple log. Note the symptom, when it occurs, how long it lasts, and what—if anything—seems to trigger it or make it better.
- Know Your History: Be prepared to talk about your personal and family medical history. It's especially important to mention if any relatives have had colon cancer or polyps.
- Write Down Your Questions: It’s so easy to forget what you wanted to ask once you're in the exam room. Jot down your questions beforehand to make sure you get the answers you need.
Key Tip: Don't minimize what you're experiencing. If you've seen blood in your stool or had a nagging change in bowel habits, say so directly. This isn't the time for embarrassment—clear, honest communication is the fastest path to an accurate diagnosis.
The Initial Evaluation and Physical Exam
During your appointment, your doctor will listen to everything you've been experiencing and go over your medical history. They’ll then perform a physical exam, which usually involves gently pressing on your abdomen to check for any tenderness, swelling, or masses.
Your doctor might also perform a digital rectal exam (DRE). It can sound a bit intimidating, but it’s a very quick and simple procedure. The doctor just inserts a gloved, lubricated finger into the rectum to feel for any unusual lumps or growths. Based on all of this, they'll decide what comes next, which often involves blood work and a referral for a closer look inside your colon.
The Colonoscopy: The Gold Standard Test
If your symptoms or risk factors point toward a potential problem in your colon, your doctor will almost certainly recommend a colonoscopy. For good reason—it’s considered the "gold standard" for both detecting and preventing colon cancer.
You can think of a colonoscopy as a fact-finding mission inside your colon. A specialist, called a gastroenterologist, uses a colonoscope—a thin, flexible tube with a tiny light and camera on its tip—to get a direct look at the entire inner lining of your colon.
What makes a colonoscopy so powerful is its dual purpose:
- It Finds the Problem: The high-definition camera sends a live video feed to a monitor, allowing the doctor to spot any polyps or other suspicious areas that could be the earliest signs of trouble.
- It Solves the Problem: If the doctor finds polyps, they can usually remove them on the spot during the procedure. Since most colon cancers start as benign polyps, taking them out is a direct form of cancer prevention.
If a suspicious area looks more like a tumor, the doctor will take a small tissue sample, called a biopsy, for lab analysis. A biopsy is the only way to know for sure if cancer is present. The results will guide the next steps and help determine the specific type of cancer you might be dealing with. To get a better sense of what follows a diagnosis, our guide on the different colon cancer stages can give you a clearer picture of the road ahead.
What to Do Next: Taking Control of Your Health
Knowing the early signs of colon cancer is one thing, but acting on that knowledge is what truly makes a difference. The most powerful thing you can do is listen to what your body is telling you and then get the right medical advice without delay. This is how you move from worrying to taking charge.
Whether you're noticing symptoms yourself, you know you have a few risk factors, or you're looking out for a loved one, the next step is to be intentional. Don't just cross your fingers and hope things get better. It's time to be proactive.
If You're Noticing Symptoms
If anything you've read here sounds familiar, your path forward is clear.
- Keep a simple log. Jot down what you're experiencing, when it started, and how often it happens. This kind of detail is incredibly helpful for your doctor.
- Make the call. Schedule an appointment with your primary care doctor or a gastroenterologist. Don't downplay your concerns—be upfront about "red flag" symptoms like rectal bleeding or dropping weight without trying.
- Be your own advocate. You are the expert on your own body. If a symptom isn't going away and you have that nagging feeling that something is off, keep pushing for answers.
If You Have Risk Factors but No Symptoms
Feeling great is wonderful, but if you have risk factors like a family history of colon cancer, you can't be passive. You need a screening plan. Remember, screening isn't just about finding cancer—it's often about preventing it in the first place by removing polyps before they have a chance to turn into cancer.
Think of your health as a partnership between you and your medical team. When you take these proactive steps, you shift from a place of anxiety to a position of control. At Hirschfeld Oncology, we’ve seen firsthand that informed patients get the best results, and our goal is to give you clarity and support at every turn.
For anyone in the New York City area, including Brooklyn and Williamsburg, our team at Hirschfeld Oncology is here to guide you. Dr. Hirschfeld and our staff can offer a timely consultation to go over your symptoms, assess your personal risk, and create a clear diagnostic plan.
Contact our office to schedule a consultation and take that first, crucial step.
Your Questions About Colon Cancer Symptoms, Answered
It's completely normal to have questions when your gut health feels off. New or lingering symptoms can be worrying, so let's walk through some of the most common concerns about the early signs of colon cancer to help you get the clarity you need.
Can Stress Cause Symptoms That Mimic Colon Cancer?
Absolutely. Stress is notorious for wreaking havoc on our digestive systems, often leading to cramping, bloating, and changes in bowel habits. These are also hallmark signs of conditions like Irritable Bowel Syndrome (IBS), which stress can definitely make worse.
But here’s the crucial distinction: stress doesn't cause the major red flag symptoms of colon cancer. We're talking about things like rectal bleeding, losing a significant amount of weight without trying, or the bone-deep fatigue that comes with iron-deficiency anemia. If you're experiencing any of these, it's vital to see a doctor and not just write it off as stress.
What Age Is “Too Young” to Worry About These Symptoms?
There is no such thing as "too young." You should take any persistent, unexplained symptom seriously, no matter your age. While routine screening for people at average risk now begins at 45, we're seeing a troubling rise in colorectal cancer diagnoses among younger adults.
The old idea that this is just a disease for older folks is a dangerous myth that can cause people to ignore symptoms and delay getting help. If you have rectal bleeding or a change in your bowel habits that lasts for more than a few weeks, it's time to talk to your doctor. Your age doesn't matter; the symptom does.
Key Insight: Don't focus on your age. Focus on the symptom. If it's new, persistent, and doesn't feel right, that's your body telling you to get it checked out.
I Have Hemorrhoids. Can I Just Ignore a Little Rectal Bleeding?
No, you should never assume that rectal bleeding is just your hemorrhoids. While it’s true that hemorrhoids are a very common cause of bright red blood on the toilet paper, colon cancer can show up in the exact same way. There's simply no way to tell the difference on your own.
Any time you see blood—whether it's on the paper, in the toilet bowl, or mixed in with your stool—it's a signal to call your doctor. A proper medical evaluation is the only way to confirm the cause, rule out anything more serious, and give you the peace of mind you deserve.
At Hirschfeld Oncology, we know that good information is the foundation of good health. If you're dealing with symptoms that concern you and are looking for guidance in the New York City area, our team is here to help you find answers with compassion and expertise. To explore your diagnostic options with our specialists, we invite you to learn more on the Hirschfeld Oncology blog.





.png)


.png)
.png)




