When you hear "radiation therapy," it's easy to feel a bit of uncertainty. Let's clear that up. At its core, radiation therapy is a highly focused treatment that uses powerful, high-energy waves or particles to damage the DNA inside cancer cells. This damage stops them from growing and multiplying, which ultimately causes them to die off.
While it's incredibly effective at zeroing in on tumors, the energy can sometimes affect healthy cells nearby. This is what leads to side effects, which can vary a great deal from person to person depending on the area being treated and other individual factors.
What Is Radiation Therapy and How Does It Work?
Think of radiation therapy like a meticulously planned, high-tech sniper mission. The goal is to take out the enemy—the cancer cells—while keeping the surrounding civilians, your healthy tissues, as safe as possible. The "bullets" in this case are invisible beams of high-energy rays, much like X-rays but significantly more powerful.
These beams are aimed directly at the tumor, where they scramble the genetic code (the DNA) inside the cancer cells. Here’s why that works so well: cancer cells are notorious for dividing and growing at a frantic pace. This constant activity makes their DNA particularly vulnerable to damage. When the DNA is hit hard enough, the cell loses its ability to replicate and eventually self-destructs. Most of your healthy cells, on the other hand, divide much more slowly, giving them time to repair the minor damage they might sustain. It’s this fundamental difference that makes radiation such a powerful weapon in the fight against cancer.
The Purpose of Radiation Therapy
Radiation isn't a one-size-fits-all solution; it's a versatile tool that your oncology team can use in a few key ways, depending on your specific situation.
- To Cure Cancer: Sometimes, radiation is the main event. It might be used on its own to completely destroy a tumor or to clean up any cancer cells left behind after surgery (adjuvant therapy).
- To Shrink Tumors Before Other Treatments: This is called neoadjuvant therapy. Hitting a tumor with radiation beforehand can make it smaller and more manageable, which can lead to a more successful surgery.
- To Prevent Cancer From Coming Back: Even after a tumor is gone, microscopic cells can linger. Radiation can be used to target the area and reduce the chances of a recurrence.
- To Relieve Symptoms: For advanced cancers, the goal might shift to improving quality of life. Palliative radiation can shrink tumors that are causing pain, bleeding, or pressure, offering significant relief.
The demand for this kind of precise, effective treatment is growing. The global radiotherapy market is expected to jump from USD 8.55 billion in 2025 to more than USD 14 billion by 2032. This reflects its vital role in cancer care across the world. You can read more about these market trends and their impact on treatment innovation.
Radiation therapy isn't an instant fix. The damage to cancer cells builds up over time with each treatment session. In fact, the effects continue to work for weeks or even months after your last appointment as the targeted cells slowly die off.
It’s also important to know that radiation often works hand-in-hand with other treatments. Your doctor might recommend it alongside chemotherapy or immunotherapy, and learning about the relationship between chemo and radiation can help you better understand your comprehensive treatment plan.
Understanding the Treatment Process
Your journey with radiation starts with a crucial planning session known as a "simulation." Think of it as creating a detailed battle map. You'll have imaging scans, like a CT scan, so your team can pinpoint the exact size, shape, and location of the tumor.
Using this map, a team of experts—including a radiation oncologist, a medical physicist, and dosimetrists—calculates the perfect angles and dosage. Their job is to design a plan that delivers a powerful blow to the cancer while carefully avoiding healthy organs and tissues as much as possible. This highly personalized plan ensures every single treatment is as safe and effective as it can be.
To help simplify these concepts, here is a quick overview of what radiation therapy involves.
Radiation Therapy At a Glance
This dedicated team works together behind the scenes, using advanced technology and careful planning to make sure your treatment is tailored specifically for you.
What to Expect: Navigating Short-Term Side Effects During Treatment

As you get started with radiation therapy, your body kicks into high gear. It's working overtime to repair healthy tissues while clearing away cancer cells damaged by the treatment. This is an intense process that demands a huge amount of energy, which is why most people experience some short-term, or acute, side effects.
These effects aren't a sign that something is wrong; in fact, they show the treatment is working. They tend to pop up a few weeks into your treatment schedule and typically fade away within a few weeks after your last session. Knowing what might be coming can make a world of difference in how you manage it.
The Deep Tiredness: Coping with Radiation Fatigue
Fatigue is hands down the most common side effect people report. This isn't just your everyday tiredness—it's a bone-deep exhaustion that doesn't always go away with a good night's sleep. It happens because your body is pouring resources into healing the healthy cells that get caught in the crossfire of the radiation beams.
It can be incredibly frustrating, but trying to "push through it" often backfires. The best approach is to listen to your body and be strategic with your energy.
Here are a few things that can help:
- Work with your energy peaks. Tackle your most important tasks whenever you feel your best, which for many people is in the morning.
- Try a power nap. A short nap of just 20-30 minutes can do more to recharge you than a long, groggy sleep in the middle of the day.
- Move a little. It sounds like the last thing you'd want to do, but gentle movement, like a slow walk around the block, can actually give you a surprising energy boost.
- Lean on your support system. Let friends and family take things off your plate. This is the time to say "yes" to offers of help with meals, errands, or childcare.
Soothing Your Skin in the Treatment Area
Think of how your skin feels after a sunburn—that's a good way to imagine how the skin in the treatment area might react. Radiation therapy affects any cells that divide quickly, and that includes your skin cells. You might start to see some redness, itching, peeling, or dryness.
Taking gentle care of this skin is absolutely essential for your comfort and to prevent more serious irritation. Your care team will give you specific instructions, but a few general rules of thumb can make you much more comfortable.
A Quick Word on Skin Products: Before you put any lotion, cream, or ointment on the treated skin, please check with your radiation oncology team. Some common ingredients, especially metals, can actually interfere with treatment and make your skin reaction worse.
Here’s how to protect your skin:
- Wash the area gently with lukewarm water and a mild, unscented soap.
- Pat your skin dry with a soft towel. No rubbing!
- Choose loose, soft clothing (cotton is great) to avoid friction against the sensitive area.
- Shield your skin from the sun. The treated area will be extra sensitive to sunlight for a long time. Cover up with clothing or, if approved by your team, use a high-SPF, broad-spectrum sunscreen.
Don't be alarmed if you experience these issues. Studies show that skin reactions happen in up to 90% of patients, and significant fatigue affects up to 80% of people. The good news is that these are temporary and manageable. Plus, modern advances like 4D treatment planning have cut down on these toxicities by 20-40%, making today's treatments much more precise. You can learn more about recent radiotherapy advancements that are improving patient experiences.
Understanding Localized Hair Loss
When people hear "radiation," they often think of losing all their hair. But unlike some types of chemotherapy that affect the whole body, hair loss from radiation is localized—it only happens in the specific area being treated. If you're having radiation to your head, you can expect to lose hair on your scalp. If it's aimed at your leg, you’ll only lose hair on that part of your leg.
This happens for the same reason your skin reacts: radiation damages the fast-growing cells in hair follicles. Hair usually starts to fall out two or three weeks after treatment begins. Whether it grows back depends on the total dose of radiation you receive. For many, it does return, though sometimes with a slightly different color or texture. In the meantime, be kind to your scalp and keep it protected from the sun.
What to Expect Down the Road: Long-Term and Late Effects
Finishing your last radiation session is a huge milestone, but your body’s healing journey continues long after. As healthy tissues recover and the last of the cancer cells are cleared away, you might notice some new changes. These are known as long-term or late effects, and they can surface months or even years after you’ve wrapped up treatment.
Think of it like a shoreline after a storm. The immediate impact is over, but the landscape has been subtly reshaped, and some of those changes only become apparent over time. The radiation can cause gradual, slow-developing shifts in healthy tissues.
It's crucial to know that these effects are not guaranteed. Many people have very few, if any, lasting issues. The goal here is to know what to keep an eye on so you can stay in the driver's seat of your long-term health.
Why Tissues Can Stiffen: Understanding Fibrosis
One of the more common late effects you might hear about is fibrosis. It’s simply the medical term for scarring or stiffening that can happen in the healthy tissues that were in the treatment area. It’s a result of the body’s healing process kicking into overdrive, creating extra fibrous tissue.
Imagine a soft, stretchy sweater. Over time, a spot that was repeatedly stressed might become a bit stiff or less flexible. In the same way, radiation can cause tissues in your skin, lungs, or other areas to lose some of their natural give, which can sometimes impact how they function.
For instance, fibrosis in the lung tissue after chest radiation could cause a nagging cough or make you feel short of breath. In the skin, it might just feel a bit thicker or tighter than it used to.
When Fluid Gets Trapped: A Look at Lymphedema
Another potential late effect, especially if your treatment involved lymph nodes, is lymphedema. Your lymphatic system is your body’s plumbing, clearing out fluid and waste. Radiation can sometimes damage these delicate channels, causing a sort of plumbing backup.
If the fluid can’t drain properly, it can collect in a nearby arm or leg, causing swelling. This can feel like a mild puffiness or a more significant heaviness and tightness. While lymphedema is a chronic condition, it is very manageable with the right care from specialists.
Being proactive is everything. The sooner you spot and manage any late effects, the better your long-term quality of life will be. This is exactly why your follow-up appointments and survivorship care are so important.
How Different Organs Can Be Affected
The specific late effects you might need to watch for depend entirely on which part of your body was treated. Every organ has a different job and reacts to radiation in its own way.
Here are a few examples of what this can look like:
- Heart: When the chest is treated, there’s a potential for an increased long-term risk of heart conditions. Your radiation oncologist took great care in planning your treatment to protect your heart as much as technology allows.
- Bowel: Radiation to the pelvis or abdomen can sometimes lead to chronic bowel changes, like lasting diarrhea, urgency, or rectal bleeding.
- Brain: Treatment to the brain can occasionally lead to cognitive shifts—that frustrating "brain fog" that can mess with your memory or focus—that develop down the line.
- Mouth and Throat: For people treated for head and neck cancers, late effects might include a permanently dry mouth or changes in swallowing if salivary glands or throat muscles were affected.
Reading about these possibilities can feel overwhelming. But remember, today’s radiation technology is incredibly precise, designed specifically to minimize these very risks. Your care team always balances the powerful benefits of treatment against the potential for long-term effects. Staying in touch with them and never skipping a follow-up is your best strategy for a healthy future.
How Side Effects Differ Based on Treatment Area
Radiation therapy is incredibly targeted. Think of it like a spotlight in a dark room—only what's in the beam gets illuminated. This precision means the effects of radiation therapy are almost always localized to the specific part of your body receiving treatment.
Someone getting radiation to their chest won’t have the same side effects as a person treated for a brain tumor. It’s a simple but crucial concept to grasp: the radiation beam only affects the cells in its direct path. Knowing this helps set realistic expectations for your own treatment journey, as the healthy organs and tissues near the tumor are what determine the side effects you might face.
Let's break down what you might expect based on where your treatment is focused. The following table gives a quick snapshot of common acute side effects you might encounter depending on the part of your body being treated.
Common Side Effects by Radiation Treatment Area
Remember, this is a general overview. Your own experience will be unique, and your care team will give you a much more detailed picture of what to expect and how to manage it.
Head and Neck Treatment Effects
When radiation is aimed at the head and neck, it can affect the many delicate structures in this area, like your salivary glands and the lining of your mouth and throat. The goal, of course, is to hit the cancer cells while protecting these vital functions as much as possible.
You might experience things like:
- Dry Mouth (Xerostomia): The salivary glands are quite sensitive and may produce less saliva. This can lead to a persistent dry feeling that makes tasting and swallowing tricky.
- Mouth Sores: The cells lining your mouth divide quickly, and radiation can inflame them. This can cause painful sores that make eating a real challenge.
- Taste Changes: It’s very common for people to report that food tastes metallic, bland, or just "off" during and after treatment.
- Difficulty Swallowing: Swelling or soreness in the throat, a condition called mucositis, can make it uncomfortable to swallow even soft foods.
These side effects are a small price to pay for what can be a life-saving treatment. Globally, 50-60% of cancer patients receive radiation, and it can boost five-year survival rates by as much as 70% for certain head and neck cancers. You can learn more about the global impact of radiation oncology and its success.
Chest Area Treatment Effects
Radiation pointed at the chest—for cancers like lung, esophageal, or lymphoma—will mostly affect the organs inside your chest cavity. The lungs and esophagus are often right in the treatment field, which leads to a very specific set of potential side effects.
The side effects you experience are a direct result of anatomy. Radiation affects the cells it passes through on its way to the tumor. If it passes through your esophagus to reach a lung tumor, you may feel some temporary irritation there.
Patients might develop:
- Cough or Shortness of Breath: This can happen if the lung tissue gets inflamed, a temporary condition called radiation pneumonitis.
- Sore Throat or Esophagitis: If your esophagus is in the beam's path, it can get irritated. This can feel a lot like heartburn or cause pain when you swallow.
Abdomen and Pelvis Treatment Effects
Your abdomen and pelvis are home to your digestive and reproductive systems, which are full of rapidly dividing cells. When this area is treated for cancers like colorectal, prostate, or cervical cancer, the side effects are usually related to digestion and urination.
You might notice symptoms such as:
- Nausea and Vomiting: Radiation can irritate the stomach lining and sometimes trigger the part of the brain that controls nausea.
- Diarrhea: The lining of the intestines can get inflamed, leading to more frequent or loose bowel movements for a while.
- Bladder Irritation: This can show up as a frequent urge to urinate or a burning sensation when you do.
The infographic below illustrates some of the long-term effects that can develop over time, which also vary based on the treatment area.
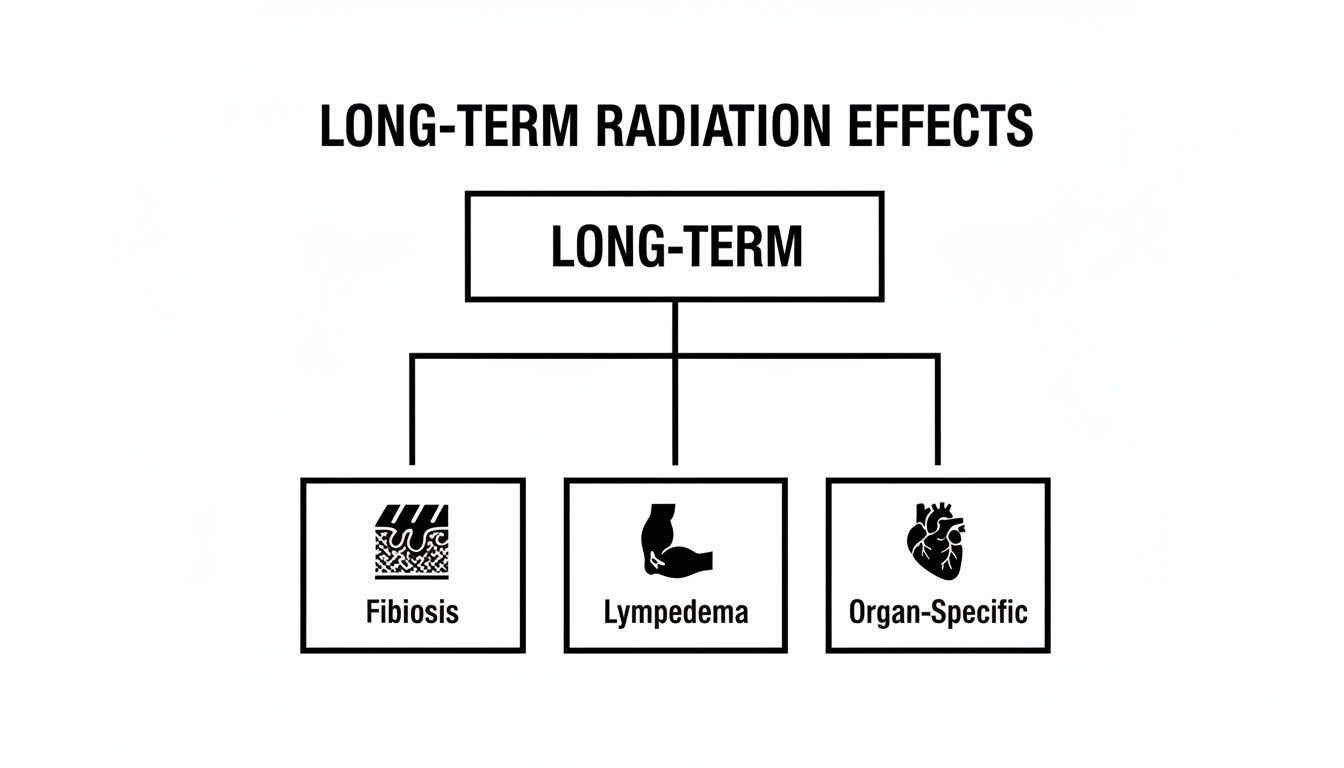
This visual helps show how late effects can appear months or years later as tissue stiffening (fibrosis), fluid buildup (lymphedema), or damage to specific organs that were in the treatment field.
Brain Treatment Effects
Treating a brain tumor demands incredible precision to protect delicate neural tissues. Here, side effects are often related to inflammation and which specific part of the brain is being treated.
Common challenges you might face during brain radiation include:
- Headaches: Swelling in the brain can create pressure, causing headaches that are usually well-managed with medication.
- Fatigue: This is an extremely common side effect. Your body is working overtime to repair healthy brain cells, and that takes a lot of energy.
- Cognitive Changes: Some people experience what they call "brain fog"—feeling a bit fuzzy, having memory issues, or finding it hard to concentrate.
- Localized Hair Loss: Hair will only fall out on the part of your scalp where the radiation beams exit your head.
Your care team will be watching you very closely for any of these effects. They can provide medications, like steroids, to manage swelling and keep you as comfortable as possible. It’s absolutely essential to keep an open line of communication about any new or worsening symptoms—it's the best way to stay safe and feel your best during treatment.
Practical Strategies for Managing Symptoms and Finding Support

Tackling the side effects of radiation therapy is just as crucial as the treatment itself. By adopting some practical and gentle self-care habits, you can make a real difference in your comfort and overall well-being. This isn't about powering through the discomfort; it’s about giving your body the support it needs to heal.
These strategies are all about simple, doable steps you can weave into your daily life. From what’s on your plate to how you talk with your care team, every little effort adds up to a better experience. Think of this as your personal playbook for navigating treatment with more confidence and control.
Nourishing Your Body During Treatment
Good nutrition is your secret weapon against fatigue and other side effects. While radiation can sometimes mess with your appetite or the taste of food, fueling your body is non-negotiable. So, let’s focus on what you can control, starting with smart food and hydration choices.
- Eat Small, Frequent Meals: When a big meal feels like too much, try eating smaller portions more often. This keeps your energy levels from crashing and is often much easier on a sensitive stomach.
- Prioritize Protein and Calories: Your body is working overtime to repair healthy cells, and it needs extra fuel for the job. Try to include protein-rich foods like eggs, yogurt, lean meats, or beans to support this healing process.
- Stay Hydrated: Dehydration is a surefire way to make fatigue and other symptoms feel worse. Aim for 8-12 cups of fluid each day. Water is your best bet, but don’t forget that soups, smoothies, and watery fruits like melon count, too.
If you’re really struggling with appetite loss or taste changes, don't be afraid to ask for a referral to a dietitian. They have all sorts of creative tricks to help you get the nutrients you need to stay strong.
Communicating Effectively With Your Care Team
Think of your oncology team as your most important partner in this process. They have a whole arsenal of tools and medications to help with just about every challenge, from nausea to skin rashes, but they can't help if they don't know what's going on.
"Keep your radiation team up-to-date with your symptoms. I have learned that this is not complaining — it is informing."
This piece of wisdom from a patient says it all. Being open isn't complaining; it’s giving your team the intel they need to give you the best care possible. Never downplay what you're feeling. If you're nauseous, they have powerful anti-nausea meds. If your skin hurts, they can recommend specific creams like Aquaphor that won't interfere with your treatment. You can find more great advice in our guide on managing side effects of cancer treatment.
Prioritizing Gentle Self-Care and Emotional Support
The physical side of radiation is only half the battle. Taking care of your emotional and mental health is just as vital for getting through this journey. Building a few gentle, restorative practices into your routine can make a world of difference.
Here are a few things that really work:
- Prioritize Rest: Your body will tell you when it needs a break, so listen to it. When you feel tired, rest. Sometimes short naps of 20-30 minutes can be more refreshing than a long sleep and are great for fighting that deep-seated fatigue.
- Incorporate Gentle Movement: It might sound backward, but light activity, like a slow walk, can actually boost your energy. The key is to stay as active as you comfortably can without ever pushing yourself to exhaustion.
- Protect Your Skin: Treat the skin in the treatment area like a newborn’s. Use lukewarm water, gently pat it dry, and wear soft, loose clothing. Most importantly, keep it completely out of the sun—it will be incredibly sensitive.
- Connect With Support Systems: You are not in this alone. Whether it's talking to a therapist, joining a support group, or just leaning on good friends and family, having an outlet for the emotional rollercoaster of treatment is essential. Whatever you’re feeling, it’s valid.
Knowing When to Call Your Doctor and Planning What’s Next
Once your last radiation session is over, the real healing begins. Think of your care team as your partners for the long haul, not just during active treatment. Keeping them in the loop and paying close attention to your body are the most important things you can do as you recover. Your healing timeline is your own, and being gentle with yourself is key.
Most side effects will fade with time, but it’s really important to know which symptoms are just part of the normal healing process and which ones need a quick call to your doctor or nurse. Never second-guess reaching out if something feels off.
Red Flags: When to Seek Immediate Medical Advice
Please get in touch with your care team right away if you experience any of the following. This isn't meant to scare you—it's about being safe and catching potential issues early.
- A fever of 100.4°F (38°C) or higher, or if you get the chills.
- Pain that isn't touched by the medication you were prescribed.
- Any new or worsening shortness of breath.
- Sudden confusion, a severe headache, or feeling dizzy.
- Nausea or vomiting so persistent you can't keep liquids down.
- Severe diarrhea or other signs of dehydration, like dark urine or a very dry mouth.
Think of it this way: telling your oncology team about a new symptom isn’t complaining. It’s giving them vital information they need to take the best care of you. You never have to just "tough it out."
Knowing what to look for puts you in the driver's seat of your own health. Your follow-up appointments are crucial for tracking your progress and managing any long-term effects. To make the most of those visits, you might want to look over this list of questions to ask your oncologist beforehand so you don't forget anything important.
The path after radiation treatment has its ups and downs, but you’re not walking it alone. By listening to your body and staying connected with your medical team, you can move forward through recovery with confidence.
Answering Your Top Questions About Radiation Effects
It’s completely normal to have a lot of questions as you prepare for radiation therapy. Getting straight answers can make the whole process feel less overwhelming and put you back in the driver's seat. Let's tackle some of the most common questions we hear from patients every day.
Will Radiation Therapy Make Me Radioactive?
This is a huge concern for many people, and for most treatments, the answer is a simple and reassuring no.
The vast majority of patients receive what’s called external beam radiation. Think of it like a highly targeted, powerful X-ray. The radiation beam passes through your body to treat the cancer cells, and the moment the machine is turned off, the radiation is gone. You can immediately and safely be around anyone—including children and pregnant women.
The only exception is a less common treatment called brachytherapy, where a radioactive source is temporarily placed inside your body. If this is part of your treatment plan, your care team will give you very specific, easy-to-follow safety instructions for the short time it’s needed.
How Long Do Radiation Side Effects Actually Last?
Everyone’s body responds differently, so there’s no single timeline. Generally, we see acute side effects, like fatigue and skin redness, start to appear a couple of weeks into treatment.
These symptoms tend to be at their most noticeable near the end of your treatment course. Once you have your final session, most of these will gradually improve over the next two to four weeks. Fatigue, however, can be stubborn and sometimes stick around for a few months as your body dedicates energy to healing.
That’s why we stress the importance of follow-up care. Some "late" effects can show up months or even years down the road, and staying connected with your team helps us manage them early.
"Think of radiation therapy like a marathon, not a sprint. No awards are given to patients who opt for fewer medications to manage symptoms and side effects. Take what helps you feel good. There’s not an ounce of shame in prioritizing comfort."
Can I Still Work During My Treatment?
Many people successfully continue to work, but it almost always requires a few adjustments. The biggest hurdle for most is fatigue. It’s not just feeling tired; it’s a deep, physical exhaustion that can make a full-time schedule feel impossible.
This is a good time to talk with your employer about options like flexible hours, working from home, or temporarily reducing your workload. The most important thing is to listen to your body.
- Rest when you need to. Pushing through the fatigue will only make it worse.
- Try some light movement. It sounds counterintuitive, but a short, gentle walk can actually give you a little energy boost.
- Be strategic with your energy. Tackle your most important tasks when you feel your best.
Your care team is here to help you figure out how to balance work, life, and treatment in a way that feels manageable and safe for you.
At Hirschfeld Oncology, we know that clear, honest communication is the foundation of great cancer care. If you have more questions or are looking into advanced treatment options here in Brooklyn, we encourage you to request a consultation with our team. You can learn more on our website at https://honcology.com/blog.





.png)


.png)
.png)




