Starting a new medication like exemestane always comes with a lot of questions, and the first step to feeling in control is to really get how it works. At its heart, this drug is designed to lower the amount of estrogen in your body, which is a key way we fight certain kinds of breast cancer. This one simple fact is the foundation for understanding everything else, including the exemestane side effects you might experience.
Understanding How Exemestane Fights Cancer
To really wrap your head around how exemestane works, it helps to know about a specific enzyme in your body called aromatase. Think of this enzyme as a little factory that’s constantly churning out estrogen.
For breast cancers that are hormone receptor-positive (HR+), estrogen is like fuel. It tells the cancer cells to grow and divide. Exemestane's job is to walk into that factory and shut the whole operation down.
Exemestane belongs to a class of drugs we call aromatase inhibitors. But it’s a special type—a steroidal aromatase inactivator. Instead of just temporarily blocking estrogen, it permanently binds to the aromatase enzyme and disables it. It’s like breaking the key off in the factory’s main lock. This action dramatically drops the amount of estrogen circulating in your system, basically starving the cancer of its fuel source.
Why This Matters for Postmenopausal Women
This "factory shutdown" method is why exemestane is so effective for women who have gone through menopause.
Before menopause, your ovaries are the main source of estrogen. After menopause, the ovaries retire from that job. Instead, most of the body's estrogen is made in other tissues, like fat and the adrenal glands, using that aromatase enzyme.
- Targeted Action: Exemestane goes right after this specific pathway, which is the main source of estrogen after menopause.
- Reduced Recurrence Risk: By cutting off the estrogen supply, it helps ensure that any stray cancer cells left behind can't grow, which significantly lowers the risk of the cancer coming back.
- Adjuvant Therapy: This is why it’s so often used as an “adjuvant” therapy—a treatment given after the main ones like surgery or chemo to keep you cancer-free.
At its core, exemestane creates an internal environment where hormone-sensitive cancer cells simply can't survive. Grasping this helps connect the dots between how the drug works so well and why the side effects—which are mostly related to low estrogen—happen.
This strategy of hormone manipulation is a true cornerstone of treating HR+ breast cancer today. As we go on, you’ll see that the very mechanism that makes exemestane a powerful ally is also directly tied to its side effect profile.
Understanding this connection is the key to managing your health and well-being during treatment. For a deeper look at this approach, you can explore our guide to cancer hormone therapy. Having this knowledge helps you partner with your care team to manage symptoms, maintain your quality of life, and get the absolute best results from your treatment.
Navigating Common Exemestane Side Effects
Starting a new treatment like exemestane means finding a new rhythm for your body, and a big part of that is understanding what to expect. Since this medication works by significantly lowering estrogen, many of the side effects feel a lot like menopause—just sometimes a bit more sudden or intense.
The great news is that most of these side effects are absolutely manageable. Being prepared is half the battle. When you know what might be coming, you can take proactive steps to stay comfortable and protect your quality of life. The goal isn’t just to get through treatment; it’s to live well throughout it.
Hot Flashes and Night Sweats
Hot flashes are probably the most well-known side effect. These are sudden, intense waves of heat that can pop up out of nowhere, usually hitting the face, neck, and chest. They can even be followed by a chill. When they happen at night, we call them night sweats, and they can really mess with your sleep.
These "vasomotor symptoms" are a direct result of your hormone levels changing, which throws off the part of your brain that acts as your body's thermostat. In major clinical trials, over 20% of patients experienced hot flashes. One key study reported that 21.7% of the women taking exemestane had them. At Hirschfeld Oncology, we spend a lot of time helping patients through this, especially those with advanced disease who need treatments they can stick with for the long haul.
This infographic breaks down how exemestane shuts down estrogen production—the very action that causes these side effects.
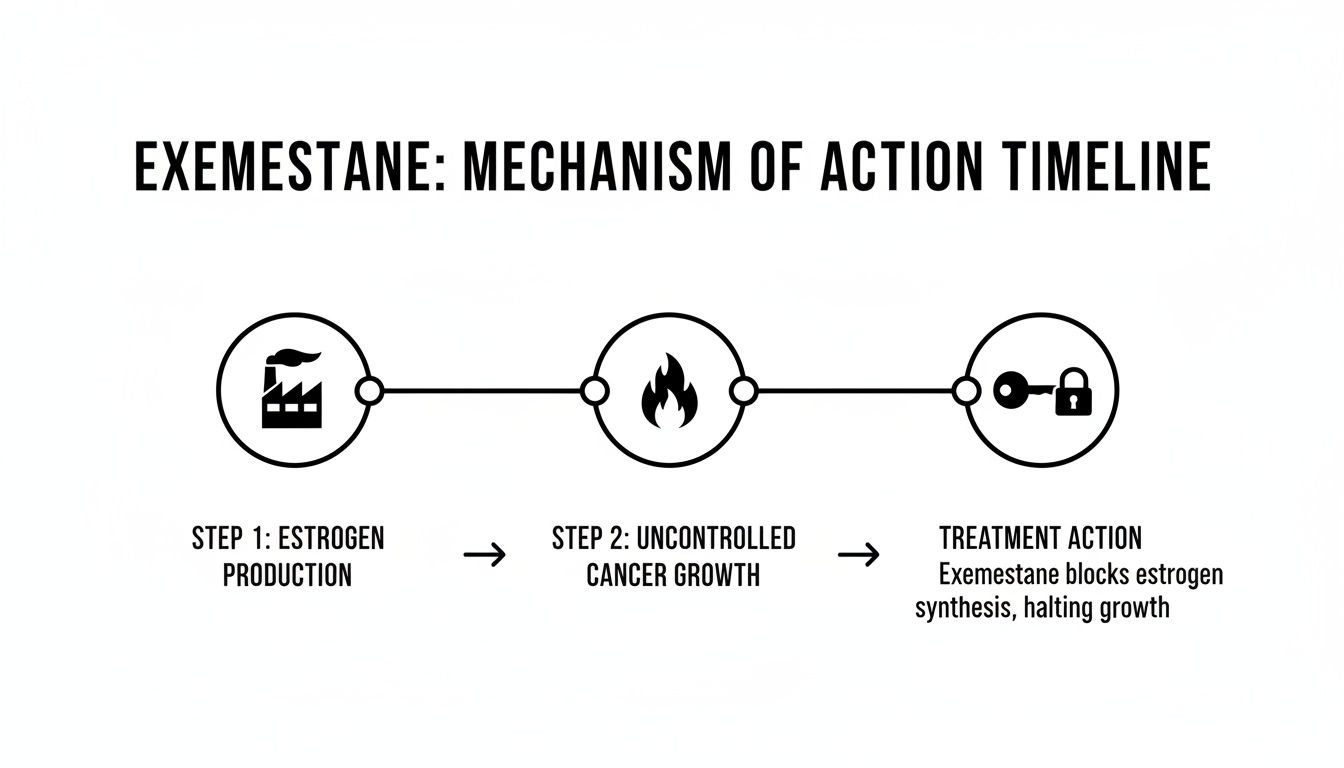
As you can see, by blocking the body’s estrogen factory, the medication effectively starves the cancer cells of their fuel. But this is the same mechanism that triggers those menopausal-type symptoms.
A few simple, practical strategies can make a world of difference:
- Dress in layers: Wear breathable fabrics like cotton that you can easily take off or put back on as your internal temperature fluctuates.
- Stay cool: Keep a fan handy at your desk or by your bed. Sipping cool water all day can also help keep your body temperature stable.
- Identify your triggers: Pay attention to what seems to set off a hot flash. Common culprits include spicy foods, caffeine, stress, or even just a warm room.
Joint Pain and Stiffness
Another very common complaint is arthralgia, which is the clinical term for joint pain and stiffness. Many people feel it most in their hands, wrists, knees, or feet, and it's often worse first thing in the morning. This happens because estrogen helps lubricate our joints and keep inflammation in check. When those levels plummet, things can get a bit creaky and sore.
While it’s definitely frustrating, this pain isn't a sign of arthritis, and it doesn't mean the medication isn’t working. It’s a very common and expected response to having low estrogen.
The best thing you can do for it? Keep moving. I know it sounds counterintuitive when you're feeling stiff, but gentle, consistent movement is key to preventing and easing the pain.
- Try gentle exercise: Things like walking, swimming, or yoga are perfect. They get blood flowing to your joints without putting too much strain on them.
- Stretch it out: Make daily stretching a habit, focusing on the areas that give you the most trouble. It really helps with flexibility and can bring a lot of relief.
- Use heat or cold: Some people swear by a warm bath or shower in the morning to loosen everything up. Others find a cold pack on a specific sore spot works best to calm inflammation.
Fatigue and Mood Changes
Feeling wiped out is another side effect many people on exemestane deal with. This isn't your normal, end-of-a-long-day tiredness; it's a more profound fatigue that a good night's sleep doesn't always solve. It can stem from the hormonal shifts, poor sleep due to night sweats, or the emotional weight of everything you're going through.
On a similar note, these hormonal changes can mess with your mood. You might find yourself feeling more irritable, anxious, or just down. It’s a physiological response, not a personal weakness. Acknowledging that is the first step. For more tips on this, our guide on managing side effects of cancer treatment for a better quality of life has some great information.
To help you keep track, here’s a quick summary of these common side effects and what you can do about them.
A Quick Guide to Managing Common Side Effects
This table breaks down some of the most common issues, when you can expect them, and some practical first steps you can take at home to feel better.
Remember, this is just a starting point. Always talk to your oncology team about what you're experiencing. You never have to just "tough it out." We have so many ways to help manage these symptoms, and we're here to find what works best for you.
Protecting Your Long-Term Health on Exemestane
It’s easy to get caught up in the day-to-day side effects of exemestane, but it’s just as crucial to think about the bigger picture. Because this medication works by dramatically lowering estrogen, it can create ripple effects in other parts of your body over the long haul. This isn't a reason to worry, but it is a call for awareness and some proactive self-care.
Taking this long-term view allows you and your oncology team to work together to protect your overall wellness. Two of the most important areas to keep an eye on are your bone health and your cardiovascular system.

Keeping Your Bones Strong
Estrogen is a key player in keeping your bones dense and strong. It acts like a traffic cop for the natural cycle of bone breakdown and rebuilding. When your estrogen levels drop so significantly, that delicate balance gets thrown off.
Think of your bone density like a bank account. Normally, you make regular deposits (building new bone) that keep pace with your withdrawals (clearing out old bone). Low estrogen is like having fewer deposits coming in, which can slowly drain your account balance over time.
This can lead to a drop in bone mineral density. It might start as osteopenia (mild bone loss) and, if left unchecked, could progress to osteoporosis (more severe bone loss). Osteoporosis makes your bones more fragile and much more likely to fracture.
Proactive monitoring is the cornerstone of protecting your bones during exemestane treatment. Your care team isn't just treating cancer; they are managing your total health, and that includes preserving your bone strength for the years ahead.
To stay ahead of this potential exemestane side effect, your oncologist will almost certainly recommend a few key strategies:
- DEXA Scans: This is a simple, painless X-ray that measures your bone density. You'll likely get a baseline scan before you even start treatment and then follow-up scans periodically to see how things are going.
- Calcium and Vitamin D: These are the essential building blocks for strong bones. Your doctor will recommend specific daily doses to make sure your body has all the raw materials it needs to maintain bone health.
- Weight-Bearing Exercise: Activities that put gentle stress on your bones—walking, jogging, dancing, or lifting light weights—send a powerful signal to your body to build more bone tissue. Even 30 minutes a day can make a real difference.
Protecting Your Heart and Cardiovascular System
Your heart health is another important long-term consideration. Estrogen actually has a protective effect on your cardiovascular system, helping to keep cholesterol levels in check and blood vessels flexible. When estrogen is suppressed, some women might notice a bump in their cholesterol, especially the LDL or "bad" cholesterol.
This doesn't automatically mean you'll develop heart problems, but it does mean it's something to watch closely. Your oncology team will keep tabs on your cholesterol with regular blood tests.
Being mindful of your heart health involves the same common-sense steps that benefit everyone:
- A Heart-Healthy Diet: Try to focus on foods packed with fiber, healthy fats, and antioxidants. Think fruits, vegetables, whole grains, and lean proteins.
- Regular Physical Activity: Aim for consistent aerobic exercise to strengthen your heart muscle and help manage your cholesterol.
- Know Your Numbers: Stay on top of your blood pressure and cholesterol levels. It's a good idea to discuss them with both your oncologist and your primary care provider.
To help manage the hormonal shifts from exemestane, some people look into hormone balance supplements for women for extra support, but it's critical to talk to your doctor before starting anything new. By staying informed and engaged, you can help ensure your entire body stays healthy and strong throughout your treatment journey and for years to come.
Your Proactive Health Monitoring Plan
Taking exemestane isn’t something you do alone—it's a true partnership between you and your oncology team. Think of us as your dedicated support crew for this part of your treatment journey. Our job is to make sure the medication is doing its work while helping you feel as good as possible along the way.
This partnership is built on a proactive monitoring plan. We'll set up a schedule of check-ins and tests designed to keep you safe and catch any potential issues early, before they become real problems. This is about more than just treating cancer; it's about protecting your overall health.
Routine Checkpoints for Your Well-Being
While your specific schedule will be tailored to you, it generally includes a few key elements to track how your body is adjusting to the significant drop in estrogen.
- Regular Blood Tests: These are incredibly useful for keeping tabs on a few different things. We’ll monitor your liver function to make sure it’s processing the medication without any strain. We also keep a close eye on your lipid panel (cholesterol levels), as these can sometimes tick up when estrogen is suppressed.
- Bone Density (DEXA) Scans: As we’ve discussed, keeping your bones strong is a top priority. You’ll almost certainly have a baseline DEXA scan before or just after starting exemestane. Follow-up scans, typically every one to two years, let us track your bone mineral density and step in with support if we see any signs of thinning.
This consistent oversight allows us to be nimble and make informed adjustments to your care plan. It’s the difference between reacting to a problem and preventing one in the first place.
Your feedback is the most important data we collect. How you feel—your energy levels, joint comfort, and overall well-being—guides our decisions just as much as any lab result or scan.
The Critical Importance of Drug Interactions
One of the most vital parts of your safety plan is keeping an open line of communication about everything you take. This means more than just prescription medications. We need to know about over-the-counter drugs, vitamins, and even herbal supplements.
Why is this so critical? Some substances can interfere with how your body absorbs or breaks down exemestane, which could make it less effective. Others might amplify the risk of certain side effects.
For example, anything that could raise your body’s estrogen levels would be working directly against your treatment. This can include certain supplements marketed for menopause relief, which might seem harmless but could undermine your therapy.
Your care team needs the full picture to keep you safe. Before you start anything new, no matter how small or benign it seems, please run it by us first. This one simple step ensures that all the different parts of your health plan are working together, not against each other.
At Hirschfeld Oncology, this collaborative spirit is at the core of how we practice. We believe a well-managed treatment gives equal weight to fighting cancer and preserving your quality of life. Your monitoring plan is how we put that belief into practice, making sure your treatment is as safe and tolerable as it is effective.
A Patient-First Approach to Managing Side Effects
When it comes to your cancer treatment, your experience is the single most important factor. A truly patient-first approach isn't just about fighting the disease; it’s about treating you as a whole person. This means your feedback on how exemestane is affecting you isn't just helpful—it's the most critical piece of information we have.

This is where the idea of shared decision-making becomes real. If you tell us about persistent joint pain or that fatigue is making your days impossible, that report becomes the starting point for our plan. It’s a conversation, not a set of instructions.
Turning Feedback into Action
Your voice actively shapes your treatment path. We're always aiming for that sweet spot: treating the cancer effectively while protecting your quality of life. This requires a flexible, nimble approach that we can adjust based on how you're feeling.
When a side effect becomes a problem, we'll talk through several options together:
- Dose Modification: Sometimes, a small dose reduction can make a world of difference in how you feel, often without compromising the drug's effectiveness. In fact, recent research suggests lower doses of some hormonal therapies can be just as potent with fewer side effects.
- Supportive Medications: We can bring in other medications to help with specific issues. This might mean using non-steroidal anti-inflammatory drugs (NSAIDs) to ease joint pain or other prescriptions to get a handle on hot flashes.
- Integrative Therapies: We often recommend evidence-based complementary treatments. This could look like a referral to a physical therapist to improve joint stiffness or suggesting acupuncture, which has shown real promise for managing treatment-related symptoms.
At Hirschfeld Oncology, we don't see side effect management as an afterthought. It's a core part of effective cancer care. Making sure you feel heard, supported, and in control is essential to getting the best possible outcome.
This personalized approach means you never have to just "tough it out" through a difficult side effect. The goal is always to find a sustainable plan that feels right for you.
The Art of Balancing Efficacy and Tolerability
The conversation about side effects is never one-and-done. What works for one person might not work for another, and what feels manageable today might need a new approach in a few months. This is particularly true for patients on long-term adjuvant therapy, which can last for 5 to 10 years.
This ongoing dialogue is where the "art" of oncology really comes into play. It’s about listening carefully to your experience and using clinical expertise to make thoughtful, tailored adjustments. For instance, if joint pain from exemestane starts getting in the way of your daily life, we'll explore every avenue.
That might mean trying a different aromatase inhibitor, since some people find they tolerate one better than another. It could also mean building a more comprehensive pain management plan. To see how these ideas fit into a larger framework, you can read about our personalized symptom management strategies during cancer treatment.
We also know that managing the emotional and psychological side of cancer treatment is crucial. Exploring practical resources and proactive coping strategies for stress can make a significant difference. Ultimately, our goal is to create a treatment plan you can not only tolerate but thrive on, ensuring you get the full, long-term benefit of your therapy while living the life you want.
Knowing When to Call Your Doctor
One of the most important things we establish with our patients is an open line of communication. When you're on a medication like exemestane, knowing what's normal and what isn't is key. Think of it less as "bothering your doctor" and more as being an active, essential partner in your own care.
It helps to think of this in two categories: things we can discuss at our next regular visit, and things that mean you should pick up the phone right away. Understanding the difference will help you feel more in control and ensure you get the right help at the right time.
Discuss at Your Next Appointment
These are the side effects that, while not emergencies, definitely impact your quality of life. For these, I always recommend keeping a simple symptom journal. Jot down what you're feeling, when it happens, and how intense it is. That log is incredibly valuable when we talk, as it helps us pinpoint the best way to make you feel better.
- Persistent Joint Pain: If the aches and stiffness are starting to wear you down or aren't getting better with the usual at-home tricks.
- Worsening Hot Flashes: When hot flashes or night sweats go from being a nuisance to something that's genuinely disrupting your sleep and your day.
- Ongoing Fatigue or Mood Changes: Let us know if you're feeling an exhaustion that just won't lift, or if your mood has been low or irritable for a while.
- Minor Swelling: You might notice a little new puffiness in your hands, feet, or ankles. As long as it's not severe or painful, it's something we can address at your next visit.
Your personal experience is a vital piece of the puzzle. Reporting even mild but persistent side effects allows your care team to make small adjustments that can lead to big improvements in your well-being.
Call Your Doctor Immediately
Some symptoms, while rare, are red flags for more serious issues. If you experience any of the following, don't wait for your next appointment—call your oncology team's office right away.
- Signs of a Blood Clot: This isn't subtle. Look for sudden pain, swelling, tenderness, or redness in just one leg, usually the calf. If a clot travels to the lungs, it can cause a sudden, sharp chest pain, shortness of breath, and a racing heart. This is a medical emergency.
- Chest Pain or Shortness of Breath: Any new chest pain, pressure, or difficulty breathing that you can't explain needs to be evaluated immediately.
- Signs of a Stroke: These signs come on suddenly. Be alert for numbness or weakness on one side of your body, sudden confusion, trouble speaking or seeing, or the worst headache of your life.
- Severe Depression or Thoughts of Harming Yourself: Your mental health is every bit as important as your physical health. Please reach out right away if you're feeling hopeless or having thoughts of self-harm. We are here to help you.
Common Questions About Taking Exemestane
Starting a long-term medication like exemestane understandably comes with a lot of questions. Let's walk through some of the things patients most often ask, so you can feel more confident and in control of your treatment plan.
How Long Do Exemestane Side Effects Last?
This is probably the most common question we get, and the answer really varies from person to person. For many women, side effects like hot flashes hit hardest in the first few months. Over time, your body starts to adjust to the lower estrogen levels, and those symptoms often begin to fade or at least become much more manageable.
Other side effects, though, like joint pain or stiffness, can sometimes stick around for the entire time you're on the drug. The encouraging news is that for most people, these issues tend to clear up within a few months after treatment ends.
The most important thing to remember is that you don't have to just "tough it out." Keeping an open line of communication with your oncology team is key. We have so many ways to manage these symptoms and make a real difference in your quality of life.
Can I Take Supplements to Help with Side Effects?
It's completely natural to look for ways to feel better, but it's absolutely crucial to run any new supplement by your oncologist first. You can pretty much count on your doctor recommending specific amounts of calcium and vitamin D. This is standard practice to help protect your bones while you're on an aromatase inhibitor.
Where things get tricky is with other supplements, especially herbal products marketed for menopause symptoms. Many of these contain plant-based estrogens (phytoestrogens) which could potentially interfere with your treatment. Others might affect how your body absorbs or breaks down exemestane.
Before starting any new vitamin, mineral, or herbal supplement, please get the green light from your care team. Your safety and the success of your cancer treatment are always priority number one.
Is It Safe to Stop Taking Exemestane?
You should never stop taking exemestane or change your dose without talking to your oncologist. I know the side effects can be incredibly challenging, but stopping the medication on your own can seriously undermine your treatment and raise the risk of the cancer coming back.
Hormone therapy is one of our most powerful tools for preventing recurrence in HR-positive breast cancer. Study after study confirms its long-term protective benefits, and sticking with it is the only way to get that full effect.
If side effects are making your daily life difficult, please tell us. We have options. Your care team can work with you to:
- Adjust the dose
- Switch you to a different aromatase inhibitor
- Prescribe other medications to help with symptoms
- Bring in complementary approaches like physical therapy or acupuncture
The goal is always to find a path forward that keeps your treatment effective while making sure you feel as good as possible. It's a partnership, and finding that balance is central to successful long-term cancer care.
At Hirschfeld Oncology, we see open, honest conversations and proactive symptom management as the foundation of great care. If you're struggling with side effects or just have questions about your treatment, check out our resources or request a consultation. We're here to build a plan that truly works for you. Learn more at https://honcology.com/blog.





.png)


.png)
.png)




