When you first hear the words "stage 4 gallbladder cancer," it's natural to feel lost and overwhelmed. The diagnosis immediately brings up so many questions about what comes next. Put simply, stage 4 means the cancer has metastasized—it has traveled from the gallbladder to other, more distant parts of the body. While this is the most advanced stage, it’s important to see this diagnosis not as an endpoint, but as the starting point for creating a clear, comprehensive plan focused on managing the cancer and protecting your quality of life.
What a Stage 4 Gallbladder Cancer Diagnosis Really Means
When oncologists talk about "staging," they're really just describing the cancer's size and how far it has spread. Think of it like a map that shows where the cancer started and where it has journeyed. For gallbladder cancer, stage 4 tells us the cancer cells have moved beyond the gallbladder itself and the lymph nodes right next to it. They've set up new tumors in distant organs.
The most common places for gallbladder cancer to spread include:
- The liver: Because it's so close, the liver is a very common place for the cancer to travel.
- The lungs: Cancer cells can get into the bloodstream or lymphatic system and make their way to the lungs.
- The peritoneum: This is the thin lining of your abdominal cavity. Cancer cells can sometimes spread across this surface.
- Distant lymph nodes: The cancer can also move to lymph nodes far away from the gallbladder.
Figuring out exactly where the cancer has spread is the first critical step your medical team takes. It’s not about applying a generic label; it’s about creating a precise picture of the situation to determine the most effective ways to manage it.
Why Staging Is So Important
Staging gives doctors a shared, universal language to talk about the extent of the disease. It helps them anticipate how the cancer might behave and decide which treatments are likely to work best. For gallbladder cancer stage 4, the main goal of treatment usually shifts from trying to cure the cancer to controlling its growth, managing symptoms, and making sure you have the best possible quality of life.
This approach is often called palliative or supportive care, but that doesn't mean giving up. It’s about adding a powerful layer of support that works right alongside active treatments like chemotherapy to help you feel stronger, manage symptoms, and live better.
This modern focus puts your physical comfort and emotional well-being at the heart of the treatment plan. Your oncology team will look at more than just the stage; they'll consider your overall health, the specific genetic markers of the tumor, and what matters most to you. This collaborative process ensures the path forward is built around you as a person, moving beyond cold medical terms to create a proactive and supportive care plan from day one.
Making Sense of Survival Rates and Prognosis
Let's be honest—this is one of the hardest conversations. When you look up statistics for stage 4 gallbladder cancer, the numbers can feel like a punch to the gut. It's easy to get lost in the percentages and feel a wave of hopelessness.
But here’s what I tell my patients: statistics are a rearview mirror, not a crystal ball. They show us where we've been, reflecting the outcomes of thousands of people diagnosed years ago. They are not a prediction of your personal journey, especially with the pace of medical progress today.
Putting Statistics into Proper Context
You’ll often come across the term "5-year relative survival rate." This is simply a statistical tool that compares a large group of people with the same cancer stage to the general population. It helps researchers understand the overall impact of a diagnosis on a broad scale.
This table provides a snapshot of how survival rates for gallbladder cancer change as the disease progresses, based on data from the SEER database.
Gallbladder Cancer Survival Rates by Stage
Seeing that 3-4% figure for distant (stage 4) cancer is understandably frightening. It means that, on average, three to four people out of 100 diagnosed between 2015 and 2021 were alive five years later compared to people without the cancer.
It is absolutely crucial to see this number for what it is: a historical baseline. It doesn't capture the impact of newer, more precise treatments that have become available since then. Your individual prognosis is so much more than just one number.
The diagram below helps visualize what "distant" spread means—the cancer has traveled from its starting point in the gallbladder to other organs.
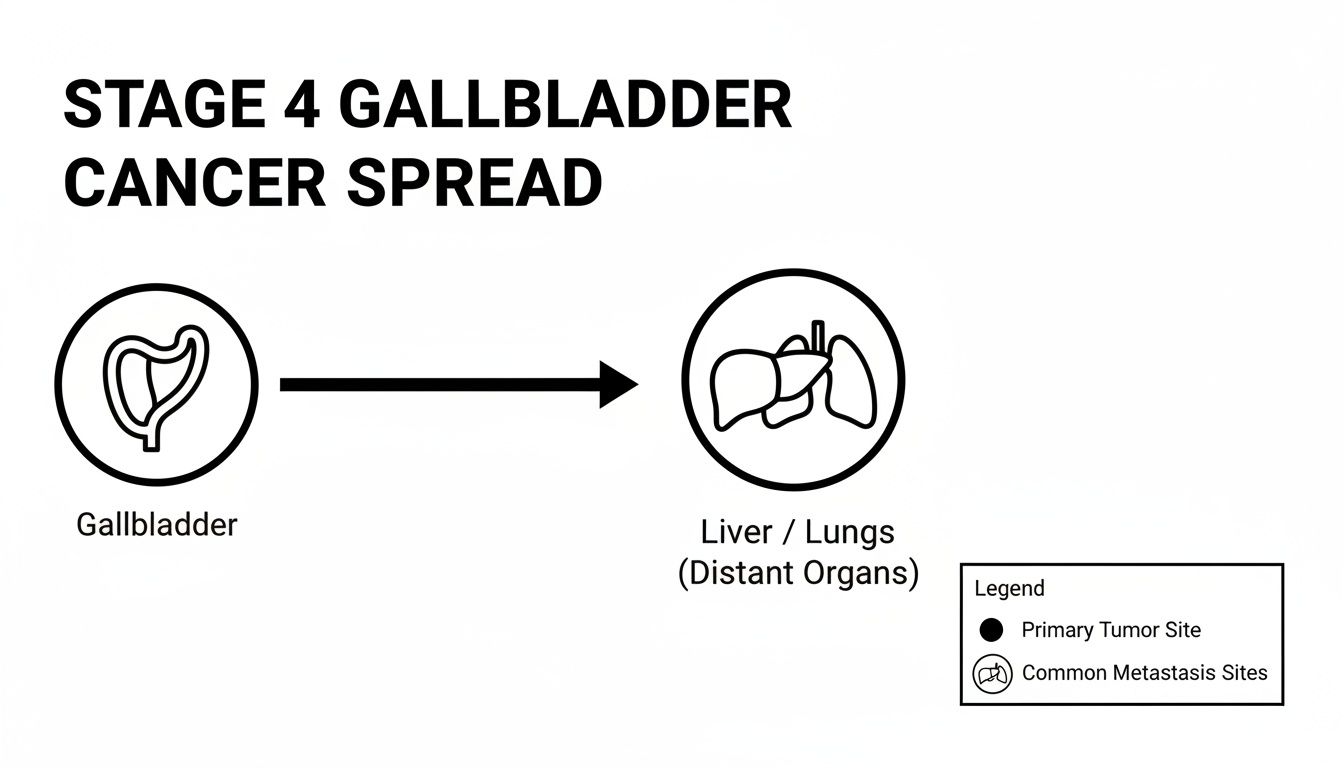
This is why treatment at stage 4 needs to be systemic—it has to address cancer cells throughout the body, not just in one spot.
Factors That Shape Your Individual Prognosis
Your story is completely unique. Your oncology team will look far beyond general statistics to build a plan that makes sense for you. They’ll consider several key factors that truly shape your outlook.
- Tumor Biology: Not all gallbladder cancers are built the same. We can now test the tumor for specific genetic mutations or protein markers. Finding one can be a game-changer, opening the door to targeted therapies or immunotherapies designed to attack that exact weakness.
- Your Overall Health: How strong you are heading into treatment matters. Your age, fitness level, and ability to handle therapies all play a huge role in what options are on the table and how effective they can be.
- Response to Treatment: This is a big one. How the cancer reacts to the first round of therapy tells us a lot. A good response can dramatically improve your prognosis and unlock new treatment possibilities down the road.
Remember, statistics describe what has happened to large groups in the past. They do not—and cannot—determine your future. Use them as a starting point for a conversation with your care team, not as a final verdict.
Your prognosis isn't a fixed point; it's a dynamic picture that can change. As treatments get better, so do outcomes. This journey is also about more than just fighting the cancer. It involves having open conversations about supportive care, managing symptoms, and understanding what families need to know about end-of-life services to ensure comfort and dignity are always at the center of your care plan. The focus is on living your best possible life, for as long as possible.
Your Guide to Advanced Gallbladder Cancer Treatments

When you're facing a stage 4 gallbladder cancer diagnosis, having a clear understanding of your treatment options is crucial. At this advanced stage, the main goal shifts from a cure to controlling the cancer's spread, easing symptoms, and making sure you have the best possible quality of life. Think of your treatment plan not as a single solution, but as a carefully selected toolkit your oncology team will use for your specific situation.
Surgery to remove the cancer is rarely an option once it has spread. Instead, the focus turns to systemic therapies—treatments that travel through the bloodstream to reach and fight cancer cells wherever they are in the body. These therapies are the cornerstone of care, working to slow the disease down and help you feel better.
Chemotherapy: The Foundational Treatment
For most people with advanced gallbladder cancer, chemotherapy is the first line of defense. These are powerful drugs that work by targeting and killing cells that divide quickly, a key characteristic of cancer. You can think of chemotherapy as a systemic patrol sent throughout your body to find and shut down these rapidly growing cells.
Because it works everywhere, chemotherapy can address cancer that has spread to distant parts of the body. The most common combination used for years has been gemcitabine and cisplatin, a regimen that became the standard of care for advanced biliary tract cancers like this one.
In this context, chemotherapy aims to:
- Slow Cancer Growth: To keep tumors from getting bigger or spreading to new areas.
- Shrink Tumors: Reducing the size of tumors can relieve pressure on nearby organs and lessen symptoms.
- Manage Symptoms: By getting the cancer under control, chemotherapy can help reduce pain, fatigue, and other issues.
Of course, chemo can't always tell the difference between cancer cells and other fast-growing healthy cells, like those in your hair, mouth, or digestive tract. This is why side effects like hair loss, nausea, and low energy happen. The good news is that modern cancer care is just as focused on managing these side effects with supportive medications and smarter dosing strategies, making treatment much more tolerable than it once was.
Targeted Therapy: A More Precise Approach
One of the biggest shifts in cancer care is the move toward more personalized treatments, and targeted therapy is a perfect example. Unlike chemotherapy's broad approach, targeted drugs are designed to find and attack specific features—or "targets"—on the cancer cells themselves.
Here's an analogy: if chemotherapy is a general patrol, targeted therapy is like having a special key that only fits the lock on a cancer cell, leaving most healthy cells unharmed. This precision often leads to a different and sometimes milder set of side effects.
To see if targeted therapy is right for you, your oncologist will need to run molecular tests on a sample of your tumor. This analysis scans the cancer's DNA for specific genetic mutations or proteins that are fueling its growth. If one of these "actionable" targets is found, there may be a drug designed to block it.
Finding an actionable mutation in your tumor's DNA can be a significant turning point. It opens the door to treatments designed specifically for your cancer's unique biological makeup, moving beyond a one-size-fits-all plan.
For gallbladder cancer, some of the specific targets your team might look for include:
- FGFR2 fusions: A genetic rearrangement that can be blocked by drugs known as FGFR inhibitors.
- IDH1 mutations: Another type of genetic error that can be shut down by specific IDH1-inhibiting drugs.
- HER2 amplification: While famous for its role in breast cancer, about 5-15% of gallbladder cancers also have this marker, opening the door to HER2-targeted treatments.
As researchers learn more, the list of potential targets keeps growing. You can dive deeper into this topic by reading our guide on what is molecular testing for cancer and how it shapes personalized treatment.
Immunotherapy: Activating Your Body's Defenses
Immunotherapy is another exciting frontier in cancer treatment. Rather than attacking the cancer cells directly, these drugs empower your own immune system to do the job it was designed to do—recognize and destroy invaders.
Cancer cells can be sneaky. They often develop tricks to hide from the immune system, almost like they're wearing a disguise. Immunotherapy drugs, especially a type called immune checkpoint inhibitors, work by ripping off that disguise. This "unmasks" the cancer cells, allowing your body’s T-cells to finally see them as a threat and launch an attack.
For immunotherapy to have a good chance of working, a tumor often needs certain biological markers. For gallbladder cancer, two of the most important are:
- PD-L1 Expression: This is a protein cancer cells use to hide. If a tumor has high levels of PD-L1, checkpoint inhibitors can be very effective.
- Mismatch Repair Deficiency (dMMR) or High Microsatellite Instability (MSI-H): These are signs that the tumor's DNA repair system is broken. This makes the cancer cells look very abnormal and "foreign" to the immune system, making them a prime target for an immunotherapy-led attack.
Only a small fraction of gallbladder cancers have these markers. But for patients who do, immunotherapy can sometimes produce remarkable and long-lasting responses. It's a powerful example of how personalized medicine is creating new hope. Your care team will test your tumor for these markers to see if this is a potential path for you.
Why Palliative Care Is an Essential Part of Your Treatment

When people hear the term "palliative care," they often jump to the wrong conclusion, thinking it’s the same as end-of-life or hospice care. I want to be very clear: that's one of the biggest myths in oncology.
Palliative care is actually an extra layer of support that should start the moment you're diagnosed with gallbladder cancer stage 4. Think of it as your dedicated quality-of-life team. While your oncologist is focused on treating the cancer itself, the palliative team is focused entirely on you—managing your symptoms, reducing stress, and helping you feel as well as possible through it all.
This specialized care runs right alongside your primary treatments. Its entire purpose is to improve your well-being so you can handle cancer therapies better and live as fully as you can, every single day.
What Palliative Care Truly Addresses
A serious diagnosis doesn't just affect you physically; it touches every corner of your life. Palliative care gets that. The team—often a mix of doctors, nurses, social workers, and dietitians—is built to address the whole picture.
Their support is customized to exactly what you're going through, and it can include things like:
- Pain Management: Finding the most effective ways to control pain from the cancer or its treatments.
- Symptom Control: Taking aggressive action to relieve common problems like nausea, crushing fatigue, loss of appetite, or shortness of breath.
- Emotional and Spiritual Support: Connecting you and your family with resources to cope with the very real anxiety and stress that a cancer diagnosis brings.
- Nutritional Guidance: Creating a plan with a dietitian to fight weight loss and keep your strength and energy up.
By tackling these problems directly, palliative care aims to prevent and ease suffering from day one. It’s all about providing comfort, support, and giving you back a sense of control.
Many people mistakenly believe they have to choose between cancer treatment and palliative care. The truth is, they work best together. Starting palliative care early has been proven to improve not only quality of life but also how satisfied patients are with their treatment.
Here’s a practical example: if chemotherapy makes you so nauseous that you can't eat, you'll lose the strength needed to continue treatment. A palliative specialist can step in with better anti-nausea medications and dietary strategies, making it possible for you to stick with your life-extending therapy more comfortably.
How Palliative Care Strengthens Your Overall Treatment
Bringing palliative care into your plan from the beginning can genuinely change your experience with stage 4 gallbladder cancer for the better. When your symptoms are under control, you are far more likely to stay on your prescribed treatment schedule.
This proactive support helps build the physical and emotional strength you'll need for the road ahead. We dive deeper into these distinctions in our guide on palliative care vs. hospice care, which clears up a lot of common confusion.
Ultimately, palliative care ensures your medical plan reflects what truly matters to you. It creates space for important conversations about your goals and gives you a dedicated team to support you and your loved ones. It’s a vital, empowering part of modern cancer care.
When the usual treatments for stage 4 gallbladder cancer aren't working as well as hoped, it's completely natural to start looking for other possibilities. This is where medical research can open up new doors, offering options like clinical trials or highly specialized surgeries.
Exploring these paths isn't for every patient, but for some, it’s a way to access the absolute newest developments in cancer care. It's all about having an open conversation with your doctors to weigh the hope of a new approach against the real-world risks and benefits.
What Are Clinical Trials, Really?
Clinical trials are simply research studies designed to test new treatments or find better ways to use the ones we already have. They are the engine that drives all medical progress. Every single treatment we consider "standard" today, from specific chemotherapy drugs to powerful immunotherapies, was once only available to patients in a clinical trial.
Joining a trial can give you access to therapies that aren't available to the general public yet. These could be brand-new targeted drugs, innovative immunotherapy combinations, or different schedules for delivering chemotherapy.
For advanced cancer, clinical trials generally aim to:
- Test New Treatments: Find out if a new therapy is safe and if it works better than the current standard of care.
- Improve Quality of Life: Many trials are focused on finding better ways to manage symptoms and reduce the side effects of treatment.
- Push Medicine Forward: Your participation adds to the collective knowledge that will help countless patients in the future.
Think of it this way: your oncology team can act as a matchmaker, connecting you with trials that fit your cancer's unique genetic profile and your overall health. You get to be on the front lines of cancer research, potentially benefiting from a new discovery while helping everyone who comes after you.
Because gallbladder and bile duct cancers are closely related, you might also find our guide to bile duct cancer clinical trials useful. There’s often significant overlap in the studies available for both.
Is Surgery Ever an Option in Advanced Cases?
In most cases, surgery isn't the primary treatment for stage 4 gallbladder cancer simply because the cancer has already traveled to other parts of the body. The main strategy shifts to systemic treatments—like chemotherapy or targeted therapy—that can fight cancer cells wherever they are.
However, in very specific and uncommon circumstances, a surgeon might consider an aggressive operation for a small, select group of patients.
This isn't a surgery meant to cure the cancer. The goal is what we call cytoreduction, which means removing as much of the visible tumor as possible. The thinking behind this is that by "debulking" the cancer, other treatments like chemotherapy might have a better shot at being effective. This is a major, high-risk procedure reserved for patients who are otherwise in very good health and whose cancer has spread in a limited way that makes an operation technically possible.
Past studies on this aggressive approach show that while the risks are serious, it can lead to longer survival for a tiny fraction of patients. One analysis of 93 patients who had surgery for stage 4 disease reported an operative mortality rate of 5.4%. For the patients with stage IVA disease, the 5-year survival was 42.8%—a huge difference from the 4.9% survival seen in the stage IVB group. These numbers really drive home how crucial it is to select the right patients for such a procedure. You can read more about these findings on gallbladder cancer surgery.
Ultimately, the decision to pursue these kinds of advanced options is deeply personal. It requires in-depth conversations with a specialized medical team to carefully weigh the potential for a longer life against the very real risks and the impact on your day-to-day quality of life.
How to Assemble Your Expert Cancer Care Team

Getting a diagnosis of gallbladder cancer stage 4 is overwhelming, but one of the first and most powerful steps you can take is to find the right medical team. This is more than just finding a doctor. It's about building a true partnership with a group of experts who listen, understand your priorities, and have hands-on experience with rare, complex cancers.
Think of this team as your personal brain trust. You want people with different skills—medical oncology, palliative care, nutrition—all collaborating for your benefit. For a rare disease like gallbladder cancer, getting a second opinion isn't just a good idea; it's practically a necessity. It provides peace of mind that the diagnosis is correct and that every possible treatment path has been explored.
Navigating care also means dealing with logistics. Taking the time to understand how to choose the right health insurance plan can make a world of difference in ensuring you have access to the specialists and facilities you need.
Finding a Specialist Who Understands Your Cancer
While a general oncologist is an incredible resource, a specialist in biliary tract cancers—like our own Dr. Azriel Hirschfeld—brings a deeper, more focused expertise. This matters. Gallbladder cancer has a unique biological fingerprint and often responds differently to treatments than more common cancers.
At Hirschfeld Oncology, this specialized, patient-first philosophy is the core of everything we do. We know that your goals aren't just about the cancer itself. They're about staying strong, keeping symptoms at bay, and living your life as fully as possible.
Our focus is on creating personalized, low-toxicity treatment plans that fit your life. We look beyond standard protocols to find a mix of therapies that can be tough on cancer but gentle on you.
Our Approach to Your Care
We believe the best decisions are made together, with you as an empowered, central member of the team. Our process is built on this partnership:
- A Deep Dive into Your Case: We start by thoroughly reviewing your entire medical history, every scan, and all your molecular testing results.
- Exploring All Options: We’ll talk through every potential route—from targeted therapies and immunotherapy to promising clinical trials.
- Creating a Tailored Plan: Together, we will build a care plan that aligns with your personal goals and what matters most to you.
Your journey is yours alone, and your care plan should reflect that. If you're looking for a team that marries deep experience with a genuinely compassionate approach, we invite you to schedule a consultation. Let's explore how we can create a plan that truly fits you.
Answering Your Questions About Stage 4 Gallbladder Cancer
When you hear a diagnosis like "stage 4," it's completely normal for your mind to race with questions. This is a difficult time, and you deserve clear, straightforward answers.
Let's walk through some of the most common concerns that come up for patients and their families. Our aim is to give you the information you need to feel more grounded and prepared for conversations with your doctors and the people you love.
What Are the Most Common Symptoms?
By stage 4, the cancer has spread, so the symptoms often become more noticeable. Dealing with these symptoms is a huge part of your care—it's not just about treating the cancer, but about helping you feel as well as possible day-to-day.
Many people with advanced gallbladder cancer experience:
- A persistent ache or pain in the upper right part of the belly.
- Losing a lot of weight without trying.
- Jaundice, which is a yellowing of the skin and eyes caused by a liver backup.
- Nausea and vomiting that can make it hard to eat and keep your energy up.
- Profound fatigue, a deep exhaustion that rest doesn't seem to fix.
It's so important to bring these issues up with your medical team. A palliative care specialist can be your best ally here; their entire focus is on managing symptoms to protect your quality of life through treatment.
Can Diet and Lifestyle Changes Make a Difference?
This is a question we hear a lot. While no diet can cure stage 4 cancer, what you eat and how you move absolutely play a vital role in supporting your body through this fight. Good nutrition can help you keep your strength up, support your immune system, and tolerate treatments better.
I always recommend connecting with an oncology dietitian. They can tailor a plan specifically for you, helping you navigate side effects like nausea or poor appetite to make sure you're getting the right fuel. In the same way, gentle exercise—if your doctor gives the okay—can be a powerful tool against fatigue and for boosting your spirits.
Think of nutrition and gentle movement not as treatments for the cancer, but as powerful tools to support your body's resilience throughout your treatment journey.
How Do I Talk to My Family About My Prognosis?
There's no easy way to have these conversations. They are deeply personal and often heartbreaking. The most important thing to remember is that you are in control. You decide who to tell, when to tell them, and how much you want to share.
Some people find it helps to have a professional, like a hospital social worker or a therapist, there to help guide the discussion. It's okay to be scared, and it's more than okay to tell your family exactly what you need from them. Leaning on honesty and love is often the best way through it.
At Hirschfeld Oncology, we know that getting through a complex diagnosis takes a team that combines deep expertise with genuine compassion. If you’re looking into treatment options for advanced cancer, we invite you to see our patient-focused approach. You can learn more about how we help at our informational blog.





.png)


.png)
.png)




