At its heart, gemcitabine is a master of disguise. Think of it as a cellular saboteur. It’s designed to look just like a natural building block of DNA, which tricks cancer cells into welcoming it inside. But once it's in, this imposter brings the entire cellular assembly line to a grinding halt, stopping tumor growth in its tracks.
How Gemcitabine Stops Cancer Cell Growth
To really get what gemcitabine does, picture a tumor as a rogue factory working overtime, churning out copies of itself nonstop. For this relentless production, it needs a constant supply of raw materials—specifically, the nucleosides that make up DNA. Gemcitabine is what we call a nucleoside analog; it’s essentially a counterfeit version of one of those crucial building blocks.
When we administer gemcitabine, it so closely mimics the real thing that hungry, fast-dividing cancer cells eagerly pull it in. They can't tell the difference. The cell then tries to slot this fake piece into a new strand of DNA, and that’s precisely when the sabotage begins.
The Trojan Horse Strategy
Gemcitabine’s power lies in this deception. It's delivered as a "prodrug," which means it's inactive and harmless on its own. It’s only once it gets inside the cancer cell and is processed by the cell's own machinery that it transforms into a highly potent weapon.
Once activated, gemcitabine launches a brilliant two-pronged attack to shut down cell division. This dual-action mechanism is why it has become such a cornerstone therapy for so many different cancers.
Here’s how the activated drug works:
- It slams the brakes on DNA replication. The activated molecule gets inserted into a new, growing DNA chain. Once it's in, it causes an irreversible error that stops the copying process cold. This is a unique effect called "masked chain termination."
- It cuts off the supply of raw materials. Gemcitabine also inhibits a critical enzyme called ribonucleotide reductase. This enzyme’s job is to produce the very DNA building blocks the cancer cell needs. By blocking it, gemcitabine creates a supply shortage, further crippling the cell’s ability to multiply.
By both corrupting the assembly line and choking off the supply chain, gemcitabine creates a powerful feedback loop. Each action reinforces the other, making its anti-cancer effects much stronger and longer-lasting. This is often called "self-potentiation."
Grasping this is fundamental for both clinicians and patients. It explains not just how gemcitabine works, but why it remains such a vital tool, particularly in managing aggressive diseases like advanced pancreatic cancer. To see how this plays out in practice, you can learn more about advanced pancreatic cancer treatment options and the ways we tailor these therapies for our patients.
In the next sections, we'll dive even deeper into the molecular details—from how the cell activates the drug to the ways we combine it with other therapies to achieve even better results.
How Gemcitabine Gets Activated Inside a Cancer Cell
Gemcitabine doesn't start its work right out of the IV bag. When we administer it, it's actually an inactive molecule—a prodrug—that can't do a thing to cancer cells on its own. Its transformation from a harmless bystander into a potent weapon only begins once it gets inside the cancer cell itself.
Getting in isn't easy. Gemcitabine needs a special escort across the cell membrane. Cancer cells, being obsessed with growing and dividing, are covered in special doorways called nucleoside transporters. These transporters, especially one called hENT1 (human equilibrative nucleoside transporter-1), are designed to pull in the natural building blocks of DNA. They mistake gemcitabine for one of these essential building blocks and actively welcome it inside.
Once it’s past the gates, the real magic happens. The inactive gemcitabine has to be converted into its active, cancer-fighting forms. This biochemical process is called phosphorylation, which is just a fancy way of saying enzymes start sticking phosphate groups onto the drug molecule. Think of it like arming a missile; the raw drug is the warhead, but it needs the phosphate groups to be armed and ready to launch.
Deoxycytidine Kinase: The Master Switch
The first and most critical step in this arming sequence is handled by an enzyme called deoxycytidine kinase (dCK). This enzyme is the master switch for gemcitabine's activity. It attaches the first phosphate group, converting gemcitabine into gemcitabine monophosphate (dFdCMP).
If a cancer cell doesn't have enough dCK, the whole process grinds to a halt right here. The drug gets into the cell but just sits there, completely harmless. This first step is the rate-limiting part of the entire process, meaning the speed and efficiency of dCK determines how much active drug is ultimately produced.
After dCK does its job, other enzymes take over, adding more phosphate groups to create the two fully armed, active forms of the drug:
- Gemcitabine diphosphate (dFdCDP)
- Gemcitabine triphosphate (dFdCTP)
These two molecules are the real killers. They’re now ready to wreak havoc on the cancer cell's DNA replication machinery. This whole pathway is a brilliant example of hijacking a cancer cell’s internal machinery and turning it against itself.
This activation process isn't just a textbook detail—it has a huge impact on whether the treatment will work. The amount of hENT1 transporters on the cell's surface and the level of dCK enzyme inside can literally make or break a patient's response.
A tumor that's rich in hENT1 and dCK will be great at pulling in and activating gemcitabine, which usually leads to a much better outcome. On the flip side, low levels of either one are a major cause of gemcitabine resistance. The drug simply can't get in or can't get armed.
The Cell's Counter-Attack
But the cancer cell isn't completely defenseless. It has its own counter-measure: an enzyme called cytidine deaminase (CDA). CDA's job is to find gemcitabine and immediately neutralize it. It breaks the drug down into an inactive compound called difluorodeoxyuridine (dFdU), which is then promptly kicked out of the cell.
This enzyme is incredibly efficient. Some studies show that CDA can neutralize as much as 90% of the gemcitabine that makes it into the cell.
So, the drug's effectiveness often boils down to a race inside the cell: the activating enzyme (dCK) versus the deactivating enzyme (CDA). A high ratio of dCK to CDA activity is what we hope for, as it means more drug gets armed than disarmed. This delicate balance is precisely why we need to understand the full mechanism—it helps us figure out why some tumors resist treatment and how we might overcome that resistance.
Now that we have our fully armed drug molecules, let's look at exactly how they sabotage the cancer cell.
Gemcitabine's Two-Pronged Molecular Attack
Once a cancer cell has been tricked into activating gemcitabine, the drug unleashes its two potent forms—dFdCDP and dFdCTP—to carry out a brilliant and devastating molecular mission. The way gemcitabine works isn't a single, blunt-force strike; it's a coordinated, two-pronged attack that simultaneously sabotages DNA production and cripples the cell's raw material supply chain. This dual strategy is what makes it so uniquely effective.
This diagram illustrates the journey from an inactive drug to its armed, active forms inside the cancer cell.
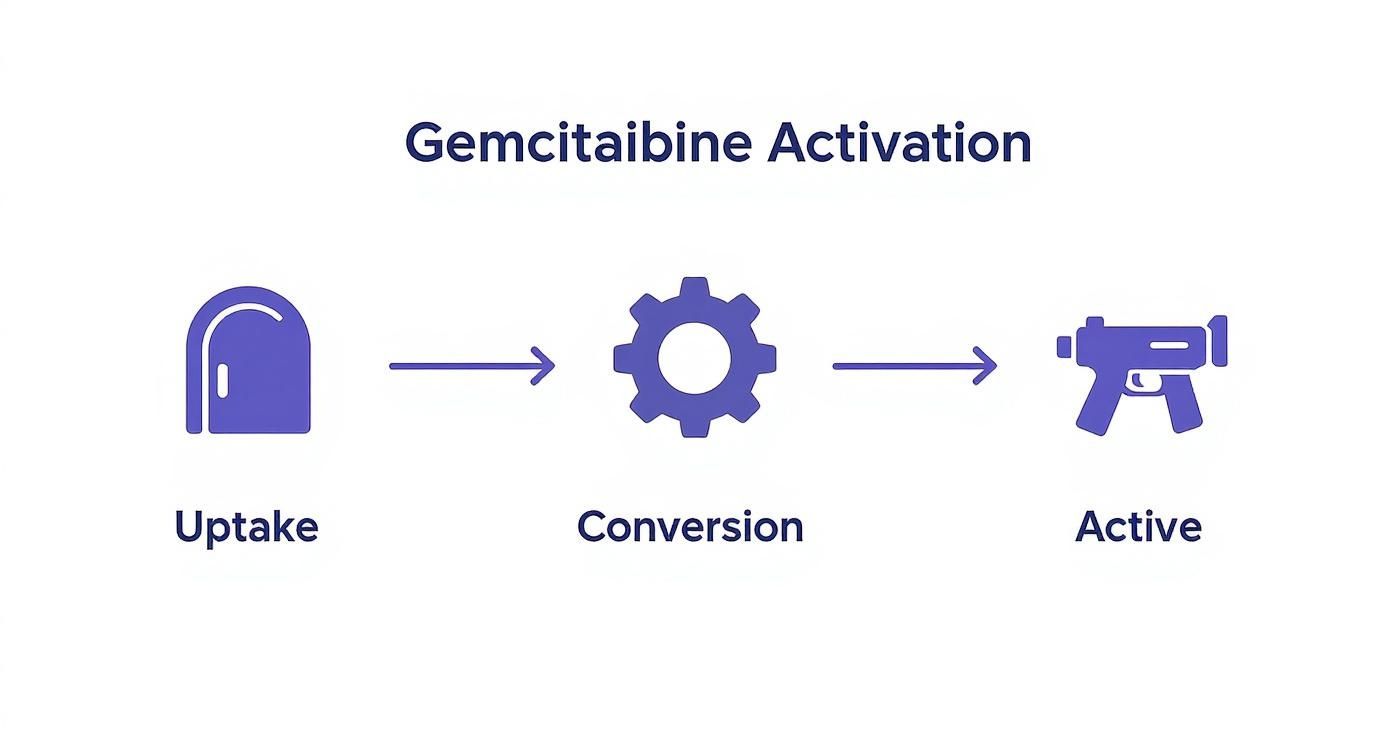
As you can see, the drug must first be taken up by the cell, then converted by internal enzymes before it can become the active weapon that attacks the cancer.
The First Attack: Halting DNA Production
The main assault is led by dFdCTP, the triphosphate version of the drug. Its structure is a masterful imitation of deoxycytidine triphosphate, one of the four essential building blocks of DNA. As a cancer cell frantically tries to copy its genetic code before dividing, an enzyme called DNA polymerase is busy assembling the new DNA strand, piece by piece.
DNA polymerase, completely fooled by the disguise, grabs the fake dFdCTP molecule and inserts it into the growing DNA chain. This is the critical moment of sabotage. The insertion of this faulty part triggers a unique and devastating outcome known as masked chain termination.
Here’s how this brilliant deception unfolds:
- Incorporation: The fake building block (dFdCTP) is added to the DNA strand.
- The Masking Step: The polymerase is then tricked into adding just one more correct, natural building block right after the fake one.
- Irreversible Halt: After adding that single extra piece, the polymerase can go no further. The production line grinds to a complete and permanent stop.
This "masking" is the key. By hiding the faulty piece under one more correct one, gemcitabine effectively prevents the cell's DNA repair crews from finding and fixing the error. The damage becomes permanent, leaving the cell with a broken, incomplete set of instructions that makes it impossible to divide.
The Second Attack: Choking the Supply Chain
While the first attack directly sabotages the assembly line, the second attack, led by the diphosphate form (dFdCDP), targets the factory's supply chain. This molecule goes after a different, but equally vital, enzyme called ribonucleotide reductase (RNR).
The job of RNR is to produce the entire pool of deoxynucleotides—the raw materials needed for DNA synthesis. It's the only source for these building blocks in the cell. By powerfully inhibiting RNR, dFdCDP effectively shuts down the entire supply chain.
This creates a critical shortage of the natural building blocks required for DNA replication, which has a profound effect on the first mechanism of action. It creates a powerful, self-reinforcing feedback loop.
This self-potentiating cycle is the secret to gemcitabine’s power. By starving the cell of its natural DNA building blocks, the drug makes it even more likely that the DNA polymerase will mistakenly grab the fake gemcitabine molecule. One attack amplifies the other, leading to a much more potent anti-cancer effect.
The two active metabolites of gemcitabine, dFdCTP and dFdCDP, work in tandem to disrupt cancer cell division. The following table breaks down their distinct but complementary roles.
Gemcitabine's Two Primary Mechanisms of Action
This elegant dual-action strategy ensures a comprehensive shutdown of the cancer cell's replication machinery, ultimately leading to cell death and helping to control tumor growth.
This multi-target approach has proven remarkably effective in clinical settings, particularly for pancreatic cancer. Gemcitabine's mechanism, centered on inhibiting DNA synthesis through this self-potentiating process, has led to significant survival benefits. In landmark clinical trials, patients receiving gemcitabine monotherapy achieved a median survival of 5.7 months with an impressive 18% one-year survival rate. This substantially outperformed the standard fluorouracil regimen, which produced only a 4.4-month median survival and a 2% one-year survival rate. You can discover more insights about this gemcitabine research on massivebio.com.
How Gemcitabine Works with Other Cancer Therapies
While gemcitabine is a powerful drug on its own, its true clinical strength often shines when it’s part of a team. In modern oncology, we’ve learned that the most effective strategies rarely involve a single “magic bullet.” Instead, we design a multi-pronged attack that cancer cells simply can't withstand. Gemcitabine happens to be a fantastic team player, creating powerful synergy with other therapies to deliver a much harder hit.
I often think of a tumor as a fortress. Gemcitabine is excellent at disrupting the fortress’s internal supply lines and sabotaging its core operations—in this case, DNA synthesis. But that fortress might have other defenses, like thick walls or the ability to rapidly repair any damage.
This is where combination therapy comes in. By pairing gemcitabine with other drugs that attack these different vulnerabilities, we create a much more comprehensive and devastating treatment plan. It's now the standard of care for many cancers, including pancreatic, biliary tract, and non-small cell lung cancer, because it hits the cancer from multiple directions at once. This boosts the odds of killing the cancer cells while also making it harder for them to develop resistance.
Creating Synergy with Other Chemotherapies
One of the most successful pairings is gemcitabine with platinum-based drugs like cisplatin or carboplatin. Platinum agents work by creating cross-links in the DNA, essentially tying the strands together so they can't be pulled apart for replication. This mechanism complements gemcitabine's action perfectly.
Here’s how they work in tandem:
- Gemcitabine weakens the defense: By hamstringing DNA repair, gemcitabine makes it much harder for cancer cells to fix the damage caused by the platinum drug.
- Cisplatin creates the damage: It’s the agent that actually delivers the blow, creating the DNA cross-links that push the cell toward self-destruction.
Another key combination involves pairing gemcitabine with taxanes, such as paclitaxel or its albumin-bound cousin, nab-paclitaxel (Abraxane). Taxanes work on a completely different part of the cell—the microtubules, which form the cell’s internal skeleton. They lock this scaffolding in place, which paralyzes the cell and prevents it from physically dividing into two new daughter cells.
So, while gemcitabine is sabotaging DNA production, the taxane is simultaneously preventing the cell from completing the physical act of division. They disrupt two distinct, yet equally critical, stages of cell replication.
By combining therapies with distinct mechanisms, oncologists can attack a tumor's growth, division, and repair processes simultaneously. This synergistic effect often leads to better tumor response and improved survival outcomes compared to using either drug alone.
Evidence from Landmark Clinical Trials
This isn’t just theory; it’s backed by years of solid clinical evidence. The pivotal phase III MPACT trial, for example, was a game-changer for pancreatic cancer. It showed that combining gemcitabine with nab-paclitaxel pushed the median overall survival to 8.5 months, a significant improvement over the 6.7 months seen with gemcitabine alone.
Of course, other regimens like FOLFIRINOX have also shown impressive results, with a higher objective response rate (31.6% vs. 9.4% for gemcitabine), but it often comes with a higher toxicity price tag. For a deeper dive into these numbers, you can read the full research on pancreatic cancer treatment trials.
Gemcitabine and Radiation Therapy
The synergy doesn't stop with other chemotherapies. Gemcitabine is also what we call a potent radiosensitizer, which is a clinical way of saying it makes cancer cells far more vulnerable to radiation.
It accomplishes this by depleting the cell’s pool of DNA building blocks (those dNTPs), which makes it incredibly difficult for the cell to repair the DNA damage inflicted by the radiation beams. This one-two punch of using chemo and radiation together is a cornerstone strategy for treating localized tumors that can't be removed surgically.
By weakening the cancer cells with gemcitabine first, the radiation can be significantly more effective at destroying the tumor. It’s a perfect example of gemcitabine’s versatility and why it remains a central player in multi-modal cancer care.
Managing Gemcitabine Side Effects and Resistance
While the gemcitabine mechanism of action is a powerful weapon against cancer, its effectiveness comes with real-world challenges. The very strategy that makes it so potent—sabotaging the DNA of rapidly dividing cells—inevitably affects some of our healthy cells, too. This collateral damage is the direct cause of its most common side effects and the reason some cancers eventually learn to outsmart it.
Understanding these hurdles is a crucial part of the treatment journey. When we connect the side effects back to the drug's core function and explore why resistance develops, we can better anticipate, manage, and overcome them. This knowledge empowers both patients and clinicians to navigate therapy with more confidence and control.
Connecting Side Effects to the Mechanism
The side effects of gemcitabine aren't random; they’re a direct consequence of its primary mission. The drug is designed to hunt down cells that are constantly multiplying—the defining characteristic of cancer. The problem is, several types of healthy cells in our bodies also divide at a breakneck pace.
Once gemcitabine enters the bloodstream, it can't tell the difference between a malignant cell and a healthy, hard-working one. It goes after both.
This non-selective action leads to some very common and predictable side effects:
- Myelosuppression: This is the big one—the most significant dose-limiting side effect. Think of your bone marrow as a bustling factory for blood cells. Since it's constantly churning out new red cells, white cells, and platelets, it becomes a prime target for gemcitabine, often leading to low blood counts.
- Fatigue: The causes here are complex, but a big part of it is the sheer energy your body expends trying to repair or replace healthy cells damaged by the chemo. Anemia from low red blood cells only makes it worse.
- Gastrointestinal Issues: The lining of your mouth and digestive tract is in a constant state of renewal. Gemcitabine disrupts this rapid turnover, which can lead to nausea, vomiting, or painful mouth sores.
The key takeaway is that these side effects are signs the medicine is working systemically. By understanding which healthy cells are most at risk, medical teams can provide proactive supportive care. For more detailed advice, check out our guide on managing side effects of cancer treatment.
How Cancer Cells Develop Resistance
Over time, some cancers can become resistant to gemcitabine. The tumor cells essentially evolve, developing clever workarounds to evade the drug's lethal effects. This isn't a single event but a collection of molecular changes that neutralize the gemcitabine mechanism of action.
One of the most common escape routes involves the cellular "doorways." Cancer cells can reduce the number of hENT1 transporters on their surface. With fewer entry points, less gemcitabine can get inside to do its job. The treatment simply becomes far less effective.
Another major resistance tactic targets the activation process itself. A tumor might start producing less of the dCK enzyme, the critical switch needed to "arm" the drug. If dCK levels drop, gemcitabine can get inside the cell but just sits there, completely harmless in its inactive state. This is a primary reason why a tumor that initially responded well may suddenly stop.
By understanding these molecular escape hatches, researchers are constantly developing new strategies to stay one step ahead. This might mean creating drugs that bypass these resistance mechanisms or combining gemcitabine with other agents that can resensitize the tumor. For oncologists, this knowledge is power—it allows us to monitor for signs of resistance and pivot to other therapies when necessary.
Your Top Questions About Gemcitabine, Answered
When you’re facing a cancer diagnosis, the big-picture science is important, but it’s the day-to-day questions that often weigh most heavily on your mind. Here, we'll tackle some of the most practical and frequent questions we hear from patients and families about starting gemcitabine therapy.
How Long Until Gemcitabine Starts Working?
This is one of the first things almost everyone asks, and for good reason. Gemcitabine gets to work on a cellular level right away, starting from your very first infusion.
But seeing those results on a scan takes time. Think of it like a long-term project—the work is happening constantly, but the visible payoff isn't immediate. Your oncologist will typically wait until you've completed a few cycles of treatment before ordering a CT scan or other imaging. This gives the medication enough time to make a measurable dent in the tumor.
Is Gemcitabine a “Strong” Chemo?
Yes, gemcitabine is definitely a powerful and effective chemotherapy drug. Its strength lies in its smart, two-pronged attack: it not only stops new DNA from being made but also chokes off the supply of materials needed to build it. It’s a go-to weapon for some of the toughest cancers we treat.
Of course, in oncology, "strong" is always relative. While it's tough on cancer, it can also affect healthy cells that divide quickly, which is what causes side effects. A huge part of our job is managing those side effects so the treatment remains powerful against the cancer but as gentle as possible on you.
Our goal is always to find that sweet spot: maximizing the drug's impact on the tumor while protecting your quality of life. Constant, open communication with your care team is the key to getting that balance right.
Can I Keep Working During Gemcitabine Treatment?
Many patients do continue to work, but it almost always requires some planning and flexibility. Whether it’s feasible for you really depends on the type of work you do, your treatment schedule, and, most importantly, how you feel.
Fatigue is the big one here—it's a very common side effect and can make a standard 9-to-5 feel like a marathon. It’s a good idea to have a frank conversation with your employer about what’s ahead. Exploring options like a more flexible schedule, remote work days, or adjusted responsibilities can make a world of difference in helping you manage treatment and work successfully.
At Hirschfeld Oncology, we know that answering your questions is just as important as administering your treatment. If you have more questions or are looking at treatment options for advanced cancer, our team is here to help. You can learn more or book a consultation by visiting us at https://honcology.com/blog.





.png)


.png)
.png)




