When you're facing a cancer diagnosis, one of the first and most urgent questions is always, "Will chemotherapy work for me?" The truth is, there's no single answer. The effectiveness of chemo isn't one number but a whole spectrum of possibilities that depends almost entirely on the specific cancer we're fighting.
For some cancers, it’s a powerful, curative tool. For others, it’s one important part of a bigger strategy to control the disease and give you more quality time.
A New Way to Think About Chemotherapy's Effectiveness
Let's try an analogy. Think of chemotherapy as a set of highly specialized tools. For a cancer like testicular cancer, a particular chemo combination is like a precision instrument that can achieve a cure in over 90% of cases, even when the disease has spread. It's one of the great success stories in modern medicine.
But for many other cancers, chemotherapy is more like one tool in a much larger toolbox. We might use it to shrink a tumor before a surgeon removes it, or to clean up any microscopic cancer cells left behind after an operation. In advanced cancer, its job is often to slow down the disease's growth. Its role—and how we measure its "effectiveness"—changes depending on the job at hand.
Defining Success: It's More Than Just Survival Numbers
When your oncologist talks about how well chemo is working, they're looking at a few different things. Getting familiar with these terms can help you feel more in control during those important conversations with your care team.
- Response Rate: This is a direct measure of how much a tumor shrinks—or if it disappears entirely—after treatment.
- Disease Control: For cancers that have spread, a huge win is simply stopping or slowing down tumor growth. This extends the time you can live well without the cancer getting worse.
- Improving Quality of Life: A successful treatment isn't just about the cancer. It's also about managing your symptoms, reducing pain, and helping you keep up with your daily life and the things you love.
This is why a one-size-fits-all approach to cancer is a thing of the past. So much depends on the unique details of your situation. Before we can even begin to talk about success rates, we need to understand several key factors.
Here’s a quick look at the main variables that play a role in your treatment journey.
Each of these elements helps your oncology team build a complete picture.
The real goal of modern cancer care is to tailor the treatment to the person, not just the disease. By understanding your specific cancer, its stage, and your personal health, we can figure out the most effective role for chemotherapy in your unique plan.
This mindset changes the conversation entirely. It’s no longer just about if chemotherapy works, but how it can work best for you. By strategically combining it with newer treatments like targeted therapy and immunotherapy, we can create a comprehensive plan designed to give you the best possible outcome—focused on both the length and the quality of your life.
How Doctors Measure Chemotherapy Success
When you start chemotherapy, the biggest question on your mind is simple: "How will we know if it's working?" Knowing how your oncologist tracks your progress does more than just ease your mind—it makes you a true partner in your own care. Doctors rely on a few key yardsticks to gauge how well chemotherapy is doing its job, and each one tells a different part of your story.
Think of it like checking the stats for a baseball team over a long season. You don't just look at the final championship win. You also track runs per game, defensive plays, and how long the team stays in the hunt for the pennant. Oncologists do something similar, looking for different kinds of "wins" against cancer.
This visual helps map out the journey, from the initial cancer diagnosis to what a successful, personal outcome really looks like.
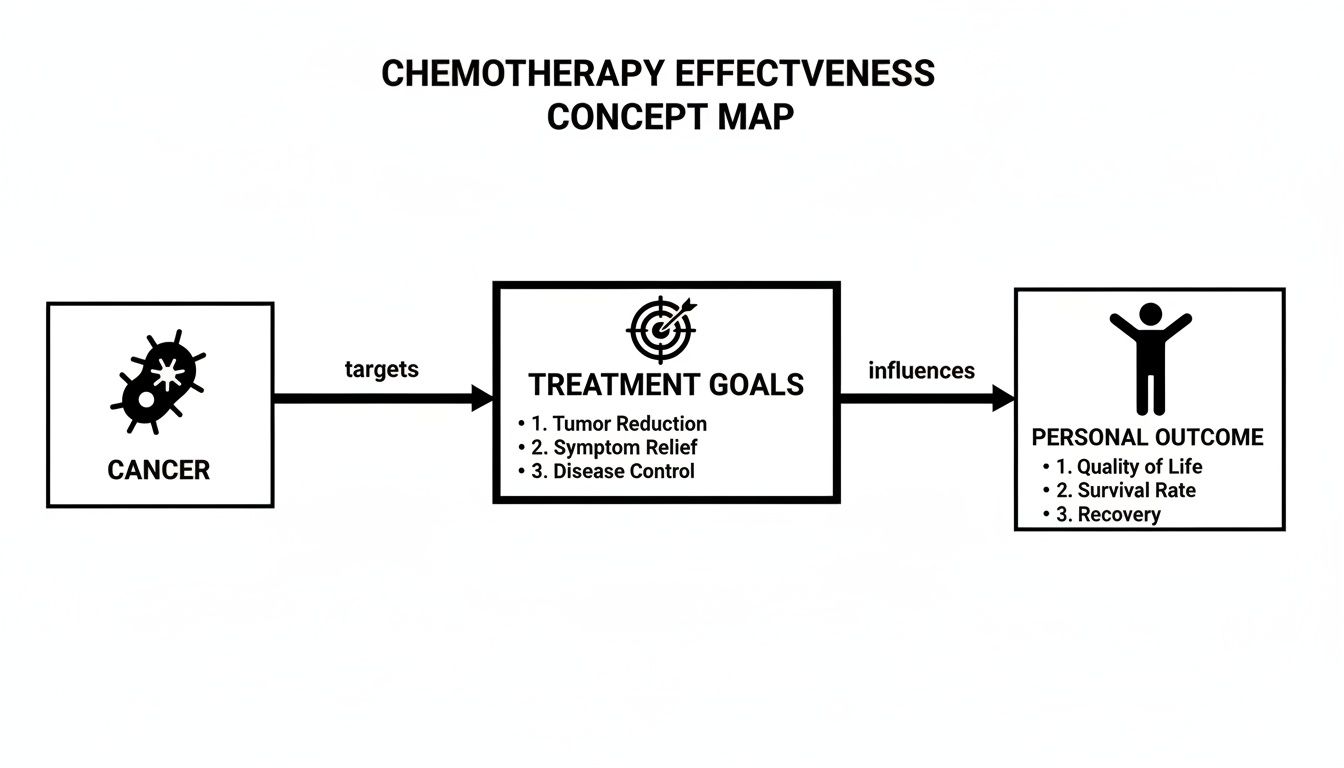
As you can see, a treatment’s effectiveness is all about how well it meets specific, personalized goals—and those goals are different for every single patient.
The Key Metrics for Success
Your care team will use some specific clinical terms to talk about your progress. Let’s break down what these common benchmarks actually mean for you.
Objective Response Rate (ORR): This is the most straightforward measure of how a tumor reacts to treatment. It’s the percentage of patients whose tumors either shrink significantly (a partial response) or disappear completely (a complete response). In our baseball analogy, this is like putting runs on the board—it’s a clear, measurable sign that your game plan is working.
Progression-Free Survival (PFS): This metric looks at the length of time you live with the cancer without it getting worse or spreading. Think of PFS as forcing a stalemate. The treatment has either stopped the cancer's advance or is holding it steady. For many advanced cancers, a long PFS is a huge win, giving you more good-quality time.
Overall Survival (OS): This is the ultimate benchmark, measuring the total time patients live after their treatment begins. While extending life is the fundamental goal of any cancer therapy, OS is the "World Series win" that all treatments are aiming for. It shows the true, big-picture impact of a therapy.
Understanding these different goals is critical. A treatment might not shrink a tumor to nothing, but it could deliver a very long progression-free survival—and that is a major victory in managing the disease. It’s also important to know that sometimes a cancer that responds well at first can learn to outsmart the treatment. If that’s a concern, you can learn more about what happens when chemotherapy stops working in our detailed guide.
The Best-Case Scenario: Pathologic Complete Response
For some early-stage cancers—especially those treated with chemo before surgery (neoadjuvant therapy)—there’s another powerful measure of success.
A Pathologic Complete Response (pCR) means that after chemotherapy is done, a pathologist looks at the surgically removed tissue under a microscope and finds no remaining invasive cancer cells.
Achieving a pCR is an incredible sign. It's strongly linked to a much lower risk of the cancer ever coming back and a higher chance of a long-term cure. It’s the equivalent of not just winning the game but making sure the other team can't even get back on the field. This is a primary goal when treating cancers like certain types of breast cancer and rectal cancer.
By getting familiar with these different measures—from immediate tumor shrinkage to long-term survival—you can have much deeper, more meaningful conversations with your oncologist. It helps you clearly define what success looks like for your journey and celebrate every single victory along the way.
Why Chemotherapy’s Effectiveness Is So Different From Cancer to Cancer
One of the hardest things to grasp about chemotherapy is why it works wonders for one person but might only slow the disease for another. It’s not a simple question with a single answer. The reality is that a treatment that can bring about a complete cure for one type of cancer might have a very different, but still vital, role in another.
Understanding this from the get-go helps set clear, realistic expectations about what chemotherapy can achieve in your specific situation.
Think of it this way: cancer isn't one disease, but hundreds of different diseases that all happen to share a name. Some are like dandelions in a lawn—aggressive and fast-spreading, but with shallow roots that a standard tool can handle effectively. Others are more like deeply rooted ivy, tangled and stubborn, requiring a more persistent, strategic approach. Chemotherapy is an incredibly powerful tool, but its success hinges on the specific "weed" it’s up against.
This isn't a sign of the treatment's failure; it's a direct reflection of the unique biology of each cancer. Let's look at two very different cancer stories to see this in action.
The Gold Standard: Testicular Cancer
When oncologists talk about a true home run for chemotherapy, testicular cancer is almost always the first example that comes to mind. For men diagnosed with this disease, even if it has spread, chemo often represents a genuine, life-long cure.
Why? It comes down to a fundamental weakness in the cancer cells themselves.
Testicular cancer cells are defined by their incredibly rapid growth and division. While that speed is what makes the disease dangerous, it's also its Achilles' heel. Chemotherapy drugs are designed to be most lethal to cells that are actively dividing. Because testicular cancer cells are in this state almost constantly, they are exceptionally vulnerable to the treatment. It’s like they have a giant "kick me" sign that only chemo can see.
This unique sensitivity leads to some of the most impressive success rates in all of oncology.
For testicular cancer, chemotherapy is one of the most effective treatments ever developed. It cures over 90-95% of patients, even in advanced stages—a feat rarely seen in other solid tumors. The introduction of cisplatin-based chemo in the 1970s was a game-changer, pushing long-term survival rates from less than 10% to well over 80% today.
The standard combination of drugs (often BEP: bleomycin, etoposide, and cisplatin) is so effective it can completely eradicate the cancer. This is the perfect example of chemotherapy acting as the primary, definitive weapon against a disease. You can explore more on these chemotherapy success rates for a deeper dive.
The Insurance Policy: Early-Stage Breast Cancer
Now, let’s pivot to a completely different role for chemotherapy. Imagine a woman is diagnosed with an early-stage but aggressive type of breast cancer. Her main treatment will almost certainly be surgery to remove the tumor, often followed by radiation to treat the breast and surrounding lymph nodes.
So, where does chemo fit into this picture?
In this scenario, chemotherapy serves as a crucial insurance policy. The surgeon did their job and removed all the cancer they could see. But the big worry is the microscopic cells that might have already escaped the tumor and are now floating invisibly in the bloodstream or lymph system. These microscopic stragglers are too small to show up on any scan, but they are the seeds of a future recurrence.
This is where adjuvant chemotherapy—chemo given after the main treatment—comes in. Its sole purpose is to hunt down and eliminate these invisible, lingering cells before they can set up shop elsewhere.
- The Goal: Not to shrink a tumor you can see, but to destroy microscopic disease you can't.
- How Success is Measured: We don't see a tumor shrink on a scan. Instead, success is measured by a lower risk of the cancer coming back years down the road.
- The Impact: For many women, adjuvant chemo slashes their recurrence risk by a significant amount, vastly improving their chances of long-term, disease-free survival.
Here, chemo isn't the standalone hero. It's a critical supporting player that works alongside surgery and radiation to lock in the victory and make sure the war is truly over.
The Takeaway: It’s All About the Job It’s Being Asked to Do
Putting these two stories side-by-side reveals the most important lesson: the answer to "how effective is chemotherapy?" is always "it depends on its mission."
For testicular cancer, chemo is the frontline soldier, capable of winning the war on its own. For early-stage breast cancer, it's the silent guardian, preventing a future ambush. And in other situations, like advanced pancreatic cancer, its role might be to control the disease, ease symptoms, and give a person more quality time.
Each of these outcomes is a form of success, defined entirely by the cancer it's fighting and the specific job it needs to do.
Personal Factors That Influence Your Treatment Outcome

While the type of cancer sets the stage, your personal health and the unique biology of your tumor play the leading roles. A successful chemotherapy plan isn't just about matching a drug to a disease; it's about matching the right treatment to the right person at the right time.
Your oncology team looks at a handful of critical factors to build a strategy that gives you the best possible chance of success. When you understand what they're looking for, you can have a much more meaningful and collaborative conversation about your own care.
Cancer Stage: The Most Important Predictor
If there’s one thing that shapes the entire treatment conversation, it’s the cancer stage. Staging is simply a way of describing how far the cancer has moved from where it started. The difference between an early-stage and late-stage diagnosis can completely change the goal of treatment.
Early-Stage Cancer: When a tumor is small and hasn't spread (it's localized), the goal is often a cure. We might use chemotherapy to shrink a tumor before surgery, but more often, it's used after surgery as an "insurance policy" to track down and eliminate any microscopic cancer cells that might have been left behind. In this situation, chemo is a powerful tool for preventing the cancer from ever coming back.
Advanced-Stage Cancer: If the cancer has traveled to distant parts of the body (metastasized), it’s no longer a local problem—it's a systemic one. Here, the primary goal of chemotherapy shifts from cure to control. We aim to slow the cancer's growth, manage symptoms, and give you as much high-quality time as possible.
This distinction is so important because it sets realistic expectations from the start. "Effectiveness" means something very different when you're trying to cure a cancer versus trying to manage it as a chronic condition.
Genomic Testing: Reading the Tumor's Instruction Manual
Here's a fundamental truth in modern oncology: no two tumors are exactly alike, even if they start in the same organ. Every tumor has its own unique genetic "instruction manual" that tells it how to grow, spread, and—most importantly—respond to treatment. This is where genomic testing, also called molecular profiling, comes in.
By analyzing a small piece of your tumor, we can identify specific mutations or proteins that act like the tumor’s Achilles' heel. It’s like finding the secret code that unlocks its vulnerabilities.
Genomic testing is what allows us to move beyond a one-size-fits-all approach. By truly understanding what makes your specific cancer tick, we can select chemotherapy drugs or targeted therapies that are most likely to hit it where it hurts, creating a truly personalized plan.
This detailed map helps us predict how a tumor might react to a certain drug and can even point us toward newer, more precise treatments you might be a candidate for. It’s no longer an optional extra; it's a core part of how we practice today.
Your Performance Status: A Measure of Strength
Your overall health and fitness level heading into treatment are incredibly important. We use a simple but effective scale called Performance Status (PS) to get a snapshot of your ability to handle daily activities. This score helps us predict how well you're likely to tolerate the rigors of chemotherapy.
Someone who is active and feeling well has a good PS and can often handle more intensive chemotherapy, which can sometimes lead to better results. On the other hand, a person who is very weak or ill may need a gentler, lower-dose approach to avoid the treatment doing more harm than good. Your PS isn't set in stone; your team will keep a close eye on it throughout your treatment journey.
Prior Treatments: The Cancer's History
Finally, your own treatment history tells a crucial part of the story. Cancers can be crafty; they can learn to develop resistance to drugs they've been exposed to before. If you've had chemotherapy in the past, your oncologist will need to choose a different type of agent—what we call a "second-line" or "third-line" therapy—to get around that resistance.
Every treatment you've had helps inform the next move. It’s a bit like a chess match, guiding your team to select therapies the cancer hasn't yet learned how to outsmart. This cumulative knowledge is vital for planning long-term strategies, especially for cancers that are advanced or have come back.
Modern Chemotherapy Is A Team Player

The old image of chemotherapy as a lone warrior against cancer is fading fast. In today's oncology, chemo rarely fights on its own. It's now a crucial part of a coordinated team, working in tandem with other powerful treatments to launch a multi-front assault on the disease.
Think of it as a well-planned mission. Chemotherapy often serves as the essential ground force. It moves in to weaken the cancer's defenses and disrupt its ability to grow, making the tumor much more vulnerable to the specialized attacks that follow.
This collaborative strategy is where modern chemotherapy truly proves its worth. By combining it with other therapies, we can achieve results that are far greater than any single treatment could deliver alone.
Partnering with Targeted Therapy
One of chemotherapy’s most important allies is targeted therapy. These are precision drugs, engineered to exploit a cancer's specific genetic Achilles' heel. If genomic testing finds a particular mutation driving a tumor, we can use a drug that acts like a key designed for that exact molecular lock, shutting down the cancer from the inside.
Here’s how they tag-team the cancer:
- Chemotherapy delivers a broad, systemic punch, damaging any rapidly dividing cells it finds.
- Targeted therapy acts more like a sniper, hitting a very specific, pre-identified vulnerability within the cancer cells.
This one-two blow can be incredibly effective. Chemo reduces the overall tumor size, while the targeted drug hones in on the cancer's core survival mechanism. It’s now a standard approach for many cancers, including certain types of lung, breast, and colorectal cancer.
For example, this approach has dramatically improved outcomes in early-stage breast cancer when used after surgery. For stage II-III breast cancer, adding chemotherapy has boosted 5-year survival rates from roughly 60-70% (with surgery alone) to over 85-90% in many cases.
Unleashing the Immune System with Immunotherapy
The other star player on the team is immunotherapy. Unlike chemo, which directly poisons cancer cells, immunotherapy works by taking the brakes off your own immune system, essentially teaching it to recognize and destroy cancer on its own.
Combining chemotherapy and immunotherapy creates a powerful synergy. As chemo kills cancer cells, it forces them to release unique proteins called tumor antigens. These antigens act like red flags, "unmasking" the cancer for the immune system, which has been newly supercharged by immunotherapy, to find and eliminate.
This strategy has been a true game-changer for cancers that were once notoriously difficult to treat, including certain melanomas, bladder cancers, and lung cancers. The chemotherapy delivers the initial blow, and immunotherapy calls in the immune system as reinforcements to finish the job and provide long-term surveillance. If you're curious about how these two approaches work, you can explore the difference between immunotherapy and chemotherapy in our detailed guide.
Why Combination Therapy Is the Future
Using chemotherapy as part of a multi-pronged strategy gives us a decisive edge. It allows oncologists to attack a cancer from several angles at once, making it much harder for the tumor to develop resistance to any single treatment. Ultimately, this approach leads to deeper, more durable responses and better long-term control of the disease.
This is the heart of modern, personalized cancer care. The question is no longer just "how effective is chemotherapy?" but rather, "how can we best deploy chemotherapy alongside other advanced treatments to create a comprehensive plan that gives the patient the absolute best chance of success?"
The Goal: Aggressive Treatment That Doesn't Overtake Your Life
Getting the best possible results from chemotherapy isn’t just about attacking cancer cells—it’s about supporting you as a whole person through every step. An effective treatment plan is one you can actually tolerate well enough to stay on schedule, because consistency is what gives the drugs their best shot at working.
This patient-first mindset is a huge shift from the old days. We're moving away from the "endure it at all costs" mentality and toward a smarter, more sustainable, and often more successful, path.
Smarter Dosing for Better Tolerance
One of the key strategies we use to achieve this balance is called metronomic chemotherapy. Instead of hitting the body with large, infrequent doses that can leave you feeling wiped out, this approach uses much lower doses of chemotherapy given more often.
Think of it like keeping a gentle, constant pressure on the cancer rather than trying to knock it out with a sledgehammer every few weeks. This steady approach is often incredibly effective at preventing cancer from growing and spreading—and usually with far fewer side effects.
The real beauty of metronomic chemotherapy is that it makes treatment a manageable part of your life. When a therapy is easier to tolerate, patients can often stay on it for much longer, which is a critical factor in controlling advanced or treatment-resistant cancers.
This approach is especially powerful when we need a long-term plan that preserves your strength and well-being.
Proactive Support is Key to Staying on Track
A treatment’s success also hinges on having a rock-solid supportive care plan in place from day one. This means we anticipate and manage side effects before they become major problems. We don’t wait for issues to pop up; we work to prevent them from disrupting your treatment and your life.
A truly comprehensive support plan always includes:
- Symptom Management: Using the right medications to proactively control nausea, fatigue, and other common side effects so they don't get the upper hand.
- Nutritional Guidance: Making sure your body has the fuel it needs to stay strong and resilient throughout the entire process.
- Open Communication: Building a partnership where you feel comfortable telling your care team about any issue, big or small, right away.
This holistic focus is non-negotiable. When you feel stronger and fully supported, you're simply better equipped to handle the journey. If you want to learn more, we have another guide that details our approaches to minimizing side effects during cancer treatment.
At the end of the day, a treatment's true power is measured not just by how it impacts the cancer, but by its ability to preserve your quality of life.
Answering Your Questions About Chemotherapy
A cancer diagnosis opens the floodgates to questions and worries. It's completely normal to want to understand the nuts and bolts of your treatment. Let's walk through some of the most common questions we hear from patients about chemotherapy and what they can expect.
Does Having Strong Side Effects Mean The Chemo Is Working Better?
This is a very common myth, but the answer is no, not necessarily. The intensity of your side effects has no direct link to how effectively the chemo is attacking the cancer. Side effects pop up because these powerful drugs target any cell that divides quickly—and that includes healthy cells in places like your hair follicles or the lining of your stomach.
How you react is a unique mix of the specific drugs you receive, the dose, and your own individual body chemistry. In fact, having mild side effects often just means your supportive care plan is doing its job beautifully. It's definitely not a sign that the treatment is failing.
How Soon Will We Know If The Chemotherapy Is Working?
Your oncology team is watching your progress closely right from the start, but the first real check-in usually happens after two or three treatment cycles. This evaluation often involves imaging, like a CT or PET scan, which typically takes place about 6 to 12 weeks after your first infusion.
In some cases, we can get an earlier hint from blood tests that track specific tumor markers. Think of the whole process as a series of checkpoints to make sure your treatment is heading in the right direction.
Can Chemotherapy Cure Stage 4 Cancer?
When we're dealing with most common solid tumors that have spread (like stage 4 breast or colon cancer), the primary goal of chemotherapy shifts from cure to control. The aim is to shrink tumors, put the brakes on the cancer's growth, ease symptoms, and give you more quality time.
That said, there are some really important exceptions. For certain cancers, like testicular cancer and some types of lymphoma, a cure is absolutely the goal and is often achievable with chemotherapy, even at an advanced stage. It really underscores how much the treatment goal depends on the specific type of cancer.
What Happens If The First Chemotherapy Stops Working?
First, don't panic. This is a very common part of the cancer journey and it is far from the end of the road. Cancers can be clever, and sometimes they learn how to outsmart a particular drug. When that happens, your oncologist has a deep bench of other strategies to turn to.
Here’s what that pivot might look like:
- We can switch to a different type of chemotherapy, which we call "second-line" therapy.
- We might add a targeted therapy or immunotherapy drug to work alongside the chemo.
- We could look into a clinical trial that’s testing a promising new treatment.
The key is to remain flexible and one step ahead. We use the cancer's response to the first treatment to inform our next, smarter move.
At Hirschfeld Oncology, our focus is on building personalized treatment regimens for patients with advanced, complex, or treatment-resistant cancers. If you're looking for a second opinion or want to explore what lies beyond standard care, our team is ready to help with compassionate, expert guidance. You can learn more about our patient-centered approach.





.png)


.png)
.png)




