When patients first hear they need chemotherapy, one of the most common questions is, "How often will I have to do this?" There's no single, simple answer. A chemo schedule is incredibly personal, with treatments ranging from daily to weekly, every few weeks, or even monthly. The best way to think about it is like a highly specialized workout plan—periods of intense effort followed by crucial time for rest and recovery.
Decoding Your Chemotherapy Schedule
Sorting through your treatment plan can feel overwhelming at first, but it all comes down to one key idea: the chemotherapy cycle. A "cycle" is just one round of treatment followed by a break. This rhythm is the blueprint for your entire schedule, and your oncology team designs it to strike a very delicate balance.
The goal is always twofold: hit the cancer cells hard while they're vulnerable and then give your body's healthy cells enough time to recover. That pause between treatments is just as vital as the infusion itself. It's when your immune system rebuilds and your body gets a handle on side effects before the next round begins.
Why Every Schedule Is Unique
Your chemotherapy schedule isn't pulled from a generic template; it’s a detailed plan crafted just for you. Your oncologist considers a whole host of personal factors, including:
- The type and stage of your cancer: Different cancers have different growth patterns and vulnerabilities, so they respond better to certain treatment rhythms.
- The specific drugs being used: Every chemotherapy agent works differently and has its own unique timeline for effectiveness and side effects.
- Your overall health: Your body’s ability to tolerate and recover from treatment is a huge factor in deciding the intensity and frequency of your cycles.
This is why your schedule might look completely different from another patient's, even if you have a similar diagnosis. This careful, personalized planning is at the heart of modern cancer care.
As we refine these schedules, the global need for chemotherapy is growing. Projections show that the number of patients requiring first-line treatment will jump from 9.8 million to 15 million annually by 2040. This 53% increase underscores just how critical evidence-based, precise scheduling is for patients worldwide.
Setting Expectations for Treatment
As you start this journey, it's helpful to view your schedule as a dynamic guide, not something set in stone. Your oncology team will monitor you closely, and they may adjust the timing based on your blood test results, how you're managing side effects, and how the cancer is responding.
Feeling prepared and empowered to ask questions makes all the difference. Our guide on how to prepare for chemotherapy offers some great, practical tips to help you get ready.
To give you a clearer idea of what your plan might look like, here's a quick breakdown of some common chemotherapy frequencies.
Common Chemotherapy Frequencies At A Glance
This table summarizes some of the most common schedules you might encounter, explaining the logic behind each one and the types of cancer they're often used for.
Of course, this is just a general overview. Your own schedule will be determined by the unique factors of your diagnosis and your specific treatment goals.
The Rhythm of Treatment: Understanding Cycles and Schedules
When you're trying to figure out how often you'll get chemotherapy, it helps to think of it as having a specific rhythm. This isn't just a random schedule; it's a carefully planned pattern built on two core ideas: cycles and schedules.
I often use a gardening analogy with my patients. Imagine spending a full day meticulously pulling weeds from your garden—that’s the treatment. Afterwards, you don’t go back the very next day. Instead, you give the garden a few weeks for the healthy plants to recover and grow stronger. That rest period is just as important as the weeding.
This intentional pattern is what your treatment plan is all about. It’s designed to hit the cancer cells hard while giving your body the downtime it needs to bounce back.
What Is a Chemotherapy Cycle?
A chemotherapy cycle is simply one round of treatment followed by a period of rest. For example, if you get an IV infusion on a Monday and your next one isn't for another three weeks, that entire 21-day period makes up one full cycle. Your oncology team carefully selects the length of a cycle—it could be weekly, every two weeks, or even monthly.
That break between infusions isn't just empty time. It's a crucial recovery phase. It gives your healthy cells, especially the important ones in your bone marrow that make new blood cells, a chance to regenerate. This rest is key to managing side effects and making sure your body is strong enough for the next dose.
The whole point of a cycle is to find that sweet spot: maximizing the damage to cancer cells while giving your healthy cells enough time to heal before the next round.
The total number of cycles you'll go through is known as your course of treatment. Sometimes this is a fixed number, like six cycles. In other cases, treatment might continue as long as it's working well and the side effects are tolerable.
Defining Your Regimen and Schedule
While a "cycle" gives you the big-picture timing, the words regimen and schedule get into the nitty-gritty details. People often use them interchangeably, but they mean slightly different things.
Regimen: Think of this as the "recipe" for your treatment. It lists the exact chemotherapy drugs you’ll get, the precise doses, and how they’ll be given (like through an IV or as a pill). A well-known regimen for lymphoma, for instance, is called "CHOP," an acronym for the four different drugs used in the combination.
Schedule: This is the calendar for your regimen. It spells out exactly which days you receive treatment within each cycle. Some schedules are straightforward—you might just come in for an infusion on Day 1 of a 21-day cycle. Others can be more complex, maybe requiring treatment on Day 1 and Day 8 of a cycle, or even taking pills daily for two weeks and then having one week off.
Your schedule is the practical, day-to-day blueprint for your treatment. It's what determines your appointments and helps you plan your life. This careful timing ensures the drugs are in your system when they can be most effective against cancer cells, catching them when they're trying to grow. Understanding this rhythm can really help take the mystery out of the process and make you feel more in control of your care.
What Shapes Your Personal Chemotherapy Plan?
Why does one person come in for weekly chemo while another has an infusion just once a month? The simple answer is that no two cancer treatment plans are ever exactly the same. Your oncology team basically acts like a group of master strategists, carefully weighing a whole host of complex factors to design a schedule that’s built specifically for you.
This isn't a cookie-cutter process. It's a personalized approach grounded in a deep understanding of your unique situation. Let's walk through the key elements your team considers to figure out the "how often" of your chemotherapy, all to make a plan that’s tough on cancer but as manageable as possible for you.
Your Diagnosis: The Starting Blueprint
First and foremost, the most significant factor shaping your chemo schedule is the cancer itself. Your diagnosis is the essential blueprint from which the entire treatment plan is built.
- Type of Cancer: Different cancers just have different personalities. A fast-growing cancer, like certain types of lymphoma, might demand a more frequent or intense schedule to keep it from multiplying out of control. On the other hand, slower-growing tumors might respond better to a less frequent but more powerful dose.
- Stage of Cancer: The stage—meaning how far the cancer has spread—also dictates the strategy. For an early-stage cancer, treatment might involve a set number of chemo cycles right after surgery, with the goal of wiping out any microscopic cells left behind. In contrast, an advanced cancer might require ongoing treatment to manage the disease, which makes the long-term sustainability of the schedule a top priority.
- Genetic Makeup: We now understand that even cancers in the same part of the body can have very different genetic markers. These unique features can make a tumor especially vulnerable to certain drugs, which in turn helps determine the most effective timing and frequency for giving those medications.
The Specific Drugs in Your Regimen
Once your oncologist has a clear picture of the cancer, they select the best "tools" for the job—the specific chemotherapy drugs that make up your regimen. Each of these drugs comes with its own set of rules for how it works and how your body processes it.
Think of it like taking medication for a headache. A fast-acting pain reliever might need to be taken every four hours, while a long-lasting one is just once a day. Chemotherapy drugs work on a similar principle. Some are flushed from the body fairly quickly and are more effective when given in smaller, more frequent doses. Others are incredibly potent and require a longer rest period for your body to recover from their powerful effects. This is why a common regimen like FOLFOX for colorectal cancer is often given every two weeks, while others might be spaced 21 or 28 days apart.
A chemotherapy plan is a dynamic strategy, not a static prescription. The timing is designed to keep maximum pressure on cancer cells when they are most vulnerable while giving your healthy cells the precise amount of time they need to recover.
Your Overall Health and Treatment Goals
Your personal health is a huge piece of the puzzle. Simply put, your body’s ability to handle the stress of treatment directly impacts how often you can receive it. Your oncology team will be keeping a close eye on your blood counts, how your kidneys and liver are functioning, and how you're coping with side effects.
If you’re bouncing back well between cycles, the schedule will likely proceed as planned. But if you’re struggling with significant side effects, like dangerously low white blood cell counts, your doctor might delay the next cycle to give your body extra time to heal. This kind of flexibility is a normal and necessary part of keeping you safe.
The overarching goal of your treatment also plays a big role in the schedule.
- Curative Intent: When the goal is to cure the cancer, the schedule might be more aggressive and intense, with a clear end date in sight.
- Palliative Care: If the goal is to manage symptoms and improve quality of life with an advanced cancer, the schedule is designed for long-term tolerability. This could mean lower doses or longer breaks between treatments.
How Other Treatments Affect Your Schedule
These days, chemotherapy is often just one part of a multi-pronged attack on cancer. When it’s combined with other therapies, the timing has to be coordinated perfectly.
- Radiation Therapy: If you're also getting radiation, your chemo might be scheduled on the same days to make the cancer cells more sensitive to the radiation's effects. This tag-team approach is called chemoradiation.
- Immunotherapy or Targeted Therapy: Combining chemo with newer treatments like immunotherapy can be a game-changer. The schedule has to be planned so the treatments work together, not against each other. For instance, chemo might be given first to weaken the cancer cells, making them an easier target for the immunotherapy-boosted immune system to find and destroy.
Your oncology team meticulously balances all these factors. Crafting these complex, personalized schedules demands an incredible level of expertise—a challenge that is only growing globally. In fact, the global cancer physician workforce must expand significantly to meet future needs, with estimates showing a need for 100,000 cancer physicians by 2040, a big jump from 65,000 in 2018. You can explore more about these workforce demands in oncology. Here at Hirschfeld Oncology, our patient-centered approach ensures every detail of your health and your goals is at the heart of the plan we create for your path forward.
Seeing It In Action: Real-World Chemotherapy Schedules
Theory is one thing, but seeing how these concepts play out in a real treatment plan makes all the difference. The question "how often is chemotherapy given?" really comes to life when you look at the specific schedules oncologists design to fight different cancers. Each one is a careful balance of the cancer type, the drugs being used, and a patient's overall health.
Let's walk through a few concrete examples to see what these different treatment rhythms actually look like.
The timeline below breaks down the core elements—your specific cancer, the rules of the drugs, and your personal health—that all come together to create a personalized chemotherapy plan.
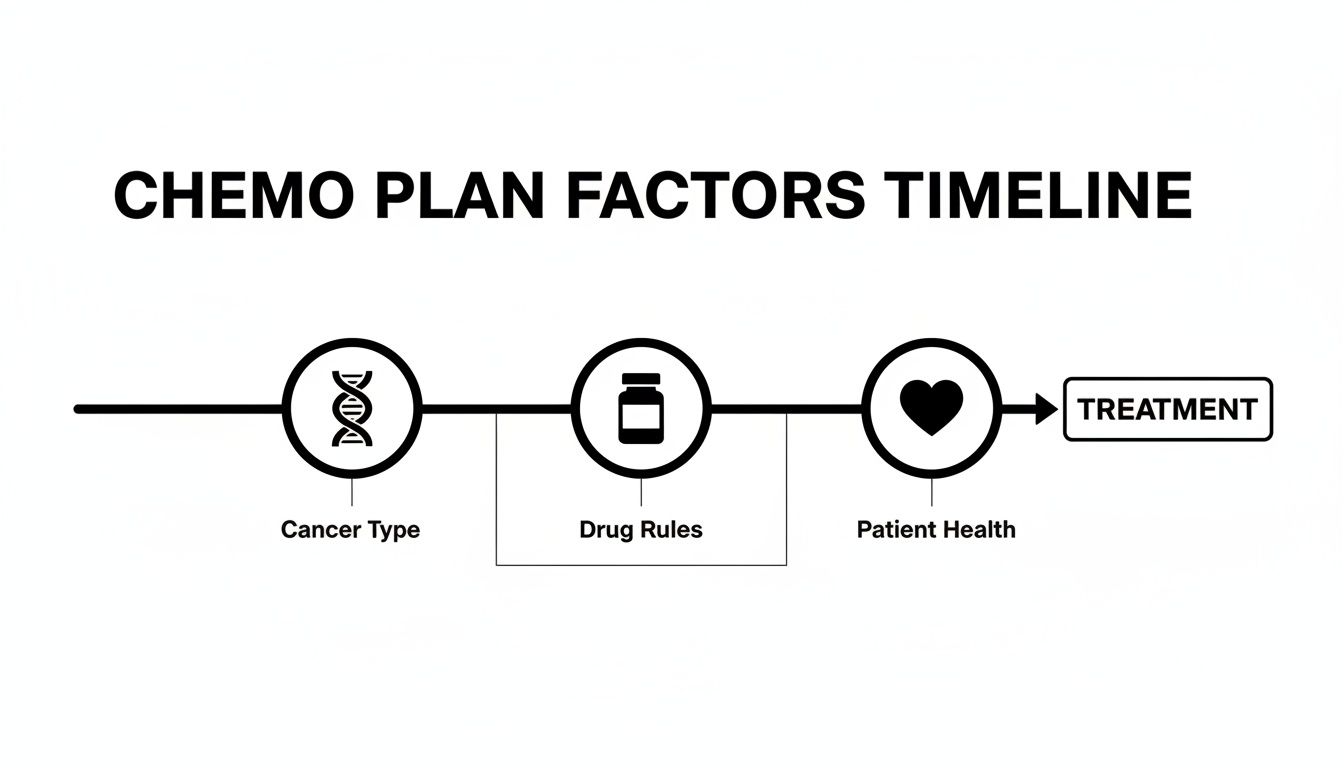
As you can see, your treatment schedule isn't based on a single factor. It’s a thoughtful strategy built by balancing these critical pieces to give you the best possible outcome.
To illustrate this, let's compare some of the most common chemotherapy regimens. Each one has a unique cadence tailored to the type of cancer it's meant to fight.
Example Chemotherapy Regimens And Schedules
These examples show just how much the timing can vary. The goal is always the same: to hit the cancer cells when they are most vulnerable while giving healthy cells just enough time to recover.
Weekly Chemotherapy: The Steady Approach
Sometimes, a steady and more frequent approach works best. A weekly schedule involves a lower dose of medicine given more often. This can keep constant pressure on the cancer cells while being gentle enough to minimize some of the harsher side effects.
A classic example of this is the drug paclitaxel, often used to treat breast cancer.
- The Schedule: A patient typically comes in for an IV infusion of paclitaxel once every week for 12 consecutive weeks.
- The Cycle: In this setup, each week is its own little cycle. You get the treatment, then have a short, six-day recovery period before the next dose.
- The Rationale: This consistent pressure helps prevent cancer cells from repairing themselves and can be much easier for the body to handle than one massive dose.
Bi-Weekly Chemotherapy: The Dose-Dense Rhythm
A bi-weekly, or "dose-dense," schedule is all about increasing the treatment's intensity by shortening the rest period. For certain aggressive cancers, this can be incredibly effective because it gives the cancer cells less time to regrow between rounds.
The FOLFOX regimen, a cornerstone of colorectal cancer treatment, is a perfect illustration.
- The Schedule: A patient receives an IV infusion on Day 1 of the cycle. They might also be sent home with a small, portable pump that continues delivering one of the drugs for the next 48 hours.
- The Cycle: This is a 14-day cycle. After the initial treatment, the patient gets about 11-12 days to recover before the whole process starts again on what would be Day 15.
- The Rationale: Hitting the cancer hard and fast every two weeks is a strategic way to try and overwhelm it, hopefully overcoming any drug resistance the cells might develop.
Three or Four-Week Cycles: The High-Impact Plan
Longer cycles—usually 21 or 28 days—are designed to allow for higher, more powerful doses of chemotherapy. This approach requires a longer recovery period so your body has time to rebuild healthy cells, especially the white blood cells and platelets produced in your bone marrow.
The well-known CHOP regimen for non-Hodgkin lymphoma is a great example of a 21-day cycle.
A 21-Day Cycle in Practice:
On Day 1, you receive your IV infusion of all the drugs in the CHOP combination. Then, you go home for a 20-day rest period. That entire 21-day block completes one full cycle, and at the end of it, you’re ready to begin the next one.
This extended break is absolutely essential for your body to bounce back from the potent drugs, ensuring you're strong enough for the next round. Having a comfortable and well-run facility for these treatment days makes a huge difference; you can learn more about what to look for when finding a local cancer infusion center near me in our guide.
IV Infusions vs. Oral Chemotherapy
The way you receive chemotherapy also has a huge impact on your schedule. IV infusions deliver a powerful, concentrated dose all at once during an appointment, which is then followed by a treatment-free rest period.
Oral chemotherapy, taken as a pill at home, completely changes the dynamic. A schedule might involve taking a pill every day for two weeks, followed by one week off. This creates a more continuous, low-level exposure to the drug. For certain cancers, this can be just as effective while offering much more flexibility in your day-to-day life.
Navigating Your Recovery: The Importance Of Rest Periods

The time between chemotherapy sessions is so much more than just a break. It's an active, essential part of your treatment plan where your body does some of its most critical work—repairing healthy cells and gearing up for the next round. Understanding what’s happening "behind the scenes" during this time can make all the difference in how you manage it.
I like to think of it this way: Chemotherapy is the demolition crew, tasked with clearing out the cancer cells. But the rest period? That’s when the rebuilding crew comes in to repair the healthy parts of the structure, ensuring the whole building stays strong. This "off-time" is non-negotiable for a successful outcome.
Rebuilding Your Body’s Defenses
Chemo drugs are powerful, but they aren't always great at telling the difference between a cancer cell and a healthy, fast-dividing cell. This is why the cells in your bone marrow, the factory for your blood, often take a hit. The rest period is specifically calculated to give these vital cells a chance to bounce back.
During this break, your body is laser-focused on replenishing its key players:
- White Blood Cells: These are the soldiers of your immune system. The break allows their numbers to climb back to safe levels, lowering your risk of infection.
- Platelets: These tiny cells are crucial for proper blood clotting. The recovery phase lets their count recover, which helps prevent issues with bruising and bleeding.
- Red Blood Cells: As the oxygen carriers in your body, these cells are rebuilt during the break, which is a big factor in combating the deep fatigue many patients feel.
The rest period is a core part of your treatment strategy. It’s a calculated pause that allows your body to heal, ensuring you remain strong enough to continue therapy safely and effectively.
This rebuilding process is precisely why your chemo schedule has those built-in breaks, whether they last for a few days or a few weeks.
Understanding the Timeline of Side Effects
Side effects don't always run like clockwork, and what you experience in one cycle might be different from the next. Some pop up almost immediately after an infusion, while others can take several days to show up.
For instance, nausea is often most intense in the first 24 to 72 hours after treatment. Fatigue, on the other hand, tends to build over several days, often peaking midway through your recovery period before it starts to ease up. Hair loss typically doesn't begin until two or three weeks after your very first cycle.
Keeping a simple journal to track your symptoms can be incredibly helpful. Just jotting down what you're feeling and when gives your care team valuable information to adjust your medications and keep you more comfortable. Managing symptoms is key, and we have many strategies to help. You can find more detailed advice in our guide on enhancing your quality of life during cancer therapy.
When to Call Your Oncology Team
Your rest period is for recovery, but it’s also a time to be vigilant. Your oncology team is your partner, and we need to know if you experience certain symptoms. Please don't ever hesitate to call us if you have:
- A fever of 100.4°F (38°C) or higher
- Nausea, vomiting, or diarrhea that you can't get under control
- Any signs of infection, like chills, a new cough, or a sore throat
- Unusual bleeding or bruising
Staying in close communication allows us to tackle any issues quickly, which keeps your treatment on track and, most importantly, protects your health. This proactive approach helps you navigate your recovery with confidence.
Questions to Ask Your Doctor About Your Schedule
Walking into an appointment with your oncologist can feel overwhelming. There's a lot of information to take in, and it's easy to forget what you wanted to ask in the moment. Coming prepared with a list of questions can make a world of difference.
Think of it as your personal road map for the conversation. To help you feel more in control and act as a true partner in your own care, we’ve put together some key questions. They’re broken down by topic, covering everything from the high-level plan to the nitty-gritty of daily life.
Understanding My Treatment Plan
The first step is to get a solid handle on the basics of your schedule. These questions are all about the "what," "why," and "how long" of your specific chemotherapy, helping you see the full picture.
- What is the name of my specific chemo regimen? (e.g., "FOLFOX," "AC-T")
- How many cycles are we planning for the entire course of treatment?
- How long does one cycle last, and on which days will I actually get my infusion or take my pills?
- What is the main goal here? Are we aiming for a cure, to control the cancer long-term, or to manage my symptoms?
- How will we track if the treatment is working? What scans or tests will we be doing?
A Note on Clarity: Getting the specifics down is empowering. Simply knowing the name of your regimen and the length of your cycles turns a confusing, abstract process into a structured, predictable calendar. It gives you a framework to build on.
Managing Side Effects and Daily Life
Treatment is only one part of the equation; how you feel day-to-day is just as critical. These questions tackle the practical side of things, helping you plan your life and stay ahead of side effects.
- What are the most common side effects I should watch out for with this schedule?
- When, during a cycle, are those side effects likely to peak? (e.g., "Day 3 is often the toughest.")
- Is there anything I should change about my diet—foods to eat more of or to avoid?
- Who do I call if I have a problem after hours or on a weekend? What's the emergency number?
- Can I still work, exercise, or travel during my "off" weeks? What limitations should I know about?
Here at Hirschfeld Oncology, we want you to ask these questions. And any others that come to mind! Open, honest communication is the bedrock of good care. Our team is here to give you clear answers and make sure your treatment plan works for your health and your life.
We Answer Your Most Common Questions About Chemo Schedules
Once you leave the clinic and get home, a dozen new questions about your chemotherapy plan can pop into your head. That’s completely normal. Sorting through all this new information is a process, and we want to provide clear, straightforward answers to the questions we hear most often.
Can My Chemotherapy Schedule Change During Treatment?
Yes, absolutely. Think of your initial treatment plan as a roadmap, not a rigid set of tracks. Your oncology team is constantly checking in on you—through blood tests, physical exams, and simply talking with you about how you’re feeling.
It’s very common to adjust the plan along the way. We might delay a cycle if your blood counts need more time to recover, or we might reduce a dose if side effects are hitting you too hard. These changes aren’t setbacks; they’re a sign of smart, personalized care designed to keep your treatment as safe and effective as possible.
If I Have Chemo More Often, Does That Mean My Cancer Is More Aggressive?
Not necessarily. How often you receive chemotherapy is less about the cancer's aggression and more about the specific drugs we’re using and how they work best against your particular type of cancer. It’s all about finding the right rhythm.
Some drugs are most effective when given in smaller, more frequent doses, which keeps constant pressure on the cancer cells. Others deliver a bigger punch with a single, powerful dose, followed by a longer break for your body to heal. Your schedule is custom-built to maximize the drug's impact on the cancer while giving your healthy cells the best chance to bounce back.
The Bottom Line: Treatment frequency is a strategic decision based on the science behind the drug and the biology of the cancer. A weekly schedule isn't inherently "better" or "worse" than a schedule with treatments every three weeks—it's just the right tool for that specific job.
How Does a Maintenance Chemotherapy Schedule Work?
Maintenance therapy is a whole different ballgame. It usually starts after you’ve finished the main, more intensive phase of your treatment. The goal here shifts from actively fighting the cancer to keeping it from coming back or holding it in check long-term.
Because the purpose is prevention, the schedule is much less demanding. You might come in for a lower-dose infusion just once a month or even every few months. This gentler approach is designed to be sustainable over a long period, with far milder side effects, so you can focus on living your life well.
At Hirschfeld Oncology, we know that understanding your treatment is just as important as the treatment itself. Clear communication is at the heart of everything we do. If you have questions about your plan or want to explore your options, our team is here to give you the answers and support you need. Find out more about our patient-first philosophy and how we can walk with you on this journey by visiting our Patient Resources blog.





.png)


.png)
.png)




