When you're dealing with a cancer diagnosis, it can be hard to find the right words to describe how you're truly feeling day-to-day. Words like "tired" or "weak" are subjective and can mean very different things to different people. This is where the ECOG Performance Status comes in.
It’s a straightforward 0-5 scale that gives your oncology team a clear, standardized way to understand how your cancer is affecting your daily life and abilities. Think of it less as a grade and more as a crucial piece of communication—a snapshot of your overall well-being.
A Common Language for Your Care
The ECOG scale creates a common language for everyone involved in your care. It translates your ability to handle daily routines into a simple number, removing ambiguity and ensuring your entire care team is on the same page.
This simple score helps answer some of the most important questions about your treatment path:
- Are you able to manage daily self-care, work, and your usual hobbies?
- How much independence do you have, or do you need help from others?
- How much of your day is spent resting or in bed?
By looking at these practical aspects of your life, your oncologist gains a much clearer picture of your physical resilience and how you might tolerate a specific treatment. First published in 1982, this scale, developed by the Eastern Cooperative Oncology Group (ECOG), has been the gold standard in oncology for over 40 years, guiding countless treatment decisions. You can learn more about its history and impact from sources like My Palliative Care Now.
The Big Picture: Your ECOG score is more than just a number. It's a reflection of your quality of life at a given moment. It directly helps determine if a proposed treatment is a realistic and beneficial option for you, making sure your care plan truly fits your life.
Before we break down each grade in detail, the table below offers a quick summary. It's a handy reference to see how each number corresponds to a person's functional level.
Decoding Each ECOG Grade with Real-Life Scenarios
To really get a handle on the ECOG Performance Status, we have to look past the numbers and see what they mean for a person’s day-to-day life. The scale gives us a vital snapshot of how a patient is doing, which in turn helps shape their entire treatment plan.
Let's break down each level with some relatable, real-world scenarios.
The diagram below shows how your overall well-being gets translated into a simple ECOG score. That score then becomes a cornerstone for building your treatment strategy.
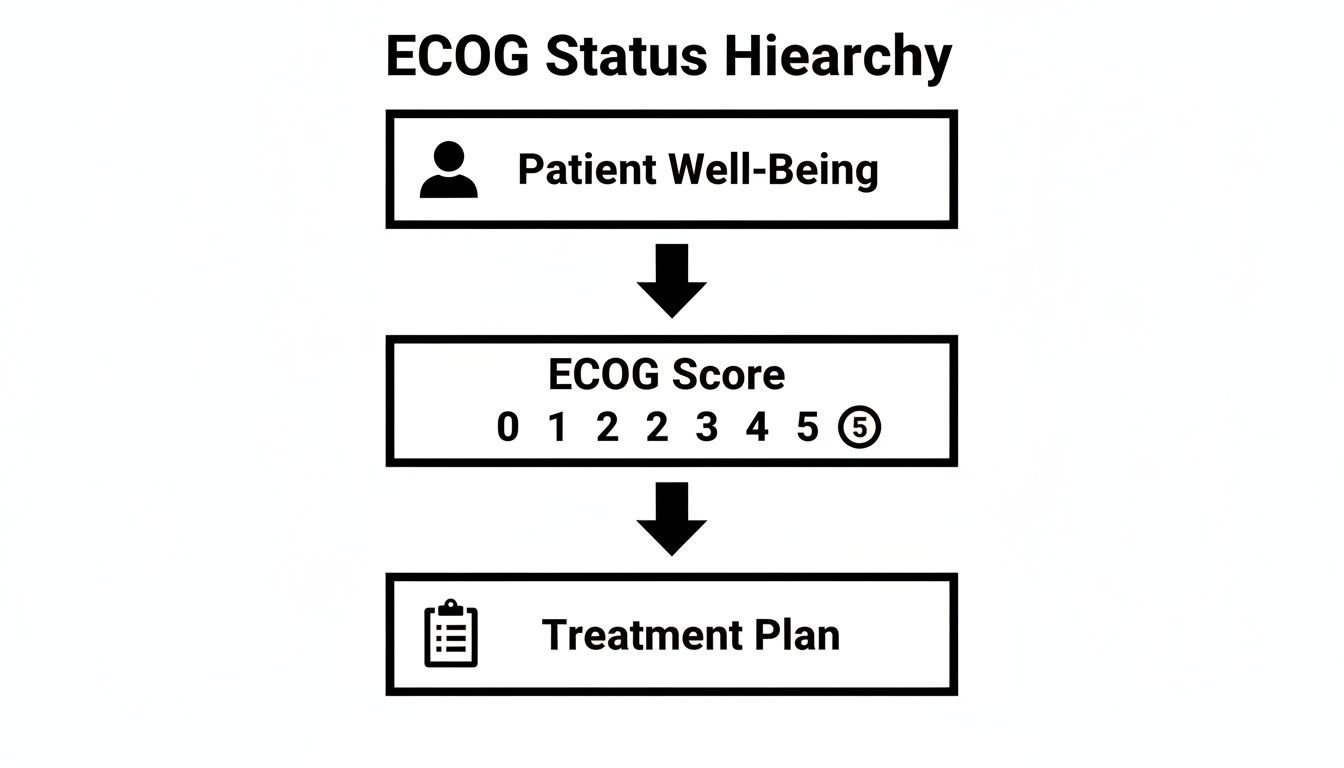
This visual helps reinforce just how central the ECOG score is. It’s the bridge connecting your personal experience with the illness to the clinical decisions being made.
ECOG 0: Fully Active and Symptom-Free
A person with an ECOG 0 is essentially living their life without restrictions from their cancer. They are fully active and can do everything they did before their diagnosis.
Think of a high school teacher recently diagnosed with an early-stage cancer. Despite the diagnosis, she continues to teach full-time, manage her household, and even go for her regular morning runs. Her cancer isn't holding her back in any noticeable way.
ECOG 1: Symptomatic but Getting Around Fine
An ECOG 1 score is for someone who is feeling some symptoms but is still completely ambulatory, or "up and about." They might have to cut back on physically strenuous activities, but they can handle light housework or office work without a problem.
Imagine a freelance graphic designer who feels persistent fatigue from his treatment. He can no longer go on long bike rides and finds himself needing more breaks. But, he can still work from his home office, manage light chores, and walk his dog around the block. That’s a classic ECOG 1.
A patient's ECOG status is a key piece of the puzzle for many clinical trials. For instance, studies for new lung cancer treatments often require participants to have an ECOG score of 0-1. This shows they are well enough to tolerate potentially demanding experimental therapies.
ECOG 2: Up and About, but Needing to Rest
A score of ECOG 2 describes someone who can take care of themselves but can no longer work. They are up and moving around for more than 50% of their waking hours but need to take significant rest periods.
Picture a retired grandmother who has always loved gardening. Now, because of her illness, she has to spend a good part of her day resting on the couch. She can still get dressed and make a simple meal, but she doesn't have the energy for her garden or to go grocery shopping alone anymore. That shift is the hallmark of ECOG 2.
ECOG 3: Limited Self-Care, Needs Assistance
When a person has an ECOG 3 score, their self-care ability is limited. They are confined to a bed or chair for more than 50% of the time they're awake.
This might be a patient who spends most of his day in a recliner, watching TV or dozing. He needs help from a family member or caregiver to bathe and get dressed. While he might be able to feed himself, he needs assistance with nearly everything else. This level marks a significant decline in functional ability.
ECOG 4: Completely Disabled, Unable to Care for Self
At ECOG 4, an individual is completely disabled. They can't perform any self-care and are confined to a bed or chair, requiring total care from others.
For example, a patient at this stage may be bedridden, unable to move without help, and dependent on others for all their needs, from eating to personal hygiene. This score reflects a severe state of illness.
ECOG 5: Deceased
The final grade, ECOG 5, simply means the patient has passed away. This score is primarily used for record-keeping and documenting outcomes in clinical data.
By seeing these real-life examples, the abstract numbers of the ECOG scale start to make a lot more sense. This clarity helps patients and their families have more effective, meaningful conversations with their oncology team.
How Your ECOG Score Guides Your Treatment Plan
Your ECOG performance status is so much more than a number on a chart. It’s one of the most practical tools your oncologist has for mapping out your treatment journey. Think of your doctor as a strategist planning a complex campaign; your ECOG score is a key piece of intelligence that tells them how much "firepower" your body can safely handle at any given moment.
This score has a direct impact on the intensity and type of therapies your team will recommend. A strong score can mean you're a candidate for more aggressive treatments, while a weaker one signals that a gentler, more supportive approach is needed.
Matching Treatment Intensity to Your Strength
For patients with a low ECOG score—a 0 or 1—the door is usually open to a wider range of options. Because you're either fully active or just slightly slowed down, your body is generally better prepared to tolerate the demanding side effects that can come with aggressive chemotherapy or combination drug regimens.
This resilience is also why most clinical trials require participants to have an ECOG score of 0-1. Researchers need to know that a patient is strong enough to handle an investigational therapy.
On the other hand, a higher ECOG score, like a 3 or 4, tells a very different story. For someone who is spending most of their day in bed, hitting them with aggressive chemo could easily do more harm than good. The risk of severe toxicity often outweighs any potential benefit. In these situations, the focus naturally shifts.
The goal is always to strike the right balance between fighting the cancer and preserving your quality of life. The ECOG score is the guide that helps ensure a treatment plan makes sense for your body, right now.
A Dynamic Guide for Adjusting Your Care
It’s so important to remember that your ECOG score isn't set in stone. It’s a snapshot in time. As your health changes, so will your score—and your treatment plan should adapt right along with it.
For instance, an effective treatment might shrink tumors and ease your symptoms, causing your ECOG score to improve. That's a fantastic development! This positive shift could open up new possibilities for different or more intensive therapies that weren't on the table before.
The reverse is also true. If a particular treatment is causing debilitating side effects and your score gets worse, that's a clear signal for your oncology team to make a change. They might lower the dose, switch medications, or bring in more supportive care to help you feel better. This is also when your team might explore other strategies, like precision oncology, which can offer targeted drugs with more manageable side effect profiles.
Ultimately, understanding your ECOG status empowers both you and your doctor. It creates a common language for discussing your health and making decisions together, ensuring your care plan always reflects your current reality. This shared understanding is fundamental to achieving better patient care and making sure every step of your journey is truly aligned with your well-being.
What Does Your ECOG Score Mean for Your Prognosis?
It's a question every patient asks: "What does this number mean for my future?" Your ECOG score is a vital part of the conversation, but it's just that—one part of a much bigger, more personal picture. It's not a crystal ball.
Generally, a lower score (ECOG 0 or 1) points toward a more favorable outlook. The reason for this is practical, not predictive. Patients who are stronger and more active can typically handle more aggressive and effective treatments. Being able to tolerate a full, robust therapy plan often translates into better results.
A Snapshot in Time, Not a Life Sentence
Think of your ECOG score as a snapshot of how you’re doing today. It’s a measure of your current functional ability, not a permanent label. Your status can—and frequently does—change throughout your cancer journey. This is where hope meets action.
Your score isn’t set in stone. Many things can affect it, and with the right support from your care team, you can actively work to improve it.
Your ECOG score is a dynamic measure, not a static destiny. Focusing on your day-to-day well-being, managing symptoms, and working with your care team can directly influence your functional status, potentially improving your score over time.
Taking Control: How to Influence Your Score
This is where proactive care makes a huge difference. By getting ahead of treatment side effects like nausea, fatigue, and pain, you can hold onto your energy and independence. This has a direct, positive impact on your ability to handle daily activities—the very thing the ECOG scale measures.
Here are a few ways you and your team can work together:
- Aggressive Symptom Control: Don't just "tough out" side effects. Addressing pain or fatigue with the right medications and therapies can dramatically improve your daily function.
- Nutritional Support: A dietitian can help ensure your body is getting the fuel it needs to stay strong, which is fundamental to feeling better and staying active.
- Physical and Occupational Therapy: Guided, gentle exercise can help you maintain strength and mobility, preserving your independence and improving your stamina.
In the end, your ECOG score is a tool that helps guide your care. It provides a useful starting point, but your journey is uniquely yours. It’s shaped by your treatment choices, your personal resilience, and the proactive steps you take to manage your health every single day.
Beyond ECOG: How Patient Assessment Is Evolving
While the ECOG score is a pillar of modern oncology, it's not the only way we measure a patient's functional health. It's part of a much bigger, constantly improving toolkit. For decades, another scale, the Karnofsky Performance Scale (KPS), has also been widely used.
Think of it this way: if ECOG is a simple 6-point scale (0–5), KPS is a much more detailed ruler. It ranges from 100 (perfectly healthy) down to 0 (death) in increments of 10, giving clinicians more granular options to describe a patient's status.
So why isn't KPS the universal standard? The straightforward nature of the ECOG scale is its greatest strength. In a busy clinic or a large-scale clinical trial, its simplicity allows for a quick, reliable assessment that everyone on the care team can grasp immediately.
ECOG vs. Karnofsky (KPS): A Quick Comparison
Here's a look at how the two most common performance scales stack up against each other. While both aim to quantify a patient's functional ability, they do so with different levels of detail.
Ultimately, the choice between ECOG and KPS often comes down to the specific clinical setting and the level of detail required.

The Future of Assessment: It's All in the Data
The most significant changes in patient assessment are now coming from technology. We're moving beyond static scores taken during appointments and into a more dynamic, continuous understanding of a patient's health. Artificial intelligence (AI) is at the forefront of this shift.
New tools are being developed that can sift through unstructured clinical notes in electronic health records to piece together a real-time picture of a patient’s functional status.
By catching subtle descriptions of a patient’s condition buried in a doctor’s notes—things like "more tired this week" or "difficulty climbing stairs"—these systems can flag potential declines far earlier than a scheduled visit might. This allows care teams to make faster, more informed adjustments to treatment or supportive care. As this area grows, tools like a Medical Scribe AI are also helping ensure those crucial details are captured accurately in the first place.
This isn't just theory. A 2023 study showed that machine learning models could determine ECOG scores directly from physician notes with impressive accuracy. This is a big deal because it helps automate a manual, sometimes inconsistent process, paving the way for more reliable and powerful analysis of patient outcomes across thousands of records.
The evolution of patient assessment is moving toward a more complete and real-time understanding of patient health. By integrating AI and analyzing electronic health data, oncology teams can build a more responsive and personalized care experience.
This technological leap goes hand-in-hand with the growing movement to include the patient's own voice more directly in their care. Our guide on implementing patient-reported outcomes explains how your direct feedback is becoming a vital part of the treatment puzzle.
Together, these advancements are shaping a future where care plans are based not just on periodic snapshots, but on a living, breathing understanding of your unique health journey.
How to Talk to Your Doctor About Your ECOG Status
Knowing your ECOG score is a great first step, but the real power comes from talking about it openly with your oncology team. This isn't just a one-way street; it's a partnership. You are the expert on how you feel day-to-day, and your insights give the medical team crucial information that a number on a chart simply can't capture.
This dialogue ensures your treatment plan is truly aligned with your life and what matters most to you. Coming to your appointments prepared isn't about second-guessing your doctor. It's about working together. When you can share specific details about your energy, what you can and can't do, and how you're feeling, you help paint a complete picture of your health.

Preparing for the Conversation
Before you head to your next appointment, take a little time to think about your daily life. It can be incredibly useful to keep a simple journal for a few days leading up to your visit. Just jot down notes about your energy levels and what activities you managed each day.
This simple practice turns vague feelings into concrete examples you can share. Think about tracking these key areas:
- Energy Levels: How much of the day are you up and moving around versus needing to rest? Is there a pattern?
- Daily Activities: Are you keeping up with work, household chores, or your favorite hobbies? What has changed?
- Self-Care: Are you managing personal care like bathing and dressing on your own, or do you need some help?
- Symptoms: Are things like pain, fatigue, or nausea getting in the way of what you want to do?
This kind of detailed feedback gives your oncologist the context they need to accurately assess your ECOG status and make any necessary tweaks to your care plan.
Your voice is the most important tool in your healthcare journey. Openly discussing your symptoms and limitations ensures your treatment plan is not just about fighting cancer, but about supporting your quality of life every step of the way.
Questions to Guide Your Discussion
Walking into a consultation with a few questions ready can help you feel more in control and make sure nothing gets missed. These aren't just for getting information; they're for starting a collaborative conversation about your ECOG score and what it means for you. For more ideas, check out our guide on 10 key questions to ask your oncologist.
Try starting with questions like these:
- "What is my current ECOG score, and what does that number tell you about my situation?" This helps you see things from your doctor's perspective.
- "How does this ECOG status affect the treatment options we're looking at?" This links the score directly to the path forward.
- "What can we do to help manage my symptoms and maybe improve my activity level?" This shifts the focus to proactive, positive steps you can take together.
- "If my functional status changes down the road, how might that change our treatment strategy?" This helps you prepare for what might come next.
When you take an active role in these discussions, you become a true partner in your own care. This ensures your treatment is always built around your individual needs and what's happening in your life right now.
At Hirschfeld Oncology, we believe that patient-centered care begins with listening. Dr. Hirschfeld and our team are dedicated to understanding your unique journey, using tools like the ECOG score to create personalized treatment plans that prioritize both efficacy and your quality of life. To explore your options with a compassionate team, please visit us at https://honcology.com/blog.





.png)


.png)
.png)




