Think of molecular testing as getting a detailed "user manual" for a specific cancer. Instead of just knowing where the cancer is (like the lung or colon), we get to look deep inside the tumor cells themselves. We're analyzing their DNA, RNA, and proteins to find the specific genetic glitches—or biomarkers—that are making them grow and spread.
This information is incredibly powerful. It helps us match the cancer with a treatment designed to attack its unique weak spots.
Looking Under the Hood of Cancer
Imagine your car’s engine light flashes on. A general mechanic might just say, "You've got an engine problem." But a specialist with a diagnostic computer can plug in and tell you exactly which sensor is failing.
Traditional cancer diagnosis is a bit like that general mechanic; it identifies the cancer's location and type. Molecular testing is the specialist's diagnostic tool. It looks "under the hood" to decode the cancer's unique genetic blueprint, moving us far beyond a one-size-fits-all approach.
So, instead of treating all lung cancers the same way, your oncologist can pinpoint the specific drivers of your lung cancer. These unique identifiers are the biomarkers.
Think of these biomarkers as signposts on a map of the cancer. They reveal critical details, like:
- Which genetic mutations are telling the cells to multiply nonstop.
- Whether the cancer has a weakness that a specific targeted drug can exploit.
- How visible the cancer might be to your immune system, and if it could respond to immunotherapy.
By reading these signposts, your oncology team can craft a much more precise and effective treatment strategy. This fundamental shift toward personalized care is the whole idea behind precision oncology. You can learn more about how this works in our detailed guide on what is precision oncology.
This detailed, molecular-level view has become an essential part of modern cancer care, especially for advanced or complex cases. The medical community’s growing reliance on it is clear from the numbers. The global market for oncology molecular diagnostics was valued at around $3.59 billion in 2023 and is expected to hit $6.35 billion by 2030. This growth is driven by the urgent need for better treatments, with nearly 20 million new cancer cases reported worldwide in 2022 alone, as detailed in this oncology molecular diagnostics market report.
To really grasp the difference this makes, let’s compare the old way of thinking with this new, personalized approach.
Traditional vs. Molecularly-Guided Cancer Care
The table below breaks down the core differences between the standard "one-size-fits-all" model and the modern, biomarker-driven strategy we use today.
Ultimately, molecular testing allows us to move from a general strategy to a highly specific one, giving us a much better chance to find a treatment that works for you.
How We Decode Your Cancer’s Unique Blueprint
To find out what makes your cancer tick, your oncology team needs to get a closer look at the tumor itself. Think of it as gathering intelligence on an enemy—we need a sample to understand its weaknesses. This is the first and most crucial step in molecular testing.
Typically, we get this sample in one of two ways.
The most common method is a tissue biopsy. This is a straightforward procedure where a surgeon or radiologist removes a tiny piece of the tumor. This solid tissue gives us a rich, detailed snapshot of the cancer's genetic makeup and protein activity at that moment.
But sometimes, a tissue biopsy just isn't practical. The tumor might be in a difficult-to-reach spot, or it might not be safe for the patient. That’s when we can turn to an incredible alternative: a liquid biopsy.
The Power of a Simple Blood Draw
A liquid biopsy is exactly what it sounds like—a test run on a simple blood sample. As cancer cells grow and die, they shed tiny fragments of their DNA into the bloodstream. We call this circulating tumor DNA (ctDNA), and we can capture and analyze it.
This method is far less invasive than a traditional biopsy. And because it's just a blood draw, we can do it more often. This allows us to track how the cancer is changing over time, see if a treatment is working, or spot new mutations if the cancer becomes resistant, all without another procedure.
This flowchart shows how molecular testing bridges the gap between diagnosis and a highly specific treatment plan.
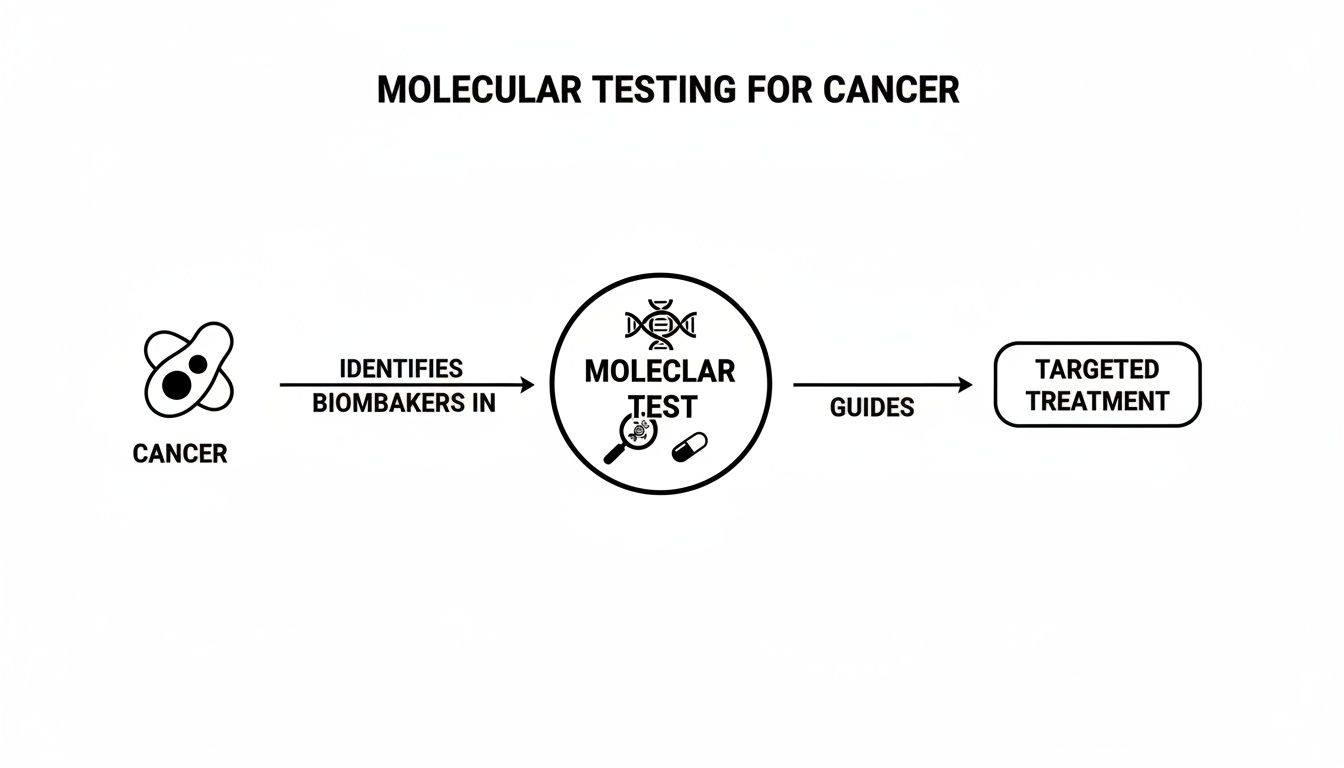
As you can see, the test results are the key that unlocks a more precise, personalized therapy.
Once we have a high-quality sample—whether from tissue or blood—it goes to a specialized lab. There, scientists use powerful technologies to read the tumor's molecular code. It's a bit like this: a simple test might look for a single typo in a book, while the more advanced methods can scan an entire library at once for any and all errors.
The Technologies That Find The Clues
There isn’t just one type of molecular test. Several different technologies can be used to analyze a cancer sample, and each is designed to find different kinds of molecular clues. Your care team will choose the best method based on your cancer type and the specific information needed to guide your treatment.
Here’s a quick look at the most common testing methods and what they do.
These highly advanced technologies are all designed to find biomarkers—the molecular "flags" that can make a cancer vulnerable to specific drugs.
For example, a test might find an EGFR mutation in lung cancer, a BRAF mutation in melanoma, or an overabundance of the HER2 protein in breast cancer. Each of these findings points us directly to a targeted therapy designed to attack that very abnormality.
Choosing the right technology is key. While a focused test like PCR is fast and efficient, a broad panel using Next-Generation Sequencing (NGS) gives us a much more complete picture. For many cancers, NGS is the gold standard because it casts a wider net, which means we’re much more likely to find an actionable target that a smaller test might miss.
To learn more about this powerful approach, check out our guide on how Next-Generation Sequencing is used in clinical decision-making for cancer care.
Ultimately, the goal is to translate your tumor's complex biology into a clear, effective treatment plan. By identifying the exact molecular drivers of your cancer, we can move beyond one-size-fits-all treatments and design a strategy just for you.
Turning Test Results Into a Treatment Plan

A molecular test report isn't just a page of data; it's a strategic map. This is where the science of genomics gets personal, connecting the dots between your tumor’s specific biomarkers and the most powerful therapies we have today.
For many of our patients, this detailed molecular blueprint opens the door to two of the most important advances in modern cancer care: targeted therapy and immunotherapy. Each one uses your test results in a completely different way to outsmart cancer, moving far beyond the one-size-fits-all approach of traditional chemotherapy.
This is the whole point of molecular testing—it helps us find a smarter, more direct, and often less toxic path forward in your treatment.
Locking On with Targeted Therapy
Think of your cancer cells as having a unique lock on their surface that healthy cells don’t. This lock is a specific protein, created by a mutated gene, that’s stuck in the “on” position, telling the cancer to grow and divide nonstop.
Targeted therapy is like a custom-made key, designed to fit that one specific lock.
When the drug—the “key”—finds its matching protein “lock,” it can do one of two things:
- Block the Signal: It can jam the lock, stopping the growth signal from ever getting inside the cell.
- Deliver a Payload: It can be used to carry a cancer-killing substance directly to the cell, leaving healthy cells alone.
This incredible precision is why targeted therapies can be so effective while often having fewer of the widespread side effects we see with traditional chemo, which attacks all fast-growing cells, healthy or not.
A molecular test report is what identifies these specific locks. For instance, if a patient with non-small cell lung cancer has an EGFR mutation, we know they may be a candidate for a drug like osimertinib, which is built to block that exact EGFR protein. Without the test, we'd be flying blind.
The Key and Lock Principle: Think of molecular testing as a locksmith who tells us the exact type of lock on a door. Targeted therapy is the custom-made key that fits perfectly. Traditional chemotherapy is more like using a sledgehammer to knock the door down—it might work, but it causes a lot of collateral damage.
Activating the Immune System with Immunotherapy
While targeted therapy hones in on the cancer cell's internal wiring, immunotherapy takes a completely different angle. It focuses on your body's own defense system—your immune cells—and essentially teaches them how to recognize and destroy cancer.
Cancer cells are notoriously sneaky. They often find ways to hide from the immune system by putting up a "don't see me" sign. This sign is a protein called PD-L1. When your immune cells see it, they get the message to back off, leaving the cancer free to grow.
Molecular testing, specifically an IHC test, can measure the amount of PD-L1 on your tumor cells.
- High PD-L1 Levels: If your cancer has a lot of this protein, it tells us the tumor is actively cloaking itself from your immune system. This is often a huge clue that an immunotherapy drug, called a checkpoint inhibitor, will work well.
- Checkpoint Inhibitors: These drugs work by blocking that PD-L1 signal. They effectively rip off the cancer’s invisibility cloak, allowing your immune system to finally see the cancer cells as a threat and go on the attack.
Other biomarkers like Microsatellite Instability (MSI-H) and Tumor Mutational Burden (TMB) are also crucial for immunotherapy. A high TMB, for example, means the cancer has a lot of mutations, creating more abnormal proteins that look like red flags to the immune system. The more flags there are, the easier it is for your immune cells to find their target once we’ve unleashed them with immunotherapy.
From Biomarker to Bedside: A Real-World Example
Let's walk through a real-world scenario. A patient with advanced colorectal cancer gets a comprehensive Next-Generation Sequencing (NGS) panel on their tumor tissue. The report comes back with a game-changing finding: the tumor has a BRAF V600E mutation.
This single piece of information changes everything about their treatment plan.
- Avoid Ineffective Drugs: We know from experience and data that certain standard chemo drugs just don't work well against BRAF-mutated colorectal cancer. The molecular test stops us from wasting precious time on a treatment that's unlikely to help.
- Select a Targeted Combination: The BRAF V600E mutation is a known "lock." The result points us directly to a combination of targeted drugs, like encorafenib (a BRAF inhibitor) and cetuximab (an EGFR inhibitor), which work in tandem to shut down the cancer's growth signals.
- Identify Clinical Trial Options: If standard therapies aren't an option or eventually stop working, that BRAF mutation could make the patient eligible for clinical trials testing new drugs designed for this exact molecular subtype.
This is personalized medicine in action. The test result isn't just a finding; it's an actionable instruction that guides every decision we make. Truly understanding the role of genomic testing in developing personalized treatment plans is central to seeing how this data shapes a patient's entire cancer journey by giving your oncologist a clear, evidence-based roadmap.
Navigating the Practical Side of Molecular Testing

Knowing the science is one thing, but figuring out the real-world details of molecular testing is another beast entirely. For patients and their families, practical questions about timing, cost, and the actual process are usually front and center. Pulling back the curtain on these steps can help ease a lot of the anxiety and set clear expectations for your care.
We want to give you a transparent, straightforward look at what this part of the journey involves. From the moment we order the test to the day we sit down to go over the results, our team at Hirschfeld Oncology is here to guide you, making sure you feel informed every step of the way.
Understanding Test Timelines
One of the first questions we always get is, "How long until I have the results?" That waiting period can feel like an eternity, so it helps to know what goes into the timeline.
For a comprehensive Next-Generation Sequencing (NGS) panel, you can generally expect the results to take between two to four weeks. It's important to remember that this clock starts after the specialized lab has your tissue or blood sample in hand.
A few things can affect that turnaround time:
- Test Complexity: A simple test looking for a single gene might be quick. But a broad panel that analyzes hundreds of genes requires a lot more time for the actual sequencing and, just as importantly, for the complex data analysis that follows.
- Sample Quality: Before anything else, the lab has to confirm your sample contains enough good-quality DNA to produce a reliable result. If the sample isn't adequate, we might need a new one, which can, unfortunately, add to the timeline.
- Lab Volume: Just like any other facility, the lab’s current workload can influence how quickly they can process your test.
We partner with top-tier labs to keep things moving as efficiently as possible. Our team will keep you in the loop and schedule a specific appointment to discuss your results with you the moment they’re ready.
Navigating Cost and Insurance Coverage
The cost of molecular testing is, understandably, a major concern for many families. The good news is that coverage has improved significantly over the past few years. Most insurance plans, including Medicare, now cover this type of testing for patients with advanced cancers when it's medically necessary to guide treatment.
That said, the world of insurance can be tricky to navigate. A crucial step called pre-authorization is almost always required before the test is run. This is where our team formally submits the medical justification to your insurer to get their official approval for coverage.
We firmly believe that financial stress shouldn't stand in the way of getting the best care. Our team at Hirschfeld Oncology is deeply experienced in managing the pre-authorization process and will work tirelessly on your behalf to secure the coverage you need.
If you do run into high out-of-pocket costs or a coverage denial, don't lose hope. Many of the testing companies offer excellent patient assistance programs. These programs can dramatically reduce or sometimes even eliminate the cost for patients who qualify, and we can help you find and apply for them.
When Is the Right Time to Test and Retest?
Deciding when to perform molecular testing is a strategic part of your overall treatment plan. It’s a decision your oncologist makes based on your specific cancer diagnosis and where you are in your treatment journey.
For many patients diagnosed with advanced or metastatic cancer, we'll order a comprehensive test right from the start. This gives us a foundational blueprint of the tumor’s genetic drivers, which helps us pick the most effective first-line therapy right out of the gate.
But cancer is a moving target. It can change and adapt, especially when it’s being treated. A therapy that works beautifully for a while might eventually stop being effective because the cancer has developed new mutations to survive. We call this acquired resistance.
When that happens, it’s often the right time to test again. This re-test is frequently done with a less invasive "liquid biopsy," which is just a simple blood draw. This test can spot new mutations that have popped up, giving us the critical clues we need to switch to a different targeted therapy or explore a new clinical trial. This kind of ongoing molecular monitoring helps us stay one step ahead of the cancer.
Finding Hope With Advanced Oncology Care
All this groundbreaking science translates into something deeply personal and powerful: your individual cancer journey. At Hirschfeld Oncology, we see comprehensive molecular testing not just as another diagnostic tool, but as the very foundation of how we care for our patients. This is the moment where abstract data becomes a clear, actionable plan built just for you.
Our commitment is to leave no stone unturned. For patients with tough-to-treat cancers—like pancreatic, cholangiocarcinoma, and colorectal cancers—these molecular insights give us a critical strategic advantage. Think of it as a detailed blueprint of the tumor; it often reveals treatment avenues that standard protocols might miss, creating new possibilities even when other options seem exhausted.
Your Journey With Hirschfeld Oncology
Your first conversation with Dr. Hirschfeld's team is exactly that—a conversation. We'll sit down to discuss your diagnosis, listen carefully to your goals, and explain how a deep molecular dive can light up the best path forward. We firmly believe in making decisions with you, not for you.
Here’s what you can expect when you partner with us:
- Initial Consultation: We’ll talk through whether molecular testing is the right next step and which type of test—from a comprehensive tissue biopsy to a less invasive liquid biopsy—makes the most sense in your situation.
- Collaborative Review: Once your results are back, we schedule a dedicated appointment to walk through the report together. We make it a priority to translate the dense scientific language into clear, understandable terms, explaining exactly what each biomarker means for your treatment options.
- Building Your Plan: Armed with these insights, we build your personalized treatment plan side-by-side. This could mean starting a targeted therapy, considering immunotherapy, or identifying a promising clinical trial that's a perfect match for your tumor’s specific molecular profile.
At Hirschfeld Oncology, a molecular test report isn’t the end of a process; it's the starting point of a hopeful, new chapter. It’s our way of ensuring that your treatment is as unique as you are, guided by the most precise science available today.
We specialize in finding paths forward where others might see roadblocks. By truly understanding what makes your cancer tick, we can move beyond one-size-fits-all care to find a strategy that maximizes effectiveness while minimizing side effects, always keeping your quality of life at the forefront. This isn’t just about advanced oncology; it’s about restoring hope.
If you or a loved one is facing a complex cancer diagnosis and want to explore how molecular insights can create new opportunities, we invite you to request a consultation with our team. Let’s discover your path forward, together.
Your Questions Answered: The Practical Side of Molecular Testing
Stepping into the world of molecular testing naturally brings up a lot of practical questions. It’s one thing to understand the science, but it’s another to know what to expect from the process itself. We’ve put together answers to some of the most common questions we hear from patients and their families to help you feel more prepared and confident.
Knowing the logistics of timing, cost, and what the results mean is a huge part of your care. Getting these questions answered can lift a weight off your shoulders, letting you focus on your treatment and well-being. Our goal is to make every step clear.
Will My Insurance Cover Molecular Testing for My Cancer?
This is usually the first question on everyone's mind, and for good reason. The great news is that insurance coverage for molecular testing has gotten much, much better over the years. Today, most major insurers, including Medicare, will cover comprehensive testing for advanced solid tumors when it’s medically necessary to guide treatment decisions.
That said, the exact details always come down to your specific insurance plan, the type of cancer you have, and its stage. Before we run any tests, we almost always have to complete a pre-authorization. This is a critical step where our team sends all the medical reasons for the test to your insurance company to get their official approval.
At Hirschfeld Oncology, our team is incredibly skilled at managing this process. We take care of the entire pre-authorization for you, working directly with your insurer to get the green light for the testing you need.
If your insurance happens to deny coverage or you're left with a high out-of-pocket cost, don't worry—there are other avenues. Many of the testing labs and several non-profit foundations offer financial assistance programs. We can help you find and apply for these resources to help ease any financial strain.
How Is This Different From Genetic Testing for Inherited Cancer Risk?
This is a fantastic and very important question. It gets to the heart of a key difference in cancer genetics. While both types of tests look at your genes, they’re looking for different kinds of information for completely different purposes.
- Molecular Testing (Somatic/Tumor Testing): This is all about analyzing the cancer cells themselves. We’re hunting for genetic mutations that the cancer developed as it grew and evolved. These are not mutations you were born with, and you can't pass them on to your children. The one and only goal here is to find targets for your treatment.
- Inherited Risk Testing (Germline Testing): This test looks at your normal, healthy cells, usually from a simple blood draw or saliva sample. It’s designed to find gene mutations you inherited from a parent, like the well-known BRCA1/2 mutations. Finding one of these means you have a higher lifetime risk for certain cancers.
Here’s a simple way to think about it: Molecular tumor testing is like a snapshot of your tumor’s DNA right now, giving us a road map for immediate treatment. Germline testing is about understanding the genetic hand you were dealt at birth and what it means for your long-term health. Occasionally, a finding from a tumor test might give us a clue that an inherited risk exists, which might lead us to recommend germline testing to confirm.
What Happens If My Test Shows No Actionable Mutations?
It’s definitely possible for a comprehensive molecular test to come back without any specific "actionable" mutations that match a currently available targeted drug or immunotherapy. Hearing this can feel like a letdown, but I want to be very clear: this result is still incredibly valuable for your treatment plan.
First off, it tells us a lot through the process of elimination. It lets your oncologist know which treatments, like certain targeted therapies, are unlikely to be effective. This is huge. It saves you precious time and protects you from the side effects of a drug that was never going to work for you in the first place.
A "negative" result like this helps us confidently steer your treatment toward other proven options that don't depend on a specific biomarker, such as certain types of chemotherapy. What's more, cancer medicine is moving forward at an unbelievable speed. A biomarker with no matching drug today could have one tomorrow. Having your tumor's full molecular profile on hand means we’re always ready, constantly watching for new breakthroughs or clinical trials that might be a perfect fit for you down the road.
How Long Does It Take to Get Molecular Testing Results Back?
The wait for results can be one of the most stressful parts of this process, so knowing what to expect is important. The exact turnaround time depends on the specific test being run and the lab doing the work.
In general, you can expect results from a comprehensive Next-Generation Sequencing (NGS) panel to take about two to four weeks. That clock starts ticking once the lab has your tissue or blood sample in hand and has confirmed it's good enough quality to analyze.
Simpler tests that look for just one or two genes, like a PCR test, are often faster, sometimes coming back in one to two weeks. We know how tough this waiting period is. At Hirschfeld Oncology, we only work with high-quality, efficient labs and we promise to keep you in the loop. The moment we have your results, we will set up a dedicated appointment to go over them with you, line by line, so you know exactly what they mean for you.
At Hirschfeld Oncology, we see these detailed molecular insights as the start of a hopeful, new chapter in your care. If you want to explore how a personalized, data-driven approach can open up new possibilities, we invite you to learn more at Hirschfeld Oncology's Blog.





.png)


.png)
.png)




