When a cure for cancer is no longer the primary focus, the treatment strategy shifts. That’s where palliative chemotherapy comes in. It’s a specialized approach that uses cancer-fighting drugs not to eliminate the disease, but to control it—managing symptoms and improving your overall quality of life.
The goal is to give you more comfort, more energy, and more meaningful time. It's about prioritizing your well-being above all else.
Shifting Focus From A Sprint To A Marathon

When most people hear "chemotherapy," they think of an all-out, aggressive fight against cancer. But what happens when the game plan changes from a short, intense sprint to a thoughtfully paced marathon? This analogy gets to the heart of palliative chemotherapy. It’s not about giving up. It’s about adapting to a new reality where endurance and daily well-being become the true measures of success.
The word "palliative" itself can be a source of confusion. It simply means to relieve symptoms and stress. This philosophy of care can be applied at any point during a serious illness and is very different from end-of-life care. Taking a moment to understand the key differences between palliative care and hospice care is essential for making clear, informed decisions.
Prioritizing Your Quality Of Life
The main objective here is to manage the cancer in a way that’s sustainable, allowing you to live as comfortably as possible. This involves using treatments designed to shrink tumors, ease pain, reduce fatigue, and help you keep up your strength and appetite.
Ultimately, the goal is to give you more good days—time to spend with family, enjoy your hobbies, and live life on your own terms.
The decision to pursue palliative chemotherapy is a proactive choice to prioritize comfort and control. It redefines winning as living better, not just fighting harder, by aligning medical treatment with personal life goals.
A Look At The Evidence
This approach has a real, measurable impact on both the quality and length of a person's life. A key study on patients with metastatic colorectal cancer, for example, found that those receiving palliative chemotherapy had a median overall survival of 12.4 months.
This was a significant improvement compared to the 5.3 months for those who only received the best supportive care. It’s a powerful illustration of how this strategic treatment can offer incredibly valuable time.
To make the distinction crystal clear, here’s a quick comparison of the two approaches.
Palliative Chemotherapy At A Glance
This table breaks down the core differences between chemotherapy aimed at palliation versus a cure.
As you can see, the entire philosophy is different. One is about total victory over the disease, while the other is about mastering the art of living well with it.
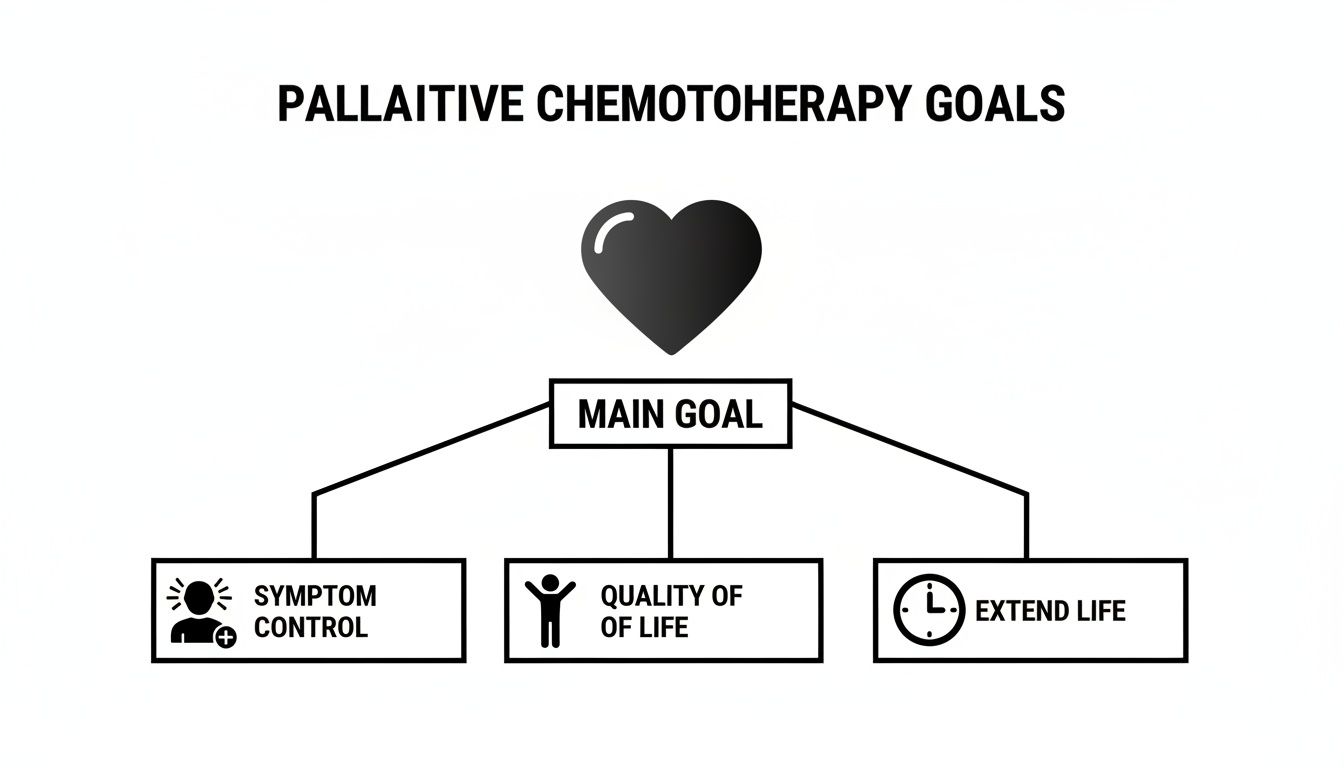
What Palliative Chemotherapy Really Aims to Achieve
When we talk about palliative chemotherapy, the first thing to understand is that we’re shifting the goalposts. Success isn’t measured by whether we can eliminate every last cancer cell. Instead, we measure it by how much we can improve your life, right now. The entire approach is built on three core ideas, and all of them revolve around you.
This isn’t a choice between "fighting" the cancer and giving up. It’s about finding a smarter, more sustainable way to live with it. The treatment plan is designed to serve your life, not the other way around. Let's break down what that really means.
Getting Symptoms Under Control
One of the most immediate and tangible goals is simply to help you feel better. Advanced cancer often comes with a heavy physical burden—things like constant pain, shortness of breath, or a deep, persistent fatigue that can make it hard to just get through the day. Palliative treatment can make a real difference here.
For example, a tumor pressing on a nerve can be a source of relentless pain. A carefully chosen chemotherapy regimen can shrink that tumor just enough to take the pressure off, providing relief without relying solely on high-dose painkillers that can leave you feeling groggy.
The same goes for a tumor near your lungs that makes every breath a struggle. By reducing its size, we can help you breathe more easily, restoring a fundamental sense of comfort and freedom. The objective is to manage the cancer's impact so you can get back to your daily life.
Protecting Your Quality of Life
Beyond just knocking back symptoms, palliative chemotherapy is all about protecting your overall quality of life. Now, that term means something different to everyone. It’s about having the energy, independence, and ability to do the things that matter most to you.
What does a good day look like? Is it having dinner with family? Spending time in your garden? Or just having the strength to read a book without feeling wiped out? Your treatment plan should be built around your answers to those questions.
"Our Supportive Cancer Care Program is about helping patients balance the side effects of treatment with day-to-day living, so that they can continue doing the activities that bring them joy with the people with whom they love."
This means we’re very deliberate about the drugs we choose, the dosages we use, and the schedule we follow. The goal is to keep the cancer under control in a way that doesn't make the treatment feel worse than the disease itself.
Gaining More Meaningful Time
The third goal, which is deeply connected to the first two, is extending life. But it's crucial to understand what we mean by that. We’re focused on adding meaningful time. Palliative chemotherapy can slow down the cancer's growth, often giving people months or even longer than they would have had otherwise.
This isn’t just about marking more days on a calendar. It's about creating more opportunities for the moments that count:
- Being there for a grandchild's graduation or a family wedding.
- Finishing a project you care about or taking a trip you’ve always wanted.
- Simply having more time for conversations and memories with the people you love.
This extra time is only truly valuable when your symptoms are managed and you feel well enough to enjoy it. By keeping the disease stable, palliative chemotherapy can open up a window to live more fully, on your own terms. That’s the principle that guides every decision we make.
How Palliative Chemotherapy Is Different In Practice
Knowing the goals of palliative chemotherapy is one thing, but what does it actually look like day-to-day? The experience is often a world away from the aggressive, high-intensity regimens used when a cure is the objective. It’s less about an all-out assault on the cancer and more about a strategic, sustainable way to manage it as a chronic condition.
Think of it like tuning a high-performance engine. Instead of redlining it for a short, powerful burst—which inevitably causes major wear and tear—you’re calibrating it for a smooth, efficient, and reliable long-distance journey. This practical shift shows up in everything from the dosage of the drugs to how often you come into the clinic.
Rethinking Dosage And Treatment Schedules
One of the biggest practical differences is the dosage of chemotherapy. In a curative setting, the idea is to hit the cancer with the maximum tolerated dose to wipe out as many cancer cells as possible. Palliative chemotherapy completely flips that script.
Here, the focus is on finding the minimum effective dose—just enough to keep the tumor in check, relieve symptoms, and keep side effects from taking over your life. This often means using lower doses of the same drugs or spreading them out over more time.
This approach is all about balancing the treatment’s benefits with its impact on your well-being.
As you can see, every practical decision—especially about dosage and frequency—is guided by the primary goals of controlling symptoms and giving you more quality time.
Treatment schedules are also tailored to fit your life, not the other way around. Instead of intense cycles every two or three weeks that leave you drained, a palliative schedule might involve less frequent infusions or even oral medications you can take at home. The whole plan is designed for better tolerance, meaning fewer interruptions to your daily routine and more time spent living your life.
To make these distinctions even clearer, let's break down how the two approaches stack up side-by-side.
Palliative Vs Curative Chemotherapy Key Differences In Approach
This table breaks down the practical differences in treatment philosophy, dosage, scheduling, and side effect management.
Ultimately, these differences highlight a fundamental shift in mindset from fighting a battle at all costs to thoughtfully managing a long-term condition.
Proactive Management Of Side Effects
With curative chemo, harsh side effects are often accepted as a necessary evil in the fight to eradicate the cancer. But in palliative care, minimizing those side effects isn't an afterthought—it's a central goal of the treatment itself. The philosophy is simple: the treatment shouldn't feel worse than the disease.
Your oncology team will work ahead of the curve to manage potential issues before they become serious. This includes things like:
- Pre-medication: Giving you anti-nausea drugs before an infusion even starts.
- Supportive Therapies: Recommending gentle exercise, nutritional guidance, or other strategies to fight fatigue and keep you strong.
- Constant Monitoring: Checking in regularly to adjust medications or offer support at the very first sign of a problem.
This focus on proactive management helps protect your energy and comfort, ensuring the treatment adds to your quality of life rather than taking away from it.
Measuring Success Differently
Finally, the very definition of "success" changes. Instead of focusing only on what a scan shows, success in palliative care is defined by your personal experience and what matters most to you.
The important questions become the new metrics:
- Is your pain under better control?
- Do you have more energy to do the things you enjoy?
- Are you able to eat and actually enjoy your meals?
- Are you spending meaningful time with the people you love?
For stage IV cancers, this approach is the foundation of modern care. In fact, it's the primary therapy for metastatic disease in 64% of cases. Its importance is backed by research showing it can increase median overall survival from about 5 months with only supportive care to over 12 months with palliative treatment, giving patients invaluable time. You can read the full study to learn more about the impact of palliative treatment on survival rates.
This redefinition of success ensures that every decision is aligned with the ultimate goal: living as well as you can, for as long as you can.
Modern, Personalized Palliative Treatments
The world of palliative care has changed dramatically. It's no longer about a one-size-fits-all approach but represents the leading edge of personalized cancer medicine. We're using advanced science to find smarter, gentler ways to manage complex cancers, creating treatment plans that are as unique as the person they’re designed for.
The goal is to find treatments that are both effective and tolerable. Modern therapies work by targeting the specific vulnerabilities of cancer cells, which minimizes the collateral damage to healthy tissue. This is the very principle that makes palliative chemotherapy a sustainable, long-term strategy.
Let’s look at a few of the most important approaches we use today.
Low-Dose Metronomic Chemotherapy
Think of it like tending a garden. Instead of blasting it with a harsh pesticide once a month that kills everything in sight, you could use a gentle, continuous fertilizer that helps your plants thrive while slowly starving out the weeds. That’s the basic idea behind metronomic chemotherapy.
Instead of hitting the body with high-dose infusions every few weeks, this approach uses low doses of chemotherapy drugs much more frequently—sometimes even daily. This steady, low-level pressure accomplishes two key things:
- It cuts off the tumor's supply lines. Metronomic chemo is fantastic at disrupting the growth of new blood vessels that tumors need to grow and spread (a process called anti-angiogenesis).
- It keeps the cancer in check. The constant presence of the drug prevents cancer cells from regrouping and repairing themselves, holding the disease stable with far fewer side effects.
This turns chemotherapy from a short-term assault into a manageable, long-term control strategy, allowing many of our patients to carry on with their lives without major disruptions.
Targeted Therapies: The Smart Keys of Cancer Care
If traditional chemotherapy is a master key that crudely forces many locks, targeted therapies are smart keys cut for one specific lock. Every cancer has a unique genetic signature—specific proteins or mutations that fuel its growth. Targeted drugs are engineered to find and block those exact targets.
For instance, a drug might be designed to shut down a very specific growth signal that’s stuck in the "on" position in your particular cancer cells. By flipping that switch off, it stops the cancer from growing without harming healthy cells that don’t rely on that signal.
This level of precision is why targeted therapy has become a cornerstone of modern palliative care. It offers powerful cancer control with a much smaller impact on your overall well-being, which perfectly aligns with our goal of preserving your quality of life.
Of course, this approach depends on detailed genetic testing of your tumor to find out which "smart keys" might fit. When we find a match, the results can be truly game-changing.
Harnessing Your Immune System with Immunotherapy
Another incredible tool in our palliative toolkit is immunotherapy. This treatment is different because it doesn't attack the cancer directly. Instead, it unleashes your own immune system, essentially taking the brakes off so it can recognize and destroy cancer cells on its own.
Imagine your immune system is a security team that has been fooled by cancer cells wearing a disguise. Immunotherapy drugs work by ripping off that disguise, allowing your body’s natural defenses to finally see the threat and go on the attack.
We can also combine immunotherapy with other treatments, like low-dose chemo or targeted drugs, to create a powerful, multi-faceted attack. For many patients, this strategy can lead to durable, long-term disease control, opening up another path to extending meaningful time while feeling well. These modern strategies show that palliative chemotherapy isn't about giving up—it's about getting smarter.
Making The Right Decision For You
Deciding on a treatment path for advanced cancer is a profoundly personal journey. There's no single "right" answer, and it’s certainly not a one-size-fits-all prescription. Think of it as a collaborative process where your voice, your values, and your vision for your life are the most important part of the conversation.
This is a decision made by a team, and you are the team captain. You, your family, and your oncology team will work together to map out a plan that genuinely makes sense for you. It’s about so much more than medical charts and scan results; it's about making sure your treatment supports the life you want to live.
Key Factors In Your Decision
To create the best possible plan, we need to bring several critical pieces of the puzzle together. This shared understanding ensures every choice is informed, thoughtful, and, most importantly, respects what you want.
The main considerations usually boil down to these:
- Your Specific Cancer: We'll look at the type of cancer, where it started, where it has spread, and its unique genetic markers. This is the technical side of things that helps us pinpoint which treatments are most likely to work.
- Your Overall Health: How are you feeling in general? Your strength, energy levels, and any other health conditions you're managing are crucial factors. This helps us gauge how well you might handle different therapies.
- Your Personal Goals: This is the most important piece of all. What do you want to achieve? What makes a day a "good day" for you? Being crystal clear about your priorities is what guides everything else.
Your Voice Is The Guiding Force
The entire decision-making process is built around what you value. There are no right or wrong answers here, only what is right for you. Your oncologist's job is to lay out the options, clearly explain the potential upsides and downsides of each, and help you weigh them against what matters most in your life.
The best treatment plan is one that not only manages the cancer but also supports your life. It’s about empowering you to make choices that honor your wishes, ensuring your care aligns with your definition of living well.
Thinking through these things ahead of time can help you feel more prepared and confident during these important conversations. To help you get started, we've put together a resource with 10 key questions to ask your oncologist.
How Global Guidelines Influence Your Care
Your oncologist’s recommendations don't exist in a vacuum; they are informed by established international standards. Global guidelines from respected organizations like the World Health Organization (WHO) and the National Comprehensive Cancer Network (NCCN) provide a strong foundation for palliative chemotherapy decisions.
For example, the 2023 WHO Essential Medicines List endorses 64 therapies, and 73% of those align with NCCN recommendations. The reality, however, is that access varies. With only 39% of countries including basic cancer care in universal health coverage and just 28% including palliative care, having expert guidance is absolutely vital.
This is why working with an experienced oncologist who can navigate all the available options is so important. They can help create a plan that is truly personalized for you, not just based on a generic checklist.
Ultimately, this collaborative journey is about making sure you have the information, support, and power to choose a path forward that feels right. Your oncologist is your partner, here to provide expertise and guidance, but you are the one who sets the course for your care.
Finding A Partner In Your Cancer Care

Navigating a diagnosis of advanced cancer isn't just about medicine; it's about finding a true partner for the journey ahead. You need an oncology team that sees the whole person, not just the disease, and is deeply committed to making sure your treatment plan actually fits your life.
The best palliative chemotherapy plans are always built on a solid foundation of trust, open communication, and shared decisions. The right team makes your quality of life the top priority, focusing on effective, low-toxicity strategies that help you feel as good as possible, for as long as possible.
What A Supportive Environment Looks Like
A truly patient-centered practice is designed completely around your comfort and well-being. This philosophy extends far beyond the treatment chair, creating an environment where you feel seen, heard, and genuinely cared for from the moment you arrive.
So, what does that support actually feel like?
- Proactive Symptom Management: Your team should be working with you to get ahead of side effects, not just react to them. The goal is to manage them before they escalate so you can maintain your energy and keep doing the things you love.
- A Comfortable Setting: An infusion center that feels calm and peaceful can make a world of difference during treatment, helping to reduce the natural stress and anxiety that comes with it.
- An Accessible Team: You should always feel like you can reach your team—the doctors, nurses, and coordinators who are there to offer guidance and emotional support every step of the way.
Choosing your oncology team is one of the most critical decisions you will make. This is the group of people who will help you chart a course forward, providing clarity, hope, and personalized care when it matters most.
Taking The Next Step With Confidence
Learning about your options is the first step, but taking action is where your power lies. Getting a consultation or a second opinion is a powerful way to make sure you've explored every possible path, especially with a practice that specializes in today's more advanced palliative treatments.
At Hirschfeld Oncology, providing this exact level of personalized, compassionate care is what we do. Our entire approach is built on using effective, low-dose regimens, targeted therapies, and immunotherapy to help our patients live better and longer. We believe in creating a supportive partnership that honors your goals and gives you a clear path forward.
If you're trying to understand what palliative chemotherapy could mean for you or someone you care about, we invite you to request a consultation. Let's talk about your options and find a plan that restores hope and puts your quality of life first.
Common Questions About Palliative Chemotherapy
Starting a conversation about palliative chemotherapy can feel overwhelming, and it’s natural to have questions. Getting clear, honest answers is the first step toward feeling confident in your decisions. Let's walk through some of the things that are most often on the minds of patients and their families.
Does Choosing Palliative Chemotherapy Mean I Am Giving Up?
Not at all. In fact, this is one of the biggest myths we hear, and it couldn't be further from the truth. Making this choice is a powerful, proactive step toward taking control of your cancer journey. It’s not about stopping the fight; it’s about changing the strategy.
Instead of focusing solely on eliminating the cancer at all costs, the goal shifts to controlling it so you can live as well as possible, for as long as possible. It's about making your comfort, your energy, and your ability to spend meaningful time with loved ones the top priority.
Will I Be Sick All The Time From The Side Effects?
A central goal of palliative chemotherapy is to keep side effects to a minimum. This is a key difference from more aggressive, curative treatments. The doses are often lower, and the schedules are designed to be much gentler on your body. The whole point is to improve your quality of life, not take away from it.
Your oncology team will be your partner in this, working to stay one step ahead of any potential side effects. The guiding principle is simple: the treatment should not be worse than the disease.
While side effects can still happen, they are almost always manageable with supportive medications and other approaches. You can learn more by reading our guide on managing the side effects of cancer treatment.
How Long Can Palliative Chemotherapy Extend My Life?
This is a deeply personal question, and there's no one-size-fits-all answer. How much time a treatment might add depends on a few key things:
- The type and stage of your cancer.
- Your overall health and personal resilience.
- How well the cancer responds to the specific drugs.
Research shows that for many people, palliative chemotherapy can add months, and sometimes longer, to their lives compared to supportive care alone. But the real goal is always to add quality time—not just more days, but better days. Your oncologist can talk through what's realistic for your specific situation, helping you weigh the potential benefits against your personal goals.
At Hirschfeld Oncology, we believe in building a partnership with you that honors your wishes and priorities. If you are weighing your treatment options, we invite you to request a consultation on our website to explore a plan that restores hope and puts your quality of life first.





.png)


.png)
.png)




