When your first cancer treatment stops working, or the cancer comes back, your oncology team will talk about the next steps. This is often when the term salvage chemotherapy comes up. It’s not a sign of failure; it’s a strategic pivot—a new game plan designed to get the cancer back under control.
What is Salvage Chemotherapy?
Hearing that your first treatment isn’t working anymore is tough. The term "salvage chemotherapy" can sound a little jarring, but it’s best to think of it as your medical team’s Plan B.
Think of it like a coach in a championship game. If the first play doesn't work, the coach doesn't just throw in the towel. They switch things up. They send in a new set of players with a different strategy to attack the opponent from a new angle. That’s exactly what salvage chemotherapy is—a smart, adaptive response to a changing situation.
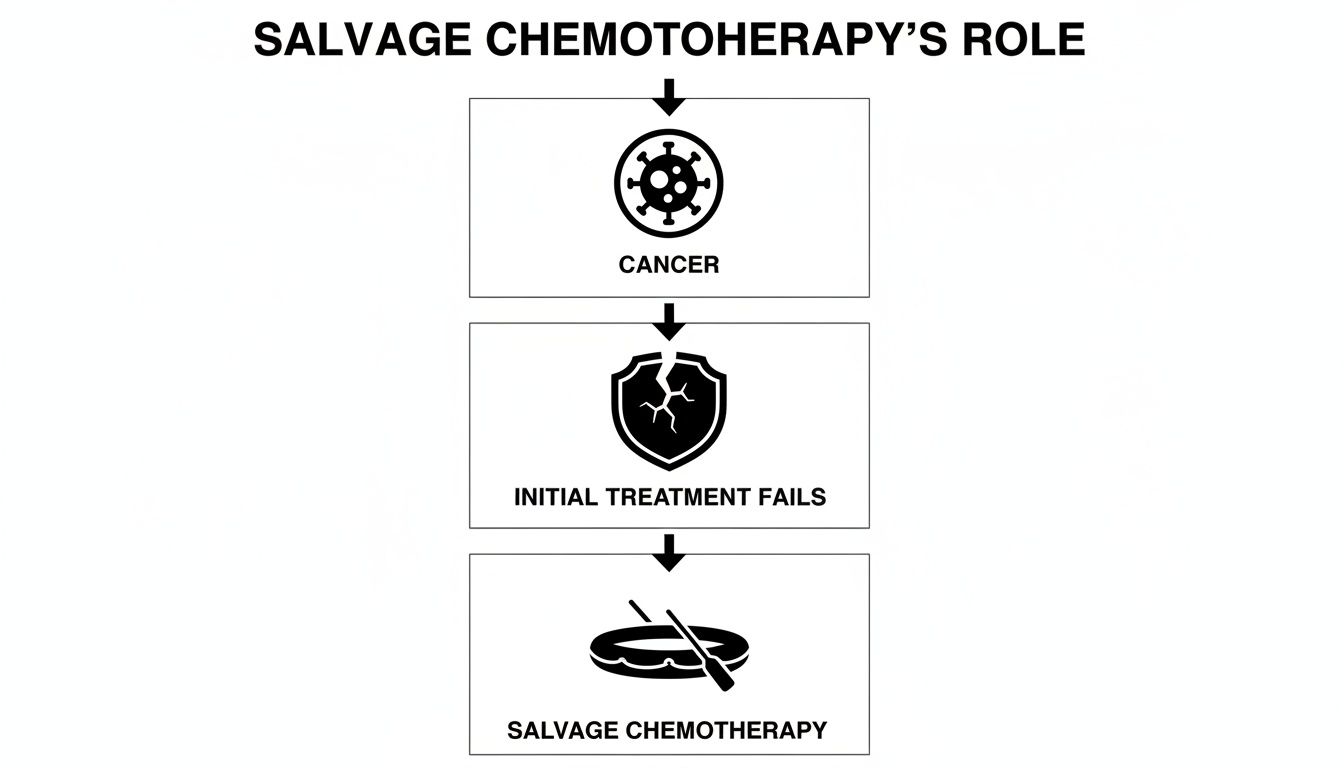
As you can see, when that first line of defense is no longer holding, salvage therapy opens up a new path forward.
When is a Second-Line Treatment Needed?
This type of treatment is typically recommended for cancers that are considered "relapsed" or "refractory." While they sound similar, they describe two different scenarios:
- Relapsed Cancer: This is when cancer returns after you’ve been in remission. The initial treatment worked for a while, but the cancer found a way to come back.
- Refractory Cancer: This describes a cancer that either never responded to the initial treatment or stopped responding while you were still on it.
In both of these situations, it’s clear the original plan is no longer the best one. The primary goal of salvage chemotherapy is to find a different approach to regain control. To get a better sense of the underlying science, you can read our guide on how chemotherapy works and why different drugs are used.
The core idea behind salvage therapy is adaptation. Cancer cells are clever and can learn to resist certain drugs. Salvage chemotherapy uses new drugs or different combinations that the cancer hasn't seen before, hitting it where it's vulnerable.
First-Line Vs Salvage Chemotherapy At a Glance
To make the distinction clearer, here's a quick comparison of the two approaches.
This table highlights that while both use chemotherapy, their purpose and timing are fundamentally different. One is the opening move, and the other is a calculated counter-move.
What Impact Can Salvage Chemotherapy Have?
This isn’t just a theoretical approach—it makes a real difference. For patients whose cancer has progressed, salvage chemotherapy can be a crucial lifeline, offering a chance at more time when other options have run out.
For example, a study looking at patients with advanced cancers like pancreatic or colorectal cancer found that those who received salvage chemotherapy had a median overall survival of 16.6 months. This was a significant improvement compared to the 2.4 months for patients who only received the best supportive care.
Ultimately, salvage chemotherapy is a powerful example of how modern oncology refuses to give up. It’s about being persistent, using new knowledge and different tools to continue the fight, always with the goal of extending life and improving its quality.
When Doctors Recommend Salvage Chemotherapy
Deciding to move on from a first-line treatment is a major step in any cancer journey, and it’s a conversation your oncology team takes very seriously. They are constantly looking for clues to see how well the initial strategy is working. The shift to salvage chemotherapy only happens when there's clear evidence that the cancer is no longer responding to the current plan.

Ultimately, the recommendation for salvage therapy comes down to a few key situations where it’s obvious the cancer has found a way around the treatment.
Key Triggers for a Treatment Change
Oncologists look for very specific signs that it’s time for a new game plan. These signals tell us that the first-line drugs aren't doing their job anymore, making it the right moment to pivot.
There are three common scenarios that prompt this change:
- Cancer Progression: This is when imaging scans, like a CT or PET scan, show that existing tumors are getting bigger or that new ones have popped up, even while you’re on treatment. It’s a straightforward sign that the cancer is on the move and the current drugs can no longer keep it in check.
- Cancer Resistance (Refractory Disease): In this case, the cancer either stops shrinking or actually starts growing again during the first-line treatment. The cancer cells have basically figured out how to survive the drugs, making the therapy ineffective. To learn more, read our article on what happens when chemotherapy stops working.
- Cancer Recurrence (Relapsed Disease): This happens when the initial treatment works beautifully—you might have even achieved remission—but the cancer comes back after some time has passed. It means a small number of cancer cells managed to survive the first round and have started multiplying again.
For certain cancers, this transition is an expected part of the treatment path. With epithelial ovarian cancer, for example, salvage chemotherapy is a crucial next step for most women. Relapse occurs in 50%–75% of advanced cases after the initial therapy is finished, meaning a second-line approach is often necessary.
How Oncologists Confirm the Need for Salvage Therapy
To be absolutely sure a change is needed, your oncology team uses a combination of tools to get a complete picture of what's going on.
They look for evidence from a few different angles:
- Imaging Scans (CT/PET/MRI): These give us the visual proof. Scans let doctors see, in detail, if tumors are growing, spreading, or shrinking. A scan showing definite growth is one of the strongest reasons to switch to a salvage regimen.
- Tumor Marker Blood Tests: Some cancers release specific proteins into the blood called tumor markers (think PSA for prostate cancer or CA 19-9 for pancreatic cancer). A consistent rise in these levels can be an early warning sign that the cancer is becoming more active, sometimes even before changes appear on a scan.
- Symptom Assessment: How you’re feeling is a critical piece of the puzzle. If cancer-related symptoms like pain, fatigue, or sudden weight loss are getting worse, it can also suggest the disease is progressing and the current treatment isn't controlling it.
An oncologist's decision to recommend salvage therapy is like putting together a puzzle. Scans are the corner pieces, blood tests fill in the edges, and your physical symptoms provide the final, central pieces. Only when the full picture shows progression does the team recommend a new plan.
Considering Your Overall Health and Fitness
Finally, the decision isn't just about the cancer; it's about you. Before recommending a new, potentially intensive treatment, your doctor will carefully evaluate your overall health. We often use a performance status scale, like the ECOG score, to get a clear sense of your strength and ability to handle daily activities.
This score helps us determine if you are physically resilient enough to tolerate another round of chemotherapy. Someone who is still active and getting around well is much more likely to manage the side effects. This whole-person assessment ensures that any new treatment we choose will not only fight the cancer but also fit with your ability to maintain a good quality of life.
Understanding the Goals of Salvage Therapy
When you're facing a new treatment plan, it’s crucial to know what you’re aiming for. The goals of salvage chemotherapy are usually quite different from your first round of treatment. Understanding this shift is the first step toward feeling in control of your care. Think of it as moving from an all-out sprint to a strategic, long-term marathon.
The conversation shifts from focusing only on a complete cure to a more nuanced set of objectives. The new mission is to regain control over the cancer now that the initial approach isn't working anymore. This isn't about giving up—it's about adapting the game plan to the new reality of the disease.
Your oncologist will start talking about a different set of priorities, each one designed to improve your life in tangible ways.
Shifting from Cure to Control
While a cure remains the ultimate hope, the practical, day-to-day goals of salvage therapy often center on management. The real aim is to turn an aggressive, fast-moving cancer into something more like a manageable, chronic condition.
This new strategy typically has three main objectives:
- Slowing Tumor Growth: First and foremost, the goal is to stop or dramatically slow the cancer's progression. By finding a drug or combination that the cancer is still sensitive to, we can keep tumors from getting bigger or spreading.
- Managing Symptoms: Advanced cancer often brings with it pain, fatigue, and other symptoms that can really disrupt your life. A key part of salvage therapy is shrinking tumors just enough to relieve that pressure, helping you feel better and get some of your energy back.
- Extending Survival with Quality: Ultimately, salvage therapy is about giving you more time—more months, or even years. But just as important is making sure that time is good time. We're constantly balancing the treatment’s power with your overall quality of life.
The core idea behind salvage therapy is to manage the cancer in a way that lets you live your life as fully as you can. It’s about adding life to your years, not just years to your life.
What Success Looks Like in Salvage Therapy
In this stage of treatment, we measure success differently. A huge win might be stabilizing the disease for a long stretch, giving you the time and health to attend a family wedding, watch a grandchild graduate, or simply enjoy more good days at home.
Take, for example, locally advanced cervical cancer that has resisted initial treatments. In these cases, salvage chemotherapy is the go-to rescue strategy, used in 51.8% of situations. Modern drug combinations can now achieve a median progression-free survival of 11.2 months and an overall survival of 25 months. These aren't just statistics; they represent a massive leap from what was possible in the past, offering patients precious, quality time. You can read more about these important salvage therapy findings.
This is a powerful reminder of how today's salvage regimens can meaningfully extend the clock and restore hope.
Balancing Efficacy with Quality of Life
Your oncology team knows that a treatment is only a true success if you can tolerate it without sacrificing your quality of life. Every decision about a salvage regimen involves a careful balancing act, weighing the potential for a good response against the likely side effects.
This balance is deeply personal, and it's where you and your doctor become true partners. The conversation will cover:
- The likelihood of response: How well is this treatment expected to work? What are the chances it will shrink the cancer or at least stop it from growing?
- The potential side effects: What are the common side effects, and what’s our plan to manage them before they become a problem?
- The impact on your daily routine: How will the treatment schedule fit into your life? Will you still be able to work, spend time with family, or enjoy your hobbies?
This open dialogue ensures the path we choose aligns with your personal values, not just our medical targets. The goal is to find a sustainable rhythm—a treatment that keeps the cancer in check while still allowing you to live well.
Common Treatments and Managing Side Effects
Stepping into a salvage chemotherapy plan means exploring a new set of medications and strategies. Your oncology team selects these treatments with immense care, aiming not just to attack the cancer but to do so while protecting your quality of life. The focus shifts to finding a regimen that is both potent against the cancer and manageable for you.
This often involves using different combinations of drugs tailored to your specific cancer and treatment history. For example, if you're facing pancreatic cancer, a common salvage regimen might be FOLFIRINOX or a gemcitabine-based therapy, depending on what was used first. For colorectal cancer, oncologists might turn to drugs like Lonsurf or Stivarga. The specific choice always comes down to your unique situation—what you've had before and how the cancer has responded.
However, modern oncology has evolved far beyond just traditional chemotherapy. Many salvage strategies now weave in newer, more precise approaches designed to be much easier on your body.
Modern Approaches to Improve Tolerability
The goal of today’s salvage therapy is to be smarter, not just stronger. Oncologists have several techniques to minimize the harshness of treatment while maximizing its impact on cancer cells. This means your treatment plan might feel very different from what you experienced the first time around.
Key strategies include:
- Lower-Dose Regimens: Sometimes, using chemotherapy drugs at a lower, more frequent dose can be just as effective at controlling cancer but with far fewer side effects. Think of it as a steady, consistent pressure on the cancer rather than an overwhelming assault on your whole body.
- Integrating Targeted Therapies: These "smart drugs" are designed to attack specific weaknesses unique to the cancer cells. Because they are more precise, they often spare healthy cells, leading to a different and sometimes milder set of side effects.
- Adding Immunotherapies: These treatments work by taking the brakes off your own immune system, allowing it to finally recognize and fight the cancer. While they have their own unique side effects, they can be a powerful and well-tolerated option for certain types of cancer.
This multi-faceted approach allows your care team to build a highly personalized plan. It’s all about finding the right tools for the job—ones that effectively corner the cancer while helping you continue to live your life.
Proactively Managing Common Side Effects
Even with more tolerable regimens, side effects are a reality of cancer treatment. The biggest difference in modern care is the shift to proactive management. Your medical team anticipates these issues and has a plan ready to go, aiming to address them before they can become severe.
Some of the most common side effects are now framed as manageable challenges, not unavoidable miseries.
The entire philosophy of modern supportive care is to stay ahead of side effects. We don't wait for you to feel unwell; we provide medications and strategies from day one to prevent or lessen the impact of treatment, ensuring you maintain the best possible quality of life.
Here is a practical guide to some common side effects and how your team will help you manage them.
Managing Common Side Effects of Salvage Therapy
This table breaks down what you might feel and the proactive steps your team will take to keep you comfortable.
Your team is there to help you navigate this entire process.
They'll provide guidance on everything from nutrition and hydration to mental health support. Understanding the bigger picture of treatment safety is also crucial. You can find more general safety information to feel better prepared. This isn't just about enduring treatment; it’s about having a strong support system in place to help you live well through it.
Exploring Treatments Beyond Chemotherapy
When cancer comes back or stops responding to the first line of defense, it's natural to assume that "salvage therapy" just means more chemotherapy. But the world of oncology has expanded dramatically. Think of your treatment plan like a highly specialized toolkit—while chemotherapy is a crucial tool, we now have many others designed to fight cancer from completely different angles.
Today, a smart salvage strategy often involves combining these approaches or using them in a specific sequence. This lets your oncology team create a personalized plan that’s anything but one-size-fits-all. We can be more strategic, choosing the right tool for the job based on your cancer’s unique biology and your overall health. The goal is always to find a path forward that is not only effective but also sustainable for you.
Targeted Therapy: The "Smart Drugs"
One of the biggest breakthroughs in modern cancer care is targeted therapy. If you think of traditional chemotherapy as a broad-spectrum approach that affects many different cells, targeted therapy is more like a precision-guided missile. It’s engineered to attack the specific molecules—often proteins or mutated genes—that cancer cells depend on to grow and survive.
These drugs work by zeroing in on a tumor's unique vulnerabilities. For example, a targeted drug might shut down a specific signal that tells cancer cells to divide, or it might cut off the blood supply that a tumor needs to get bigger.
Because these drugs are so specific, they tend to spare healthy cells. This can lead to a different, and sometimes more manageable, set of side effects compared to conventional chemotherapy. Before we can use this approach, your oncologist will run tests on a tumor sample to confirm it has the specific molecular "target" these drugs are designed to hit.
Immunotherapy: Unleashing Your Immune System
Another powerful tool in our kit is immunotherapy. This approach is fascinating because it doesn't attack the cancer directly. Instead, it works by "unleashing" your own immune system, essentially training it to recognize and destroy cancer cells far more effectively.
Cancer cells are notoriously sneaky; they can develop tricks to hide from the immune system, almost like putting on an invisibility cloak. Immunotherapy drugs, especially a class known as checkpoint inhibitors, work by tearing that cloak off. They block the signals cancer cells use to hide, allowing your body's natural defenses—your T-cells—to finally see the cancer and launch an attack.
Immunotherapy represents a fundamental shift in cancer treatment. Instead of relying on external drugs to kill cancer cells, we are now able to empower a patient’s own body to do the fighting. It’s a strategy that can lead to durable, long-lasting responses in some patients.
Immunotherapy has produced incredible results in many cancers, including melanoma, lung cancer, and kidney cancer, particularly as part of a salvage therapy plan. To get a better handle on how it works, you can learn more about immunotherapy for cancer in our detailed guide.
Clinical Trials: Access to Tomorrow's Treatments
When standard treatments are no longer an option, clinical trials can open a door to the next generation of cancer care. These carefully designed research studies test new drugs, new combinations, or entirely new treatment methods to see if they are safer and more effective than what’s currently available.
Participating in a clinical trial gives you access to treatments that aren't yet on the market. For many people with advanced or treatment-resistant cancers, this is a chance to be on the front lines of medical science and potentially benefit from a major breakthrough.
Palliative Care: An Essential Layer of Support
Finally, it’s absolutely critical to understand the role of palliative care. So many people mistakenly think it's the same as end-of-life or hospice care, but that couldn't be further from the truth. Palliative care is specialized medical support focused on providing relief from the symptoms and stress of a serious illness—no matter the diagnosis or prognosis.
The main goal is to improve the quality of life for both you and your family. It's provided right alongside curative treatments like salvage chemotherapy, at any stage of your illness. The palliative care team partners with your oncologist to manage:
- Pain, nausea, fatigue, and other physical symptoms
- The emotional and psychological weight of a cancer diagnosis
- Practical, logistical, and spiritual concerns
Bringing palliative care into the picture early is a key part of a truly comprehensive, patient-first approach. It ensures your comfort and well-being are always a top priority, helping you live as well as possible throughout your treatment journey.
How to Make an Informed Treatment Decision

Deciding on the next step in your cancer care is a profoundly personal journey. Your oncologist provides the medical expertise, but you are the expert on your own life, values, and what you hope to achieve. You're not just a passenger; you are the most important member of your care team.
This collaborative approach is called shared decision-making. Think of it as a partnership where you and your doctor work together to find a plan that makes sense medically and, just as importantly, aligns with what matters to you. It’s all about making sure you feel confident and in control of the path ahead.
Starting the Conversation with Your Oncologist
To make this partnership work, you need good information. I always tell my patients that walking into an appointment with a list of questions is one of the most powerful things they can do. It’s not about second-guessing your doctor; it’s about building a complete picture together.
To get the ball rolling, consider asking questions like these:
- What is the specific goal of this treatment for my situation right now?
- Realistically, what are the chances it will help, and for how long?
- How will this treatment affect my day-to-day life and energy?
- How will we get ahead of side effects before they become a big problem?
- What other options should we be talking about, including any clinical trials?
These questions help shift the conversation from just the "what" of treatment to the "how"—how it will fit into the fabric of your life.
Weighing Benefits Against Burdens
Every cancer treatment involves a trade-off between potential benefits and definite burdens. The "best" choice is the one where that trade-off feels right for you. Your oncologist can lay out the medical odds and facts, but only you can weigh them against your personal priorities.
For example, a treatment might offer a 30% chance of shrinking the cancer but means spending every week at the infusion clinic. Another option might be less effective on paper but is a simple pill you can take at home. There's no single right answer here. The best path is the one that respects what you value most, whether that's time at home, energy for hobbies, or fighting for every possible day.
The goal of any treatment discussion is simple: clarity. You should walk away feeling like you truly understand your choices, the possible outcomes, and that the plan you’ve made reflects what you want for your health and your life.
In the complex world of cancer care, doctors often use sophisticated tools to help guide these conversations. Learning about clinical decision support systems can show how technology helps refine treatment recommendations for complex situations like salvage therapy.
Ultimately, making an informed choice is about feeling heard. It's about finding a path that doesn't just treat the cancer but also honors you as a person, protecting your quality of life and your hope for the future. You are in the driver's seat, with your care team right there beside you to help navigate the road.
Answering Your Questions About Salvage Chemotherapy
When your doctor brings up salvage chemotherapy, it's completely normal for your mind to start racing with questions. Let's walk through some of the most common concerns we hear from patients and their families, breaking them down with clear, straightforward answers.
Is This a "Last Resort" Treatment?
Not at all. A better way to think about it is as the next strategic step. When a cancer stops responding to the first plan of attack, salvage therapy isn't a shot in the dark; it's a carefully planned pivot to a new approach designed to get the cancer back under control.
This is a standard part of the treatment roadmap for many types of cancer, especially those known to be stubborn or likely to recur. It's a proactive and hopeful way forward, not an act of desperation.
How Is This Different From My First Round of Chemo?
The biggest differences are in the goals and the specific drugs we use. The first time around, the aim is usually a cure or a long-lasting remission using a standard, well-established regimen. With salvage chemotherapy, the focus often shifts to controlling the cancer's growth, easing symptoms, and extending your good-quality time.
Because of that, the medications will likely be different. Your oncologist will specifically choose drugs your cancer hasn't "seen" before, looking for a new chink in its armor. The intensity and schedule might also be adjusted to strike a better balance between fighting the cancer and protecting your overall well-being.
What Makes Someone a Candidate for Salvage Therapy?
Your oncology team looks at a few key things before recommending this path. It really comes down to a complete picture of your health.
- Your Cancer's Behavior: We need clear evidence—from scans, blood work, or how you're feeling—that the cancer is growing again, has become resistant to the current treatment, or has returned after being in remission.
- Your Overall Health: How strong you are physically is a huge factor. We need to be confident you can handle another course of treatment. Doctors often use a tool called a "performance status scale" to make sure the benefits will outweigh the physical toll.
- Your Treatment History: What you've already been through gives us crucial clues. Knowing which drugs worked before (and for how long) helps us predict which new ones are most likely to be effective now.
Should I Expect the Side Effects to Be Worse?
Not necessarily. While some salvage treatments can be intense, a huge part of modern cancer care is getting ahead of side effects. We have so many more tools at our disposal now. Your team might use different dosing schedules or combine chemotherapy with targeted drugs or immunotherapies, which often have entirely different—and sometimes milder—side effects.
We are far more aggressive with supportive care than ever before. This means we start anti-nausea medications, pain management, and other strategies right from the beginning to prevent discomfort, not just treat it after it starts. The goal is to help you maintain the best quality of life possible.
The entire strategy is about finding a treatment that's tough on the cancer but as manageable as possible for you.
At Hirschfeld Oncology, creating personalized salvage strategies for complex, advanced, and treatment-resistant cancers is at the core of what we do. Dr. Hirschfeld and our team are committed to exploring every option to find a path forward that honors your goals and prioritizes your well-being. To learn more about our approach, we invite you to visit our blog at https://honcology.com/blog.





.png)


.png)
.png)




