At its core, chemotherapy uses powerful medicines to find and destroy cells that are dividing rapidly—which is exactly what cancer cells do. It’s what’s known as a systemic treatment, meaning the drugs travel throughout your entire body to hunt down cancer cells wherever they might be.
This approach is designed to stop these aggressive cells from multiplying and spreading.
How Chemotherapy Finds and Fights Cancer
Think of your body as a vast, complex garden. Cancer cells are like aggressive weeds that grow and spread much faster than the healthy plants around them. Chemotherapy is like a specialized weed killer that circulates through the whole garden, designed to target and eliminate these weeds.
This is a key difference from treatments like surgery or radiation, which are "local" and focus on one specific spot. Chemo's systemic nature is its greatest strength. It can attack the main tumor while also tracking down any cancer cells that might have broken off and traveled to other parts of the body (a process called metastasis).
The primary mission of these drugs is to disrupt the cancer cell's ability to divide and make copies of itself, effectively shutting down its growth engine.
Targeting Rapid Cell Division
The one thing all cancers have in common is uncontrolled, rapid cell growth. Chemotherapy is built to take advantage of that very weakness.
The drugs are designed to damage the internal machinery or DNA of any cell caught in the act of dividing. Since cancer cells divide far more often than most of your normal, healthy cells, they are much more likely to be affected and destroyed by the treatment.
Of course, this powerful mechanism is also why side effects happen. Some of your healthy cells also divide quickly as part of their normal job. This includes cells in your:
- Hair follicles
- Bone marrow (which makes your blood cells)
- The lining of your mouth and digestive tract
When these healthy, fast-growing cells are temporarily damaged along with the cancer cells, it can lead to some of the common side effects of treatment. Your oncology team knows this and plans for it. That’s why chemo is usually given in cycles—a period of treatment followed by a period of rest.
This "work and rest" schedule is intentional. It gives your healthy cells a chance to recover and rebuild, while the cancer cells are hit again and again with each new cycle. Understanding the effectiveness of this cyclical process helps put the treatment journey into perspective. Learn more about what makes chemotherapy effective in our detailed guide.
Chemotherapy remains a cornerstone of cancer care for a reason. A major global study found that in 2018, 58% of all new cancer cases—a staggering 9.8 million people—needed chemotherapy. With cancer diagnoses expected to increase, the demand for chemotherapy is projected to rise by 53% by 2040. You can explore the full study about the global demand for chemotherapy.
To make these concepts even clearer, let's break them down into a simple table.
Chemotherapy at a Glance: Key Concepts Explained
This table provides a quick summary of the fundamental principles of chemotherapy, helping you grasp the core ideas before we dive deeper into the details.
This foundation gives us a much better understanding of not just what chemotherapy does, but how it accomplishes its goal.
A Closer Look at Different Types of Chemo Drugs
Not all chemotherapy drugs are created equal. Think of it like a master carpenter's toolkit—you wouldn't use a sledgehammer for a delicate finishing job. In the same way, oncologists have a wide array of chemotherapy drugs, and each one is designed for a specific task in the fight against cancer.
The choice of drug is anything but random. It depends on the type of cancer you have, where it is, and sometimes even its unique genetic signature. Each category of chemotherapy has a distinct mission, targeting the cancer cell’s ability to grow and survive at different points in its lifecycle. This strategic approach is the key to making chemotherapy work.
The core idea is simple: use powerful drugs to disrupt the out-of-control growth of cancer cells. This visual breaks it down.
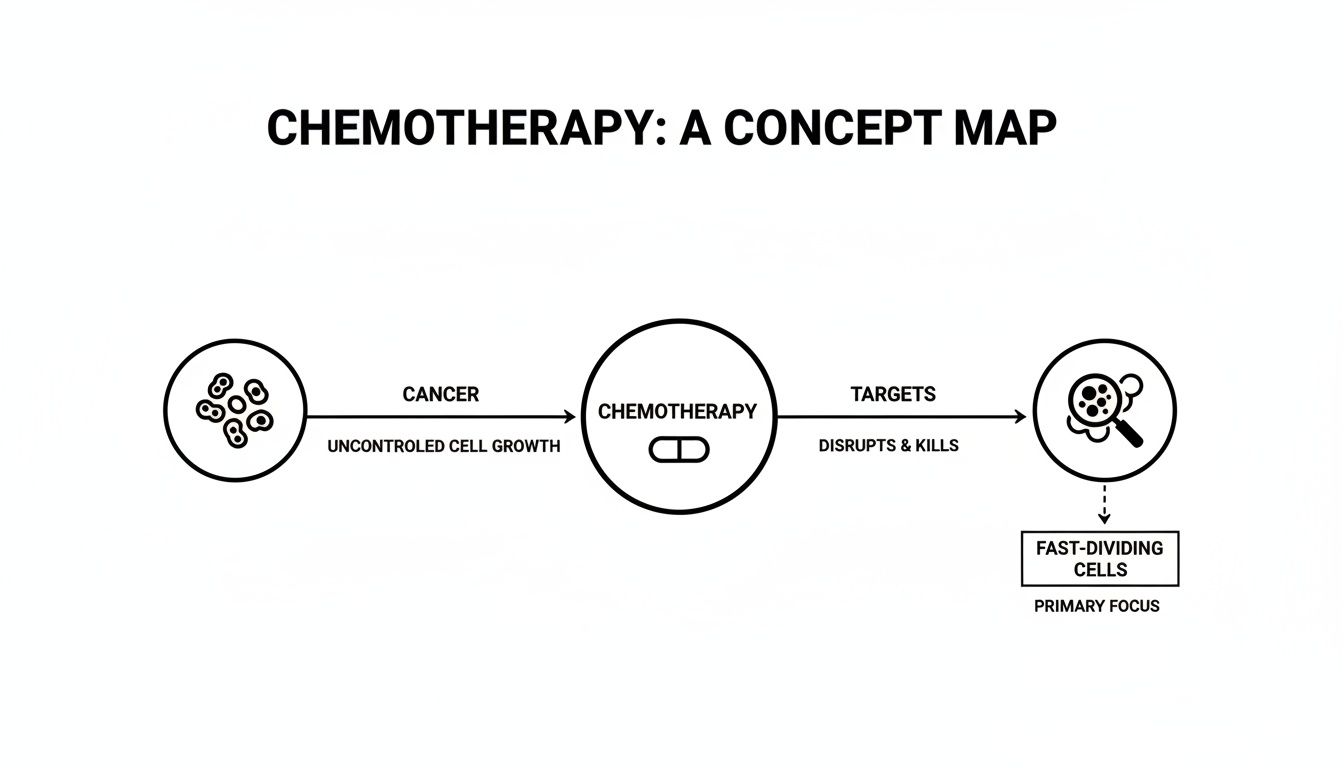
As you can see, chemotherapy is all about interfering with the machinery that allows these cells to multiply so quickly. Let's dig into the main types of these drugs and how they accomplish their mission.
Alkylating Agents: The DNA Saboteurs
Among the oldest and most reliable tools in the box, alkylating agents work by causing direct, irreversible damage to a cancer cell's DNA.
Imagine them as saboteurs who weld the two sides of a DNA zipper together. When the cell tries to unzip its DNA to make a copy, it can't. The strands are stuck. This damage is often so catastrophic that it triggers a self-destruct sequence called apoptosis, forcing the cancer cell to die. Because they can attack cells at any stage of their life, these drugs are workhorses used against a broad range of cancers, including leukemias, lymphomas, and various solid tumors.
Antimetabolites: The Impostors
Antimetabolites are masters of deception. They are designed to perfectly mimic the natural building blocks—metabolites—that a cell needs to construct its DNA and RNA. Cancer cells, which are constantly gobbling up resources to fuel their rapid division, readily take in these fakes.
Once inside, these impostor drugs bring the cell's production line to a grinding halt. They either clog up the enzymes needed for DNA synthesis or get inserted directly into the DNA strand, creating a faulty blueprint. Either way, the cell can no longer divide. This clever strategy is especially potent against fast-growing cancers like certain leukemias and cancers of the breast, ovaries, and digestive system.
Anthracyclines: The DNA Unravelers
Anthracyclines are a particularly powerful class of chemo drugs because they launch a two-pronged attack on cancer cells.
Their primary job is to interfere with enzymes called topoisomerases. These enzymes are crucial for untangling and re-tangling DNA during cell division—a bit like a librarian carefully managing a complex scroll. By jamming these enzymes, anthracyclines prevent the DNA from being copied correctly, stopping cell replication in its tracks. As a bonus, they can also generate highly reactive molecules called free radicals that inflict even more damage on the cell's DNA and membranes. Often recognizable by their distinct red color, these drugs are effective against a wide variety of cancers.
A Note on Combined Strategies: You’ll often hear the term "combination chemotherapy." This means your oncologist is using drugs from different classes together. Hitting the cancer from multiple angles at once makes it much harder for cells to develop resistance and dramatically increases the treatment's overall effectiveness.
Mitotic Inhibitors: The Division Blockers
Another major group of chemo drugs is the mitotic inhibitors. Many of these are derived from natural plant sources, and their sole purpose is to stop cell division (a process called mitosis) right as it's happening.
They do this by targeting microtubules, which are tiny protein fibers that act as a cell's internal scaffolding. During division, these fibers have the critical job of pulling the newly copied chromosomes apart into two identical daughter cells.
Mitotic inhibitors throw a wrench in this process in one of two ways:
- Some prevent the microtubules from forming properly in the first place.
- Others stabilize them so much that they can't be broken down when their job is done.
Either way, the result is the same: the cell gets stuck mid-division and can't complete the process, which ultimately leads to its death. This makes them a vital tool against many different cancers. Understanding these different strategies helps paint a clearer picture of how your personal chemotherapy plan is built to be as precise and effective as possible.
Defining the Goals of Your Chemotherapy Treatment
Now that we’ve looked at the different types of chemotherapy drugs, let's talk about the big picture: what are we trying to accomplish? Chemotherapy isn't a single tool for a single job. The goal can be entirely different from one person to the next, and understanding your specific mission is a powerful first step.
Think of your oncologist as a strategist. Before starting any treatment, they map out a clear objective. This goal dictates everything that follows, from the specific drugs you'll receive to how often you'll receive them. We generally group these goals into three main categories.
Aiming for a Cure
When the goal is a cure, we're swinging for the fences. The mission is to completely eradicate every last cancer cell in the body, giving you a long-term, disease-free life. This is often the most intensive approach and is typically used when a cancer is caught early or is known to be very responsive to chemotherapy.
You’ll often see this strategy used after surgery to hunt down and destroy any microscopic cancer cells that might have been left behind. We call this adjuvant therapy, and its whole purpose is to dramatically lower the chances of the cancer ever returning.
Here, success is clear-cut: achieving complete remission and getting you back to your life.
Controlling the Cancer
For some, especially with cancers that are more advanced, the goal shifts from cure to control. The objective here is to shrink tumors, stop them in their tracks, or prevent them from spreading. The focus becomes treating cancer like a chronic condition, similar to how one might manage heart disease or diabetes.
This approach can add months, and often years, to a person's life while also helping them feel better and maintain their quality of life. Chemotherapy for control can slow down a fast-growing disease, turning it into a manageable one and giving you more time to do the things you love.
Success in this case isn't measured by a complete cure, but by keeping the cancer under control. Stable scans over a long period or shrinking tumors that ease symptoms are huge wins.
The impact of this is very real. For instance, in early-stage breast cancer, adjuvant chemo helps push cure rates well over 70-90%. And for stage III colon cancer, a diagnosis we frequently see here at Hirschfeld Oncology, adding chemotherapy after surgery is a game-changer for 5-year survival. You can learn more by reading about chemotherapy success rates across different cancers.
Focusing on Comfort (Palliative Care)
Finally, chemotherapy can be used with palliative intent. This is a compassionate approach focused entirely on improving your quality of life by easing symptoms caused by cancer. It’s not about curing the disease, but about making you feel as comfortable as possible.
Palliative chemo often involves lower, less aggressive doses designed to shrink tumors that are causing specific problems.
What Does Palliative Chemotherapy Help With?
- Reducing Pain: Shrinking a tumor that’s pressing on a nerve.
- Improving Breathing: Easing pressure from a tumor in the lung causing shortness of breath.
- Restoring Function: Relieving a blockage in the digestive system to help with eating.
Success here is measured by your well-being. Less pain, a better appetite, or just having more energy to spend with your family—these are the victories we aim for. This approach truly honors a core principle of good medicine: we treat the person, not just the disease.
To make this even clearer, let's break down these different goals in a simple table.
Understanding the Goals of Your Chemotherapy
Knowing the "why" behind your treatment plan can help you feel more grounded and prepared for the road ahead. Always feel empowered to ask your care team, "What is the primary goal of this chemotherapy for me?" The answer will help frame your entire experience.
How Your Chemotherapy Plan Is Designed and Delivered
Knowing which drugs are used to fight cancer is one piece of the puzzle. The other, equally important piece is understanding how your personal treatment plan actually comes together. This isn't a "one-size-fits-all" approach; we design your chemotherapy plan specifically around you, your type of cancer, and your overall health.
This plan answers the big questions: Which drugs will we use? What’s the right dose? How often will you need to come in for treatment? We think through every detail to hit the cancer cells as hard as possible while giving your body the time it needs to recover between sessions. It's all about finding a rhythm that's both effective and manageable for you.

Understanding Chemotherapy Cycles and Schedules
One of the first things you'll hear about is your treatment cycle. The easiest way to think about it is a repeating pattern of "work and rest." You’ll receive treatment for a certain amount of time, and then you’ll have a scheduled break before the next round. This entire pattern is one cycle, which we repeat a set number of times.
The "work" phase is when the chemotherapy drugs are actively doing their job. But the "rest" phase is just as vital. It gives your healthy cells—like the ones in your bone marrow and digestive system—a chance to bounce back and rebuild. This deliberate pacing is key to managing side effects and keeping you strong enough for your next treatment.
A typical cycle might last two, three, or even four weeks. For example, a 21-day cycle might involve getting chemo on the first day, followed by 20 days of rest and recovery. Your specific schedule is something your oncologist designs based on proven treatment protocols and how your body responds. You can get a much deeper look into how often chemotherapy is given and all the factors that go into that decision.
A chemotherapy plan is not just about the drugs themselves; it's about the timing. The schedule is a strategic weapon designed to keep constant pressure on the cancer while allowing your body the necessary time to heal and stay resilient.
Common Ways Chemotherapy Is Administered
Once we’ve mapped out the schedule, the next question is how you’ll receive the medicine. Most people immediately picture an IV drip, but there are actually several ways to deliver chemo, and we choose the best one for your specific drug and cancer type.
Your care team here at Hirschfeld Oncology will walk you through exactly what to expect. Generally, these are the most common methods:
- Intravenous (IV) Infusion: This is what most people are familiar with. We deliver the medicine directly into your bloodstream through a small, thin tube placed in a vein. An infusion can take anywhere from 30 minutes to a few hours, and you’ll receive it right here at our center.
- Oral Chemotherapy: Some chemo drugs now come as a pill or capsule you can take at home. While this is certainly more convenient, it’s incredibly important to stick to the prescribed schedule to make sure it works effectively.
- Injections: Certain drugs are given as a quick shot, either just under the skin (subcutaneous) or deeper into a muscle (intramuscular). This is usually done quickly in the clinic.
There are also less common but very specific methods, like delivering chemo directly into the spinal fluid (intrathecal) or into an artery that supplies a specific organ. The delivery method is always chosen to get the drug exactly where it needs to be. Your personalized plan is a testament to the thoughtful, deliberate process behind modern cancer care.
Combining Treatments for a Stronger Attack on Cancer
Chemotherapy is a powerful tool in the fight against cancer, but it very rarely works alone. It's better to think of it as a key player on a highly skilled team, where every member brings a unique and vital strength to the table. Modern cancer care is built around this team-based approach, combining different therapies to create a multi-pronged attack that is far more effective than any single treatment could ever be.
This strategy allows us to attack the cancer from multiple angles at once. By doing so, we can head off potential resistance, improve outcomes, and often achieve results that were once considered out of reach. It’s a thoughtful, strategic approach that tailors the fight to your specific type of cancer.
Chemo as a Partner to Surgery and Radiation
One of chemotherapy’s most important jobs is to support local treatments like surgery and radiation. It can be used before, during, or after these procedures to make them as effective as possible. This collaborative relationship is a cornerstone of how we achieve lasting results.
There are two main ways we do this:
- Neoadjuvant Chemotherapy: This is chemo given before surgery. The primary goal here is to shrink a large tumor, making it much easier for the surgeon to remove it completely. This often means the surgery can be less extensive, which can lead to a better recovery and outcome.
- Adjuvant Chemotherapy: This is chemotherapy given after surgery or radiation has finished. Its mission is to hunt down and eliminate any microscopic cancer cells that might have broken away from the original tumor. By clearing out these hidden stragglers, we can significantly reduce the risk of the cancer coming back later on.
The success of these combinations is clear. For rectal cancer, using chemotherapy and/or radiotherapy alongside other treatments can contribute to an overall 80% total survival rate. And for late-stage uterine corpus cancer, 73% of patients receive treatment plans that involve chemo in addition to surgery and sometimes radiation. You can learn more about these treatment combination statistics.
Pairing Chemo with Immunotherapy and Targeted Therapy
Beyond its classic partnership with surgery and radiation, chemotherapy is now frequently teamed up with newer, more precise treatments like immunotherapy and targeted therapy. This is where the strategy gets even more sophisticated.
Chemotherapy and ImmunotherapyImmunotherapy is fascinating because it doesn't kill cancer cells directly. Instead, it works by essentially taking the brakes off your own immune system, empowering it to recognize and attack the cancer itself. When you add chemotherapy to the mix, an incredible synergy happens.
As chemo kills cancer cells, they burst open and release unique proteins called antigens. This process essentially puts a spotlight on the cancer, making it much more visible to the newly activated immune cells. You could say chemo "unmasks" the enemy, and immunotherapy then unleashes the attack.
This one-two punch can be a game-changer. Chemotherapy creates a more favorable environment for the immune system to do its job, while immunotherapy ensures your body’s natural defenses are primed and ready to go.
Chemotherapy and Targeted TherapyTargeted therapy drugs are molecules engineered to interfere with specific pathways that cancer cells rely on to grow. They are incredibly precise—like a key designed for a single lock. Combining these precision drugs with the broader-acting power of chemotherapy can be a knockout combination.
Chemotherapy weakens the overall cancer cell population, while targeted therapy hones in on the specific escape routes the cancer needs to survive and expand. This dual approach can shut down the cancer's ability to repair itself or develop resistance, often leading to a much more durable, long-lasting response.
At centers like Hirschfeld Oncology, designing these sophisticated combination therapies is at the very heart of what we do. By thoughtfully integrating different treatments, we can build a plan that gives you the best possible chance of success while carefully managing your quality of life. This strategic, team-based fight is the future of cancer care.
Managing Side Effects and Protecting Your Quality of Life
One of the first questions almost every patient asks is about side effects. It’s a completely valid concern, and understanding why they happen is the first step toward managing them. It all goes back to chemotherapy's core mission: targeting cells that divide quickly.
This powerful approach is exactly what we need to fight fast-growing cancer cells. The catch is that our bodies have other healthy cells that also divide rapidly. Think about your hair follicles, the lining of your mouth and digestive tract, and the bone marrow that produces new blood cells. Because chemo can't always tell the difference, it can temporarily affect these healthy cells, which is what causes side effects like hair loss, nausea, or fatigue.

The great news? We've gotten incredibly good at managing these effects. Protecting your quality of life isn't just a side goal; it's a central part of every modern, thoughtful treatment plan.
Proactive Strategies for Your Well-Being
Your comfort is not an afterthought—it’s a priority from day one. Instead of just reacting to side effects, modern oncology focuses on preventing them or treating them before they become a major issue. We have a deep toolkit of medications and supportive care strategies to keep you feeling as strong as possible.
Here are a few of the most common and effective approaches we use:
- Advanced Anti-Nausea Medications: We don't wait for you to feel sick. These medications are often given before your infusion even starts and are highly effective at preventing nausea and vomiting. While over 70% of patients used to report these symptoms, modern antiemetics have dramatically changed that experience.
- Blood Count Support: Your blood counts are monitored very closely. If your white blood cells (infection fighters) or red blood cells (oxygen carriers) dip too low, we can use medications called growth factors to help your bone marrow bounce back much faster.
- Fatigue Management: Fatigue is very real, affecting about 80% of patients. We'll work with you to find a healthy balance of gentle activity and restorative rest. You might be surprised how much simple things, like short walks and good nutrition, can boost your energy.
Beyond what we do in the clinic, there's a lot you can do to feel more in control. Learning about practical strategies for quicker healing can empower you to take an active role in your own recovery.
Your oncology team’s goal is to make your treatment as tolerable as it is effective. Open communication is key—always tell your team exactly how you are feeling so they can adjust your supportive care plan.
This focus on proactive management means your journey is not just about fighting cancer, but about living as well as possible while you do it. We encourage you to check out our complete guide on managing side effects of cancer treatment for a better quality of life to learn even more.
Frequently Asked Questions About Chemotherapy
Even after learning how chemotherapy works, it's completely normal to have lingering questions about what it will actually mean for you day-to-day. We get it. This is where we answer some of the most common questions we hear from patients and their families, one by one.
The goal here is simple: to give you straightforward, practical information that helps you feel more prepared and in control as you start treatment.
How Will My Doctor Know If the Chemotherapy Is Working?
This is probably the biggest question on every patient's mind. Your oncologist uses a few key methods to track how your body is responding to treatment, creating a full picture that combines hard data with your own personal experience.
Here’s what that looks like:
- Imaging Scans: Think of CT, PET, or MRI scans as detailed maps of what's happening inside your body. By comparing new scans to the ones taken before you started treatment, your doctor can physically see if tumors are shrinking or have stopped growing.
- Blood Tests: Some cancers leave behind a trail of substances called tumor markers. We can measure the levels of these markers in your blood, and a drop in those numbers is a great sign that the treatment is hitting its target.
- Physical Exams & Symptom Checks: This one is crucial—how you feel matters. During your visits, your doctor will perform a physical exam and, just as importantly, ask you about your symptoms. Are you in less pain? Do you have more energy? These improvements are a huge indicator of success.
By weaving all this information together, your care team can see exactly how things are going and make any necessary tweaks to your plan to keep it working for you.
Is It Safe to Be Around My Family During Chemotherapy?
Yes, absolutely. For the vast majority of patients, it is completely safe to be around your loved ones, and that includes children, pregnant family members, and even your pets. Go ahead and give those hugs—they’re not only allowed but highly encouraged!
The chemotherapy drugs do their work inside your body and are then broken down and flushed out, usually within a couple of days. You aren’t radioactive or contagious in any way.
On rare occasions, a very specific type of therapy might require you to take some simple precautions with bodily fluids for a short period after an infusion. If your treatment falls into this category, your care team will give you crystal-clear instructions on what to do.
What Is the Difference Between Standard and Low-Dose Chemotherapy?
The main difference comes down to the strategy: are we going for a knockout punch or a long-term press?
Standard chemotherapy is the knockout punch. It uses the highest dose of drugs that your body can safely handle to kill as many cancer cells as possible, as quickly as possible. This aggressive approach is often the goal when the intent is to cure the cancer.
Low-dose chemotherapy, sometimes called "metronomic" chemotherapy, is more like a steady, continuous pressure. It uses much smaller doses of medicine given more frequently. Instead of directly obliterating cancer cells, the goal is often to disrupt their support systems—like cutting off their blood supply—which keeps the cancer in check with far fewer side effects. This is often used alongside other treatments, like targeted therapy, to manage cancer while helping you maintain a high quality of life.
At Hirschfeld Oncology, we focus on creating personalized cancer treatment plans that are right for you, which can include low-dose chemotherapy and combination therapies. To learn more about how we can help, we invite you to explore our approach and request a consultation on our website.





.png)


.png)
.png)




