When we talk about survival rates for bile duct cancer, the first thing to understand is that the single most important factor is the cancer's stage when it's found. While the overall 5-year relative survival rate for all stages combined is around 10-13%, this number doesn't tell the whole story.
In reality, the outlook changes dramatically depending on whether the cancer is still confined to its original spot or if it has started to spread. It's crucial to remember that these statistics are tools to help us understand the bigger picture, not a prediction of your personal journey.
What Do Bile Duct Cancer Survival Rates Really Mean?
Seeing survival statistics for the first time can be jarring. The numbers can feel cold and scary. But I encourage my patients to see them for what they are: a high-level view based on the experiences of thousands of people, not a crystal ball for any one individual.
The most common statistic you'll encounter is the 5-year relative survival rate. This figure is a comparison. It compares people with the same type and stage of bile duct cancer to people in the general population. So, if a specific stage has a 25% 5-year relative survival rate, it means that people with that cancer are, on average, 25% as likely as people without it to live for at least five years after their diagnosis.
Putting the Numbers in Context
It's easy to misinterpret these rates as some kind of deadline, but that's not their purpose. They are a starting point for a conversation with your oncology team about the general prognosis and how to build the best treatment strategy for you.
Here are a few things to keep in mind:
- These are not your personal odds: Your overall health, how you respond to treatment, and the unique characteristics of your tumor are what really matter.
- The data is from the past: These numbers are based on patients diagnosed years ago. They don't always reflect the impact of newer, more effective treatments available today.
- Stage is everything: The most significant factor influencing these statistics is whether the cancer is localized (contained) or has spread.
This infographic shows just how different the outlook can be when we compare localized versus distant-stage bile duct cancers.
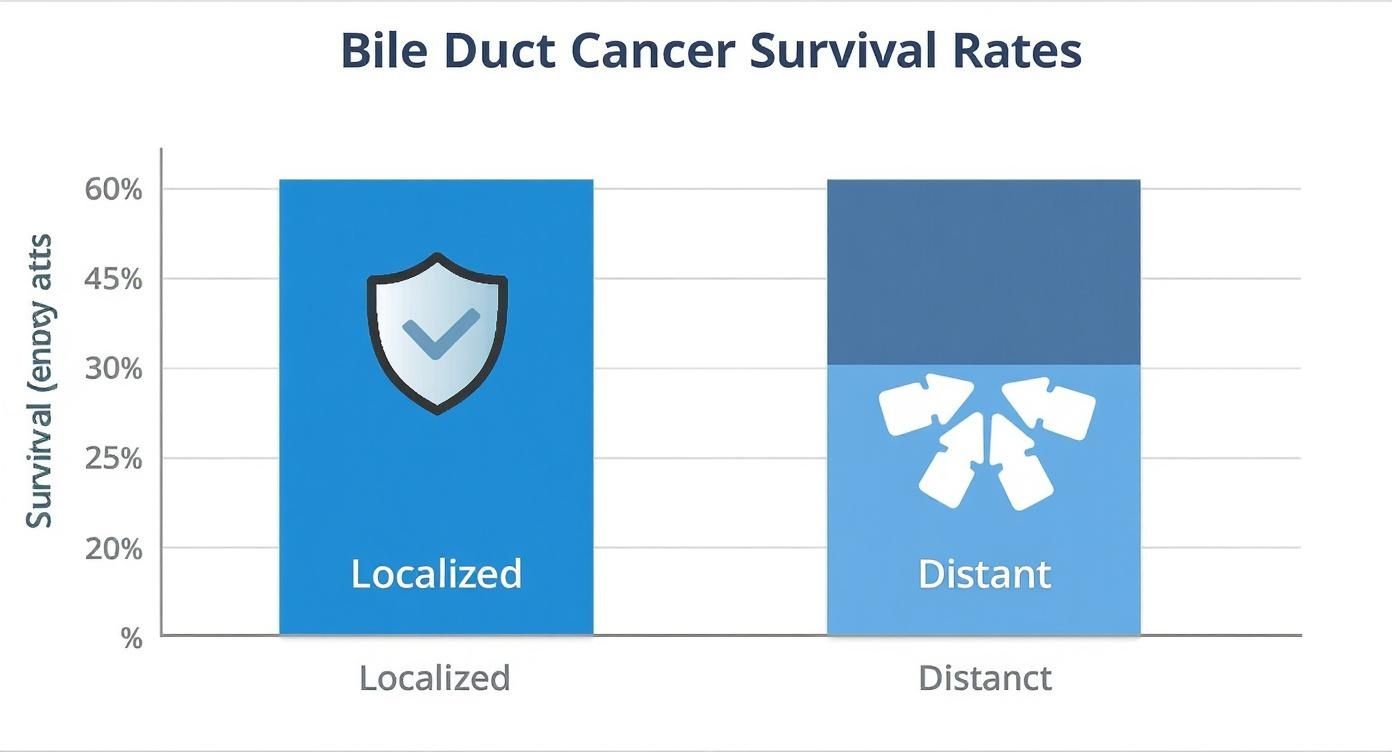
As you can see, the difference is stark. Finding the cancer early, before it has a chance to spread, is directly tied to a much more favorable prognosis.
A Closer Look at the Statistics by Stage
To give you a clearer picture, let's look at data from the National Cancer Institute's Surveillance, Epidemiology, and End Results (SEER) Program. This data, gathered between 2015 and 2021, breaks down survival by the cancer's location and stage.
5-Year Relative Survival Rates for Bile Duct Cancer by Stage
These numbers highlight the critical importance of stage. For a cancer inside the liver (intrahepatic), the 5-year survival rate is 25% if it's found when it's still localized. But that number drops to just 3% once it has spread to distant parts of the body. We see a similar pattern with cancers outside the liver (extrahepatic), where the rate is 19% for localized disease and 2% for distant disease. You can explore the complete survival statistics on the SEER website to learn more.
Understanding these statistics is the first step toward becoming an active, empowered partner in your own care. They give you a common language to discuss your prognosis and goals with your medical team, so you can make informed decisions together.
By viewing these numbers as a guide rather than a judgment, you and your family can better navigate the road ahead and focus on what truly matters: your treatment and your quality of life.
How Cancer Staging Shapes Your Prognosis
When you first get a diagnosis, it can feel like you're learning a whole new language. One of the first and most important terms you'll hear is "stage." For bile duct cancer, the stage is probably the single biggest factor in understanding what comes next, because it gives doctors a clear map of where the cancer is and how far it has traveled.
It answers the most critical questions: How big is the tumor? Has it moved into the lymph nodes nearby? Has it spread to other, more distant parts of the body?
Think of it like this: an early-stage cancer is a small, contained campfire. It's something you can manage and, with the right approach, put out completely. A late-stage cancer that has metastasized, on the other hand, is more like a wildfire that has spread across a forest. The goal changes from putting out one flame to controlling a much larger, more complex situation. This is exactly why finding the cancer early is so tied to better long-term outcomes.
Breaking Down the Stages of Bile Duct Cancer
Staging gives doctors a shared language to describe the cancer, which is essential for planning the most effective treatment. While the details can get technical, the progression from Stage I to Stage IV follows a pretty logical path of the cancer's growth and spread.
Stage I: This is as early as it gets. The tumor is small and completely contained within the bile duct where it began. It hasn't grown into any blood vessels or spread to lymph nodes. This is our "contained campfire" scenario.
Stage II: The cancer is a bit larger now. It might have started to grow through the wall of the bile duct or into nearby tissues like the liver or pancreas. Crucially, though, it hasn't reached regional lymph nodes or distant organs yet.
Stage III: At this point, the cancer is considered locally advanced. It has usually spread to nearby lymph nodes or major blood vessels, which makes it much harder to treat with surgery alone.
Stage IV: This is the most advanced stage, often called metastatic cancer. The cancer has now traveled to distant parts of the body, like the lungs, bones, or the lining of the abdomen.
Understanding which stage you're dealing with is vital because the entire treatment plan is built around it. For a deeper dive into how treatment decisions are made at each stage, our guide on cholangiocarcinoma treatment guidelines can provide more clarity.
The Direct Link Between Stage and Survival
The stage at diagnosis has a massive impact on whether a cure is possible. Surgery to completely remove the tumor gives patients the best shot at long-term survival, but that's really only on the table in the earlier stages when the cancer hasn't spread.
The possibility of a cure is almost exclusively tied to early-stage diagnoses where the tumor can be surgically removed with clean margins. As the cancer advances, the focus of treatment often shifts from cure to control—extending life while maintaining its quality.
The prognosis for bile duct cancer is tied directly to the stage, and you can see this clearly in the 5-year survival rates. For patients with Stage I disease, where the tumor is localized and can be fully removed (R0 resection), the 5-year survival rate is between 35% and 45%.
For Stage II and III cancers, which have often grown into nearby tissues, the cure rate drops to around 20% to 30%. Once the cancer reaches Stage IV and has spread to distant sites, the chance of a cure, unfortunately, becomes close to zero. You can find more insights on how stage impacts cure rates on OncoDaily.
This really highlights why paying attention to symptoms and getting checked out quickly is so critical. The earlier the stage, the more options you have, and the better the chances for a good outcome.
More Than Just the Stage: Key Factors That Shape Your Prognosis
While a cancer's stage gives us a critical starting point, it's really just the broad outline of the story. To understand what the journey with bile duct cancer might look like for an individual, we have to look much deeper. Several other factors play a huge role in shaping outcomes, adding layers of detail that make every person's situation truly unique.
Think of it this way: the stage is like knowing you have to drive from New York to Los Angeles. That tells you the distance, but it doesn't tell you anything about the car you're driving, the road conditions, or the skill of the driver. Details like the tumor's exact location, the success of surgery, your overall health, and the tumor's specific genetic makeup are what really fill in the map.

Where the Tumor Starts Matters
The biliary system is complex, and where a tumor first develops has a massive impact on everything that follows—from the symptoms it causes to the treatments that are possible.
Bile duct cancers are generally grouped by their location:
- Intrahepatic Cholangiocarcinoma (iCCA): These tumors grow in the small bile ducts inside the liver. Tucked away deep in the organ, they often don't cause noticeable symptoms until they've become quite large, which unfortunately can mean a later-stage diagnosis.
- Extrahepatic Cholangiocarcinoma (eCCA): This type develops in the larger ducts outside the liver. Because they can easily block the main pipeline for bile, they often trigger earlier warning signs like jaundice (yellowing of the skin and eyes), which can sometimes lead to a quicker diagnosis.
This difference in location is directly reflected in survival statistics. Large-scale global studies have shown that 5-year relative survival for intrahepatic cancers is around 10.8%, compared to 19.9% for extrahepatic cancers. This gap is largely due to the higher likelihood of early detection and successful treatment for tumors outside the liver. You can dig into the data on these global trends in the full study published in Nature.
The Surgeon's Goal: Getting "Clear Margins"
For anyone with early-stage bile duct cancer, surgery is the single most important tool we have and offers the best shot at a cure. But the success of that surgery hinges on one crucial detail: achieving negative or "clear" margins.
A surgery with clear margins is like removing a weed along with its entire root system. If even a microscopic piece of the root is left behind, the weed can grow back. The same is true for cancer cells.
When a surgeon achieves a "clear margin," it means that when the removed tissue is examined under a microscope, the outer edge is completely free of cancer cells. This is the best-case scenario—it tells us the entire visible tumor was removed with a safety buffer of healthy tissue, which dramatically reduces the chance of it coming back. A positive margin, on the other hand, means cancer cells were found right at the edge of the tissue, suggesting some might have been left behind.
Your Overall Health and "Performance Status"
It’s not just about the cancer; it’s also about the person fighting it. Your general health going into treatment, what doctors call performance status, is a powerful predictor of your outcome. This is essentially a measure of how well you can handle daily activities and, by extension, how well your body can tolerate demanding treatments like major surgery or chemotherapy.
Patients who are active and have few other serious health problems (a good performance status) can typically handle more aggressive therapies. This opens up a wider range of treatment options and often leads to a better prognosis.
Looking Deeper: Tumor Markers and Genetics
Today’s cancer care goes far beyond what we can see on a CT scan. We now have the ability to analyze a tumor’s unique genetic fingerprint to find its specific weaknesses. This process, called biomarker testing, gives us clues that can guide treatment decisions.
Below is a quick look at some of the factors, beyond staging, that influence a patient's outlook.
Prognostic Factors in Bile Duct Cancer
Understanding these factors provides a more complete and personalized picture of the road ahead. Key markers we look for include:
- CA 19-9 Levels: This is a protein measured in the blood. While not a perfect test, a high CA 19-9 level that falls dramatically after surgery is usually a very good sign.
- Genetic Mutations: It's now standard to test tumor tissue for specific genetic changes like FGFR2 fusions or IDH1 mutations. Finding one of these isn't bad news—in fact, it's often the opposite. It opens the door to targeted therapies, which are modern drugs designed to attack the cancer cells that have that specific mutation, often leading to better results with fewer side effects than traditional chemo.
How Today's Treatments Are Changing the Outlook
Survival statistics give us a starting point, but they don't tell the whole story. The real story is about action—the steps we can take to improve those odds. Modern cancer care is all about changing the narrative, extending life, and improving its quality. The right treatment plan, started at the right time, can turn a statistical probability into a personal reality.
We've moved far beyond a one-size-fits-all playbook. Your treatment strategy will be tailored to the specifics of your cancer: its stage, its exact location, and, crucially, its unique genetic fingerprint. This personalized approach is our most powerful weapon in the fight.
Surgery: The First and Best Chance for a Cure
When we catch bile duct cancer early, surgery is our cornerstone. It offers the most direct path to a potential cure. The objective is clear and simple: get the entire tumor out before it has a chance to spread. As we touched on earlier, success hinges on achieving clear margins, which means a pathologist sees no cancer cells at the very edge of the tissue removed during the operation.
But the work doesn't necessarily end when the surgery is over. Often, what follows is a course of adjuvant chemotherapy. I like to think of this as the "cleanup crew" coming in after the main event. Even the most successful surgery can leave behind microscopic cancer cells that are too small to show up on any scan. Adjuvant chemo is designed to hunt down and eliminate these stragglers, dramatically cutting down the risk of the cancer coming back.
This one-two punch—surgery followed by chemotherapy—is a proven combination that has significantly improved outcomes for many people with resectable bile duct cancer.
Systemic Therapies: Fighting Cancer Throughout the Body
When surgery isn't an option because the cancer is too advanced, or if it has returned after initial treatment, we turn to chemotherapy. This is a systemic approach, meaning the drugs travel through your bloodstream to reach and attack cancer cells wherever they may be hiding in the body.
For a long time, the standard combination was two drugs, gemcitabine and cisplatin, which helped to slow the cancer's growth and manage symptoms. But things are always evolving. More recently, major studies have shown that for some patients, adding a third drug—paclitaxel—to that mix can extend survival even further, giving us a new, more powerful frontline option.
It's important to remember that chemotherapy works by attacking rapidly dividing cells. While this is great for targeting cancer, some of your healthy cells divide quickly, too, which is what causes side effects. A huge part of modern oncology is finding that perfect balance: maximizing the damage to the cancer while minimizing the impact on you.
The New Era of Personalized Medicine
The biggest leaps forward in improving bile duct cancer survival have come from truly understanding the tumor on a molecular level. We now know that no two bile duct cancers are exactly alike. They are driven by unique genetic mutations that act as their growth engines.
This is why molecular testing is no longer optional—it's essential. By taking a small sample of your tumor tissue, we can run a genetic analysis to map out its specific blueprint. Once we have that map, we can start looking for weaknesses to exploit.
This opens the door to two incredible classes of treatment:
Targeted Therapy: Think of these drugs as precision-guided missiles. They are engineered to seek out and attack cancer cells that have a specific genetic flaw. For instance, if a tumor has an FGFR2 fusion or an IDH1 mutation, we now have FDA-approved drugs that can specifically block the signals those faulty genes are sending. It’s like cutting the power cord to the cancer’s growth engine. This approach is not only often more effective, but it also tends to have fewer side effects than traditional chemotherapy.
Immunotherapy: This is a completely different strategy. Instead of attacking the cancer directly, immunotherapy empowers your own immune system to do the fighting. Cancer cells are clever—they develop ways to hide from the immune cells that are supposed to police the body. Immunotherapy drugs, like pembrolizumab, essentially pull off this disguise, allowing your body's T-cells to finally see the cancer and launch an attack.
In fact, adding immunotherapy to standard chemotherapy has now become a new standard of care for many people with advanced bile duct cancer, marking a massive step forward. These treatments represent a fundamental shift toward truly personalized medicine. We're no longer treating just the location of the cancer, but the very biology that makes it tick. This tailored approach is steadily improving survival and bringing new hope to patients and their families.
Navigating Advanced or Recurrent Cancer

Hearing that your bile duct cancer is advanced or has come back after treatment can feel like the ground has shifted beneath your feet. It's a moment that brings a wave of uncertainty and tough questions. When the cancer has spread to distant organs (metastatic) or returned (recurrent), the path forward changes—but it's so important to know there is a path forward.
At this stage, the primary goal of treatment often shifts from a cure to control. Think of it like managing a chronic condition, like heart disease. The focus becomes keeping the cancer in check for as long as possible, slowing its growth, and most importantly, preserving your quality of life. This perspective allows you and your oncology team to zero in on strategies that help you live better, and longer.
Exploring Second-Line Treatment Options
When the first round of treatment—what we call first-line therapy—stops working, your oncologist will start discussing second-line options. This isn't a sign that you're out of choices; it just means it's time to pivot to a new game plan. The right next step depends entirely on your specific situation, like which therapies you’ve already had and the unique molecular profile of the tumor.
For instance, if your first treatment was a standard chemotherapy regimen, trying a different one might be the next move. If earlier biomarker testing revealed a specific genetic mutation, a targeted therapy you haven't used yet could be a powerful option. This next step is a crucial part of extending bile duct cancer survival and maintaining control.
The Critical Role of Palliative Care
Many people hear "palliative care" and immediately think of hospice or end-of-life care. That’s a common and unfortunate misconception. Palliative care is specialized medical support focused on relieving the symptoms and stress of a serious illness, and it should be part of your care from day one.
Palliative care is not about giving up; it's about gaining control. It’s an extra layer of support that works alongside your cancer treatment to improve your day-to-day life by managing pain, nausea, fatigue, and other side effects.
Bringing a palliative care team on board early almost always leads to better symptom control, improved mood, and a significantly better quality of life. It makes sure that you, not just your cancer, are being treated.
Finding Hope in Clinical Trials
For patients with advanced bile duct cancer, clinical trials can be a gateway to the next generation of therapies, long before they're widely available. These research studies explore new treatments or new ways of using existing ones. Participating gives you a chance to receive a potentially more effective therapy while helping to push the science forward for future patients.
These trials are where the latest discoveries happen, testing things like:
- Targeted therapies designed for newly discovered genetic markers.
- Immunotherapy combinations that might unlock a more powerful immune response.
- Novel chemotherapy drugs that work in entirely new ways.
Your oncologist can help you find trials that might be a good fit. This is where having an expert team becomes absolutely vital.
Why a Second Opinion Is So Important
Bile duct cancer is both rare and complex. Because of this, getting a second opinion from a specialist who sees a high volume of these cases isn't just a good idea—it can be a game-changer. An expert in cholangiocarcinoma might have access to different treatment protocols, more experience with rare side effects, or know about niche clinical trials that aren't on everyone's radar. You can learn more about how specialists approach advanced disease by reading our guide on immunotherapy for Stage 4 cancer.
A second opinion can confirm your current path or open up new doors you didn't know existed, providing peace of mind that every avenue has been explored. At a specialized practice like Hirschfeld Oncology, the entire focus is on creating individualized plans for complex cases, ensuring every possible option is on the table to improve your bile duct cancer survival outlook.
Living Fully and Finding Your Support System
When we talk about improving bile duct cancer survival, it's easy to get lost in the numbers and medical jargon. But survival is so much more than that. It’s about living as well as you can, for as long as you can—and that means focusing on your entire well-being.
Your quality of life, your emotional health, and the people you surround yourself with are just as critical as the treatments you receive. This is about actively managing not just the cancer, but every aspect of your health to build a life that remains full and meaningful.
Managing Physical and Emotional Health
Bile duct cancer can bring on some really tough physical challenges. Symptoms like jaundice, debilitating fatigue, or relentless itching aren't just minor side effects; they can completely drain your energy and spirit, impacting your ability to get through the day.
This is where open, honest communication with your oncology team is key. Don't downplay what you're feeling. There are often ways to manage these symptoms, whether through specific medications, minor procedures, or simple lifestyle changes. You have to be your own best advocate.
At the same time, we can't ignore the emotional weight of it all. A cancer diagnosis can unleash a torrent of fear, anxiety, and uncertainty. Tending to your mental health isn't a luxury—it's a fundamental part of your treatment plan. This might mean talking to a therapist, exploring mindfulness, or just opening up to a trusted friend.
Your emotional well-being and your physical health are deeply intertwined. Taking care of your mind can build resilience, help you better tolerate treatment, and ultimately improve your overall quality of life.
Building Your Circle of Support
Nobody should have to walk this path alone. Think of your support system as your personal crew—a mix of family, friends, and professional resources who have your back. These are the people who can drive you to an appointment, listen without judgment, or just offer a much-needed dose of encouragement.
Sometimes, the people who love you most don't know how to help. It's okay to guide them. Giving them specific tasks or just telling them what you need can make all the difference. If you're looking for a resource to share, our guide on how to support someone with cancer offers practical advice.
Beyond your immediate circle, patient advocacy groups can be a lifeline. They connect you with a community of people who just get it in a way no one else can. They offer a sense of solidarity and a wealth of credible information that can feel incredibly empowering.
- Find Your Community: Support groups, whether online or local, let you share stories and learn from others who are on the same journey.
- Get Reliable Information: Advocacy organizations provide vetted, up-to-date information on treatments, trials, and managing your health.
- Feel Empowered: Connecting with others who understand can drastically reduce feelings of isolation and arm you with the knowledge and hope you need.
A fantastic place to start is the Cholangiocarcinoma Foundation. It’s an incredible resource for educational materials, patient support programs, and a direct connection to a community that is fighting this disease together. Finding your people can be one of the most powerful steps you take.
Frequently Asked Questions

When you or a loved one is diagnosed with bile duct cancer, the questions can feel overwhelming. We've compiled straightforward answers to some of the most pressing concerns that come up, helping you find clarity during a difficult time.
Can Bile Duct Cancer Be Cured?
Yes, a cure is possible, but it hinges almost entirely on catching the cancer early. The best chance for a cure is when the tumor is discovered at a localized stage (Stage I), before it has had a chance to spread.
In these early cases, surgeons can sometimes remove the entire tumor with clean edges, known as an R0 resection. Once the cancer has advanced, treatment goals often shift from a cure to controlling the disease, managing symptoms, and prolonging life as much as possible.
What Is the Most Important Factor for Survival?
Without a doubt, the single most critical factor for bile duct cancer survival is the stage at diagnosis. Cancers confined to the bile duct have a much better outlook than those that have spread to nearby lymph nodes (regional) or other organs (metastatic).
The reason is simple: early-stage tumors are the ones that can potentially be treated with curative surgery, which remains our most powerful tool against this disease.
Should I get a second opinion? Absolutely. Given that bile duct cancer is a rare and complex disease, seeking a second opinion is not just acceptable—it's highly recommended. Consulting with a team that specializes in cholangiocarcinoma can provide invaluable peace of mind.
A specialist can confirm your current treatment plan is the right one, suggest important tweaks, or open the door to new options like clinical trials you might not have known about. It's about making sure every stone has been turned over.
What Are Targeted Therapy and Immunotherapy?
These are two of the most exciting advancements in cancer care, moving beyond one-size-fits-all chemotherapy. Whether they are an option for you depends on the unique genetic signature of your tumor, which we discover through molecular testing.
- Targeted Therapy: Think of these as "smart drugs." They are designed to seek out and attack cancer cells that have specific genetic glitches, like FGFR2 fusions or IDH1 mutations. They work by shutting down the precise pathways these mutations use to grow.
- Immunotherapy: This approach is completely different. It doesn't attack the cancer directly; instead, it unleashes your own immune system to do the job. It effectively takes the brakes off your body's natural defenses, allowing them to recognize and fight the cancer cells.
For the right patients, these modern treatments are truly changing the game.
At Hirschfeld Oncology, we focus on building personalized treatment plans for complex cancers like cholangiocarcinoma, always aiming to improve both survival and quality of life. To learn more about how our expert team can help you or a loved one, please visit us at our blog and resource center to request a consultation.





.png)


.png)
.png)




