For decades, the primary weapons against cancer were chemotherapy and radiation—powerful but often indiscriminate. Today, we're in a new era of cancer treatment, one that works with your body instead of just acting on it. This approach is called biologic therapy, and at its heart are biologic response modifiers (BRMs).
These are not your typical drugs. BRMs are substances derived from living organisms that essentially retrain and re-energize your own immune system to fight cancer. Also known as immunotherapy, this strategy turns your body’s natural defenses into a highly targeted, cancer-fighting force.
A New Era in Oncology: Understanding Biologic Response Modifiers
Think of your immune system as a sophisticated security team patrolling your body 24/7. Normally, it's brilliant at spotting and eliminating threats. But cancer cells are clever; they've developed sneaky ways to disguise themselves or even switch off the immune system's alarms, allowing them to multiply without being noticed.

This is where biologic response modifiers step in. They’re like giving your security team advanced surveillance tech and a new set of orders. Instead of poisoning cancer cells with an outside chemical (the way chemotherapy does), BRMs give your own immune cells the tools they need to do their job better. They don't just attack the disease—they teach your body how to win the fight itself.
The Core Philosophy Behind BRMs
The fundamental idea behind BRMs is to empower the body's innate ability to heal. These therapies carry out several critical missions to shore up your anti-cancer defenses:
- Boost Immune Activity: They can act like a rallying cry, stimulating immune cells to become more aggressive and hunt down tumors more effectively.
- Improve Recognition: They help your immune system see through cancer's camouflage, marking the rogue cells for destruction.
- Restore Normal Function: They can block the "off" signals that cancer cells use to paralyze your immune response, effectively turning the system back on.
This approach is all about creating a durable, long-term defense by tapping into the most personalized weapon we have: a patient's own immune system.
By modifying, boosting, or restoring the immune system's ability to spot and eliminate cancer cells, biologic response modifiers offer a more targeted and hopeful path forward in oncology. This strategy is designed to maximize treatment effectiveness while minimizing toxicity.
Moving Beyond a One-Size-Fits-All Approach
Oncology is steadily moving away from broad-stroke treatments and toward more precise, personalized medicine. Biologic response modifiers are leading this charge. Unlike traditional therapies that can harm healthy cells in the process of killing cancerous ones, BRMs are designed with much greater specificity.
This tailored strategy allows oncologists to develop treatment plans that are uniquely suited to a patient’s specific cancer biology and overall health. For those facing advanced or complex cancers, this opens up new avenues for managing the disease and enhancing quality of life. At Hirschfeld Oncology, our specialty lies in weaving these sophisticated therapies into a holistic care plan, providing new hope when standard treatments may no longer be enough.
How Biologic Response Modifiers Train Your Body to Fight Cancer
Think of biologic response modifiers not as a brute-force attack from the outside, but as a team of strategic coaches. Their job is to teach your own immune system how to recognize, track down, and get rid of cancer cells far more effectively. They take your body's existing defenses and sharpen them, turning a general security patrol into an elite anti-cancer task force.
This "training" happens in a few clever ways. Some of these therapies act like communication experts, making sure the right messages get to the right immune cells at the right time. Others are more like targeting specialists, painting a giant bullseye on tumor cells that were hiding in plain sight. No matter the method, the end goal is always the same: to tip the scales back in your body's favor.
Sounding the Alarm and Rallying the Troops
One of the most important jobs of a biologic response modifier is to boost the communication network that your immune system relies on. Cancer is sneaky; it often thrives by silencing the very alarm signals that immune cells use to launch a coordinated attack. These therapies can break through that interference.
Certain BRMs, like cytokines, essentially act as dispatchers, sending out an urgent, system-wide alert. They crank up the volume on the distress signals, which has a ripple effect:
- Calling for backup: They recruit more immune cells to the fight, pulling powerful defenders like T-cells and natural killer cells directly to the tumor.
- Waking up sleeping guards: They activate immune cells that were dormant, making them more aggressive and ready to engage the enemy.
- Boosting stamina: They help your immune cells stay in the fight longer, preventing the exhaustion that can happen during a prolonged battle with cancer.
This supercharged communication ensures the threat isn't just noticed—it's met with a strong and sustained counter-attack from your body’s best defenders.
Marking the Target for Precision Strikes
Another brilliant tactic is simply making cancer cells easier for the immune system to see. Cancer cells are masters of disguise, often covering themselves with proteins that make them look like any other normal, healthy cell. This camouflage is what allows them to fly under the radar and multiply without being stopped.
Biologic response modifiers essentially strip away this disguise. They function like highly specific guided missiles or smart keys, engineered to lock onto unique proteins—known as antigens—found on the surface of cancer cells.
This mechanism, famously used by monoclonal antibodies, achieves a few things at once. By latching onto a cancer cell, the therapy acts like a bright red flag, signaling to the immune system, "This is the enemy—attack here!" This process turns the cancer cell into an unmistakable target. The beauty of this approach is its precision; the immune assault is focused right where it's needed, sparing healthy tissue from collateral damage. For a deeper look at these mechanisms, you can explore how immunotherapy works for cancer.
Disrupting Cancer's Growth and Survival Signals
Beyond just flagging cancer cells for destruction, some biologic response modifiers go a step further by directly messing with the internal machinery cancer needs to survive and grow. They can physically block the critical growth signals that tumors depend on, effectively cutting off their fuel supply.
Picture a cancer cell that’s constantly getting "grow and divide" messages from its surroundings. A BRM can be designed to jam that signal by blocking the receptor that receives it—it’s like putting the wrong key in a lock so the right one can’t get in. This simple action can:
- Stop cell division: It prevents the cancer cells from making more copies of themselves.
- Trigger cell death: By cutting off essential survival signals, it can tell the cancer cell to self-destruct.
- Starve the tumor: Some of these therapies can stop a tumor from building new blood vessels, which it needs to get nutrients to grow.
By getting in the way of these vital processes, biologic response modifiers don't just help your immune system fight—they actively weaken the cancer itself, making it an easier and more vulnerable target.
The Major Classes of Biologic Response Modifiers
The term "biologic response modifiers" isn't one single thing but a whole category of sophisticated therapies. It's best to think of it as an oncologist's specialized toolkit, where each tool is designed for a very specific job. Once you understand these different classes, you can see how a treatment plan is built around the unique details of a person's cancer.
This strategic variety is what allows us to create highly personalized treatment plans. Each class of BRMs offers a different way to empower your immune system, turning it into a precision weapon against cancers like pancreatic, breast, and colorectal cancer.
Cytokines: The Signal Boosters
Cytokines are the communications officers of your immune system. They're proteins your body naturally makes to carry messages between cells, coordinating a powerful and effective response against threats. In cancer therapy, we use lab-made versions of these proteins to amplify those signals, essentially turning up the volume on the immune system's alarm bells.
Imagine your immune cells are firefighters. Cytokines are the dispatchers shouting through the radio, "There's a five-alarm fire over here! All units respond immediately!" They don't fight the fire themselves, but they make sure the response is swift, strong, and overwhelming.
Two main types of cytokines used in oncology are:
- Interferons: These help the immune system recognize and attack cancer cells and can also slow a tumor's growth directly.
- Interleukins: These ramp up the growth and activity of key immune cells, especially the powerful T-cells and B-cells that are so critical for destroying tumors.
Monoclonal Antibodies: The Guided Missiles
Monoclonal antibodies are one of the most widely used types of BRMs today. These are lab-engineered versions of the antibodies your body already produces, but they’re designed with a single, highly specific mission: to find and attach to a particular protein (called an antigen) on the surface of a cancer cell.
Think of them as guided missiles programmed with the exact coordinates of an enemy target. They circulate through the body, ignoring healthy cells until they find the one specific marker they’ve been built to hit. Their precision is their greatest strength.
Once they lock onto their target, they can fight cancer in a few different ways:
- Marking for Destruction: By latching onto a cancer cell, they act like a bright red flag, making it easy for other immune cells to find and destroy it.
- Blocking Growth Signals: Some can physically block the receptors on a cancer cell that tell it to grow and divide, effectively cutting off its command signals.
- Delivering Treatment Directly: Certain antibodies are linked to chemotherapy drugs or radioactive particles, a combination known as an antibody-drug conjugate. This allows them to carry a toxic payload directly to the tumor while minimizing damage to surrounding healthy tissue.
The success of these therapies is driving huge growth in oncology. Monoclonal antibodies hold a 56.48% share of the entire biologics market. The overall BRM sector is projected to grow from USD 141,104.47 million to USD 203,903.68 million by 2031, with oncology treatments making up 40% of that expansion.
This growth reflects real benefits for patients. For example, in certain HER2-positive metastatic breast cancer cases, the antibody-drug conjugate ado-trastuzumab emtansine improved median overall survival to 29.9 months compared to 25.1 months with standard care.
This infographic shows the core actions these therapies use to empower your body's defenses.
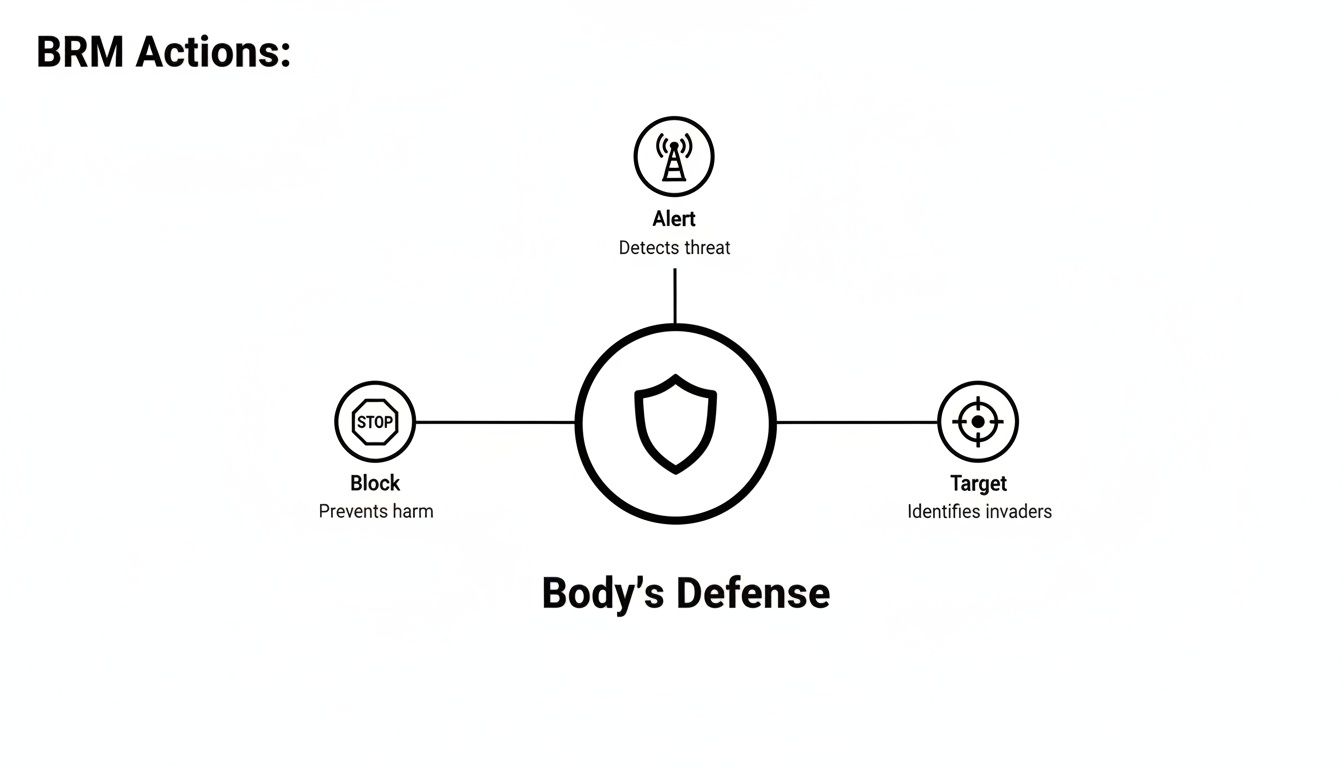
As you can see, BRMs alert the immune system, block harmful cancer pathways, and directly target invading cells to strengthen the body's natural defense shield.
To provide a clearer overview, the table below summarizes the key classes of BRMs and their roles in cancer treatment.
Key Classes of Biologic Response Modifiers and Their Roles
This table helps illustrate how each type of therapy brings a unique strategy to the fight, allowing oncologists to choose the right approach for the right cancer.
Immune Checkpoint Inhibitors: The Brake Removers
Your immune system has natural "brakes," or checkpoints, that keep it from becoming overactive and attacking your own healthy cells. It’s a crucial safety feature. The problem is, some cancer cells have figured out how to exploit this system. They produce proteins that hit those brakes, effectively shutting down the very T-cells that should be attacking them.
Immune checkpoint inhibitors are drugs that block this devious interaction. They don't boost the immune system directly; instead, they release the brakes that the cancer has applied. This frees up the T-cells to get back to work recognizing and destroying the tumor. It’s like a security guard finally realizing the person trying to shut down the alarm system is actually a burglar.
This approach has been a game-changer for several hard-to-treat cancers. By unleashing the immune system's own power, these therapies can produce durable, long-lasting responses in some patients.
Cell Therapies: The Living Drugs
Among the most advanced BRMs are cell therapies, where we actually harvest a patient's own immune cells and re-engineer them to become supercharged cancer killers. The most well-known example of this is CAR-T cell therapy.
Here’s how it works:
- We start by collecting a patient's T-cells from their blood.
- In a specialized lab, these T-cells are genetically modified to produce special receptors on their surface called chimeric antigen receptors (CARs).
- These CARs are custom-designed to recognize and latch onto the specific antigens on that patient's cancer cells.
- Millions of these new, engineered CAR-T cells are grown in the lab and then infused back into the patient.
These modified cells are often called "living drugs" because they can multiply inside the body and continue hunting down cancer cells for months or even years. This provides a long-term, vigilant defense system against the disease. It’s a remarkable step forward in personalized oncology. For a deeper dive into one of the core technologies behind this, you can read our guide that explains how monoclonal antibodies work.
Comparing BRMs with Traditional Cancer Treatments
To really understand what makes biologic response modifiers (BRMs) so different, it helps to see how they stack up against the cancer treatments that came before them. Each one has a completely different philosophy for fighting the disease. Imagine you’re trying to take down an enemy fortress—there are several ways to go about it.
Traditional chemotherapy is a lot like a widespread bombing campaign. Its goal is to destroy any and all rapidly dividing cells, which is a hallmark of cancer. While it can be very effective at hitting the enemy, this approach always causes significant collateral damage. It harms healthy, fast-growing cells in your hair follicles, digestive tract, and bone marrow, which is why its side effects are so well-known.
Targeted therapy is more like sending in a skilled sniper. These drugs are engineered to find and disable specific molecules that cancer cells need to grow and spread. This is a much more focused attack than chemotherapy, but it has a catch: it only works if the cancer has the exact target the sniper is trained to hit.
Biologic response modifiers are a whole new game plan. They aren't the weapon; they're the intelligence officers and elite trainers. Instead of launching a direct, outside attack, their job is to train, equip, and empower the body's own defense forces—the immune system—to carry out a highly precise and self-sustaining mission against the cancer.
A Focus on Specificity and Collateral Damage
The fundamental difference here boils down to how each treatment tells friend from foe. Chemotherapy’s broad-spectrum attack leads to that familiar list of side effects, while targeted therapy, though more precise, can still have off-target effects.
BRMs, by working through the immune system, offer a unique level of precision. Your immune system is already a genius at telling "self" from "non-self." BRMs just give it the boost or the intelligence it needs to do its job better against cancer, leading to an entirely different set of side effects that are usually related to a revved-up immune system, not widespread cell death.
This strategic shift is more than just a scientific detail; it has a massive impact on a patient's quality of life. For oncologists who prioritize low-toxicity regimens, BRMs can reduce severe adverse events by 30-50% compared to chemotherapy.
This improvement means more patients can keep up with their daily lives and maintain their strength during treatment. We've seen this play out in real-world scenarios. For example, data from metastatic breast cancer studies showed how HER2-targeted BRMs like trastuzumab extended median survival from 20.3 to 25.1 months. With thousands of clinical trials now exploring these therapies for even the toughest cancers, their potential to improve both survival and well-being is only growing. You can learn more about this trend by reviewing market research on cancer biological therapy.
Comparing the Three Main Approaches
To make these differences crystal clear, let's lay them out side-by-side. The table below gives you a quick snapshot of how biologic response modifiers, chemotherapy, and targeted therapy compare. It’s a great starting point for having more informed conversations with your oncologist about the best path forward for you.
Treatment Approaches at a Glance BRMs vs Chemotherapy vs Targeted Therapy
As the table shows, while every cancer treatment has potential side effects, the source of those side effects is what's different. The side effects from BRMs come from a newly activated immune system doing its job, sometimes a little too enthusiastically. In contrast, chemotherapy’s side effects come from direct damage to healthy tissues. Understanding these distinctions is a huge part of making collaborative decisions with your care team about a treatment plan that fits your health goals and your life.
Your Guide to Navigating Biologic Response Modifier Therapy
Starting any new treatment can be overwhelming, but you're not going into this alone. Think of it as a partnership. By understanding what to expect and what questions to ask, you become an active, empowered member of your own cancer care team.
Let's walk through how you can prepare for your journey with biologic response modifiers (BRMs) and manage your treatment with confidence.
This process is a two-way street between you and your oncology team. Your personal insights—how you feel day-to-day—are just as critical as any lab result or scan. Our goal is to give you the tools and knowledge to navigate your therapy with clarity.
Key Questions to Ask Your Oncologist
Your first few appointments are the best time to lay a solid foundation of understanding. I always encourage my patients to bring a list of questions; there's no such thing as a silly one. Getting clear answers helps set realistic expectations and makes the entire process feel less intimidating.
Here are a few great starting points for that conversation:
- How will we know it's working? Ask about the specific tests, like blood work or imaging scans, that will be used and how often you'll have them.
- What side effects should I really watch for? While we can talk about general side effects, your oncologist can pinpoint the most common ones for your specific BRM.
- What does a treatment day look like? Get clarity on whether it's an IV infusion, an injection, or a pill, and understand the schedule for each cycle.
- Who is my point of contact for problems? Make sure you know exactly who to call—and when—if you start feeling unwell or have a reaction between visits.
Being your own best advocate means asking questions until you feel comfortable and confident in the plan. That open dialogue is the key to a strong patient-doctor relationship and a smoother treatment journey.
Proactively Managing Potential Side Effects
Because BRMs work by revving up your immune system, their side effects often look quite different from chemotherapy. In many ways, they're signs that the treatment is doing its job, but they absolutely need to be managed.
The most important thing you can do is communicate with your care team. Don't ever brush off a symptom as being too minor to mention. What seems like a small issue could be an early warning sign that needs attention.
Here are some common side effects and a few practical tips:
- Fatigue: This is a big one. Be kind to yourself. Prioritize rest, try short naps, and see if gentle activity like a short walk can actually boost your energy.
- Skin Issues: Rashes, dryness, and itching are common. Stick to gentle, fragrance-free lotions and let your team know right away if any skin changes become severe or painful.
- Flu-Like Symptoms: It's not unusual to experience chills, fever, and muscle aches, especially right after a treatment. Your doctor can often recommend over-the-counter options to help.
The impact of these therapies is truly remarkable. For some ovarian cancers, BRMs can extend progression-free survival by 6-12 months. Better yet, their side effect profiles are often manageable enough that 80% of patients can continue with their normal daily activities.
With over 50 FDA-approved BRMs for solid tumors, millions of patients across the U.S. now have access to these powerful and often less toxic treatments. You can learn more about their growing role in oncology by exploring the biologic response modifier market and its impact.
How Hirschfeld Oncology Personalizes Your Treatment
Knowing the science behind these advanced therapies is just the starting point. The real work—and where we excel—is in applying that science to your individual cancer journey. At Hirschfeld Oncology, we move beyond standard protocols to deliver true precision medicine.
It all begins with a deep dive into your unique cancer biology. Dr. Hirschfeld and our team use this information to build a treatment plan from the ground up, specifically for you. We often integrate these sophisticated therapies to manage complex, advanced-stage cancers, always focusing on creating effective, low-toxicity regimens that aggressively target the disease while protecting your quality of life.
Collaborative and Adaptive Care
Your treatment isn’t a one-time prescription; it's a dynamic, evolving process. We firmly believe in collaborative decision-making. Your voice, your concerns, and your well-being are at the heart of every choice we make together. This partnership is built on a bedrock of open communication and careful oversight.
We are constantly monitoring how you're responding to treatment, ready to make real-time adjustments. This flexibility allows us to maximize the therapy's impact and get ahead of side effects, ensuring your care plan adapts right alongside you.
Delivering this level of personalized care requires a seamless back-end operation. For a practice like ours, flawlessly managing patient data and clinic workflows is essential for efficiency and optimal outcomes. To see how these systems work, you can explore this guide on integrated EMR and practice management.
A Beacon of Hope in Brooklyn
For patients here in Brooklyn and the surrounding areas navigating a diagnosis of pancreatic, colorectal, or breast cancer, our approach represents a meaningful path forward. We offer hope by blending decades of hands-on experience with an unwavering commitment to patient-first care.
We encourage you to request a consultation with our team. Let's sit down and explore how advanced biologic response modifiers can be woven into a comprehensive plan that prioritizes your health today and your future tomorrow. To learn more about our specific methods, you can read about our approach to immunotherapy at Hirschfeld Oncology.
Frequently Asked Questions About Biologic Response Modifiers
When you're facing a new treatment plan, questions are completely normal. Getting clear, straightforward answers is the first step toward feeling more in control and prepared for the journey ahead. Here are a few of the most practical questions we hear from patients about biologic response modifiers.
How Long Will I Need BRM Therapy?
This is a very common question, and the honest answer is: it truly depends. There’s no single timeline for treatment with biologic response modifiers. The duration is shaped entirely by your specific cancer, the drug we choose, how your cancer responds to it, and how you feel on the therapy.
For some, treatment might continue for as long as it's working and the side effects are easy to manage. For others, we may plan for a specific number of cycles or a set period of time. Your oncologist will map out a personalized schedule for you from the start and will always be ready to adjust it based on your progress and how you're doing.
Are Biologic Response Modifiers Covered by Insurance?
This is a critical, and often stressful, question. The good news is that most insurance plans, including Medicare, generally do cover FDA-approved biologic response modifiers for cancer. These treatments are now a core part of modern cancer care.
Of course, the details always come down to your specific plan, diagnosis, and the prescribed therapy. Our team has years of experience handling the insurance approval process. We make it a priority to help you understand your coverage and any potential costs before your first treatment, so there are no surprises. If you're curious about the technical side of organizing information like this, you can learn about tools like how to build an FAQ bot that help deliver answers efficiently.
Can BRMs Be Combined with Other Cancer Treatments?
Absolutely. In fact, that’s one of their greatest strengths. BRMs are very often used as part of a multi-part strategy. We can pair them with other treatments like low-dose chemotherapy, targeted therapy, or radiation to launch a more effective, coordinated attack on the cancer.
A combined approach often works better than any single therapy on its own. For instance, a biologic response modifier might "unmask" cancer cells, making them more susceptible to chemotherapy. This can lead to better results, often with lower and more tolerable chemo doses.
At Hirschfeld Oncology, creating these smart, integrated treatment plans is what we do. We carefully design every regimen based on your unique cancer biology, always aiming to maximize results while protecting your quality of life.
At Hirschfeld Oncology, we believe an informed patient is an empowered patient. If you have more questions about biologic response modifiers or want to discuss what personalized cancer care could look like for you, we encourage you to request a consultation. You can also learn more about our philosophy on our blog at https://honcology.com/blog.





.png)


.png)
.png)




