A bone marrow biopsy is a procedure where your doctor takes a small sample of the soft, spongy tissue inside your bones to get a closer look at your blood cell production. This tissue, the bone marrow, is where all your blood cells are made. The sample is then sent to a lab and examined under a microscope to help diagnose blood disorders, stage certain cancers, or check if a treatment is working. It gives us a level of detail that a simple blood test just can't provide.
A Look Inside Your Body's "Blood Cell Factory"

Hearing you need a bone marrow biopsy can be intimidating, but knowing what to expect can make all the difference. The best way to think about it is to picture your bone marrow as the "factory" inside your larger bones that constantly manufactures your blood cells—the red cells, white cells, and platelets.
Sometimes, we need to go directly to the source to understand what’s going on. A bone marrow biopsy procedure is how we take a tiny, direct sample from this factory floor to see how well it's running and inspect the cells it’s producing.
Aspiration vs. Core Biopsy: Two Sides of the Same Coin
The procedure almost always involves taking two different kinds of samples, one right after the other. This two-part process gives your medical team a complete picture of your marrow's health.
- Bone Marrow Aspiration: This part comes first. We use a thin needle to draw out a small amount of the liquid portion of your bone marrow. This fluid is rich with developing blood cells and provides a snapshot of the individual "workers" in the factory.
- Core Biopsy: Right after the aspiration, we use a slightly different needle to collect a tiny, solid piece of the spongy bone marrow tissue itself. This sample keeps the marrow's architecture intact, showing us the "factory floor" and how all the cells are organized.
A good analogy is checking on a beehive. The aspiration is like sampling the honey (the liquid), while the core biopsy is like taking a small piece of the honeycomb (the structure). You really need both to understand the full story.
For an oncologist, getting both the aspiration and core biopsy samples is non-negotiable. It’s like having a detailed blueprint of your cellular health, giving us the critical information needed to build the most effective and personalized treatment plan for you.
Why Both Samples are So Important
Each sample gives us a unique piece of the diagnostic puzzle.
The liquid from the aspiration is perfect for identifying the different types of cells, counting them, and seeing if there are any abnormal ones. It’s what we use for precise cell counts and many genetic tests.
The solid core biopsy sample, on the other hand, shows us the marrow’s “cellularity”—basically, how crowded or empty the factory is. It reveals if the marrow has been taken over by cancer cells or replaced by scar tissue. This structural view is essential for staging diseases like lymphoma or seeing if another cancer, like breast cancer, has spread to the bones.
By taking both, we leave no stone unturned. We get a comprehensive look at your health, from the individual cells to the overall structure of the marrow itself.
Why We Need to Look Deeper: The Reason for a Bone Marrow Biopsy
If your oncologist has recommended a bone marrow biopsy, it’s because we need to get a look at something incredibly important that other tests just can’t show us. Think of it this way: a regular blood test is like looking at the cars on a highway. It tells us how many there are and what types are passing by, which is useful information. But a bone marrow biopsy takes us directly to the factory where those cars are being built.
Inside that factory—your bone marrow—we can see exactly what’s happening on the assembly line. It's the only way to get a direct, unfiltered view of your blood cell production, and that view is often critical for getting your diagnosis right and crafting the most effective treatment plan.
Getting to the Bottom of Abnormal Blood Counts
One of the most common reasons we perform this procedure is to investigate abnormal results from a routine blood test. When your red blood cell, white blood cell, or platelet counts are persistently off—either too high or too low—we need to find out why.
Is your marrow factory working overtime and churning out too many faulty cells, as we see in leukemia? Or has production slowed down or stopped, which might point to conditions like aplastic anemia or myelodysplastic syndrome (MDS)? A biopsy is the only way to get the definitive evidence we need to tell the difference.
It's not just a numbers game, though. We’re also assessing the quality of the cells. The samples we collect allow our pathologists to examine the size, shape, and maturity of the cells under a microscope. This detailed look tells us if your blood cell production is running smoothly or if there's a serious issue that needs immediate intervention.
Staging Cancer and Tracking Your Progress
Beyond making an initial diagnosis, a bone marrow biopsy is essential for staging certain cancers. For blood cancers like lymphoma or multiple myeloma, it answers a crucial question: has the cancer moved into the bone marrow? The answer directly influences the stage of the disease and how we approach treatment.
The same is true for cancers that start in other parts of the body, like the breast, colon, or lung. Sometimes, these cancers can spread (metastasize) to the bone marrow. A biopsy is the gold standard for confirming whether this has happened, which is a game-changer for your overall treatment strategy.
A bone marrow biopsy gives us the blueprint for your care. It reveals the unique characteristics of the cancer cells, right down to their genetic markers. This allows us to choose therapies specifically designed to target your cancer's weaknesses.
This detailed blueprint is also our guide for monitoring how well your treatment is working. By comparing a biopsy taken after a round of therapy to the one we took at the beginning, we can see the real-world impact of your treatment. This allows us to make smart, timely adjustments to keep you on the most effective path.
Furthermore, we can analyze the genetic markers on the marrow cells, which gives us powerful insights. Understanding these specific identifiers helps us pinpoint the most effective targeted therapies. You can learn more about how these identifiers are revolutionizing cancer treatment in our guide on what cancer biomarkers are.
This table breaks down some of the most common reasons we perform a bone marrow biopsy here at Hirschfeld Oncology.
The ability of this procedure to provide such precise diagnostic information is why it's a cornerstone of modern oncology. Its importance is reflected in market trends, with the global bone marrow biopsy market valued at USD 1.10 billion in 2021 and projected to hit USD 1.79 billion by 2029. This growth is a direct result of its indispensable role in both diagnosing blood disorders and staging metastatic cancers, as highlighted in reports about the expanding role of this diagnostic tool from Data Bridge Market Research.
Ultimately, a bone marrow biopsy provides the clarity we need to move forward with confidence, ensuring every decision we make is based on a deep and accurate understanding of what’s happening inside your body.
How to Prepare for Your Biopsy Appointment
A smooth bone marrow biopsy really starts with good preparation. Taking a few simple steps beforehand can make a huge difference, helping you feel less stressed and more in control. Think of it as handling the logistics ahead of time so you can just focus on yourself on the day of the procedure.
The most important first step? A good, clear conversation with your care team. This is your time to go over your complete medical history and, crucially, every single medication you're taking. That includes prescriptions, over-the-counter drugs, vitamins, and even herbal supplements.
Discuss Your Medications and Health History
Some common medications can interfere with blood clotting, which is something we need to manage carefully for a biopsy. It’s essential that you tell your doctor if you take any of the following:
- Blood thinners (like aspirin or warfarin)
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen
- Insulin or other medications for diabetes
Your oncologist might need to tweak your dose or ask you to pause a medication for a short time before the procedure. It's also vital to let us know about any allergies you have, especially to numbing agents like lidocaine. This open line of communication is all about keeping you safe and avoiding any potential issues.
Preparing for a procedure is a team effort. When you openly discuss your medications and ask questions, you become an active partner in your care. This helps us manage every detail for your safety and comfort.
This conversation is also the perfect chance to clear up any questions still on your mind. Feeling informed is one of the best ways to ease anxiety. If you need a little help getting started, check out our list of important questions to ask your oncologist.
Logistics and Comfort on the Day of Your Procedure
Once the medical details are squared away, you can turn your attention to the practical side of things for the day of your appointment. These small things can make a big impact on your experience.
Arrange Your Transportation
You'll most likely be given a sedative to help you relax and stay comfortable. Because this medication will make you drowsy, you must arrange for someone to drive you home. Don't leave this to the last minute—confirm your ride ahead of time. You won’t be able to drive, operate machinery, or drink alcohol for the rest of the day.
Eating and Drinking
Your doctor will give you specific instructions about food and drink. Sometimes, you might be asked to fast for a few hours beforehand. Just be sure to get clear guidelines from your clinical team so you know exactly what to do.
What to Bring with You
Keep things simple. Wear loose, comfortable clothes. Bring a list of your medications, your insurance card, and an ID. It’s also a good idea to bring something to help you relax while you wait, like a book, music, or a podcast. Your job is just to stay as calm and comfortable as possible.
What Happens During the Procedure Step by Step
Walking into a procedure like a bone marrow biopsy can feel intimidating. Knowing exactly what will happen, moment by moment, can make all the difference. The good news is that the entire process is surprisingly quick—we're usually done in less than 30 minutes. Our team at Hirschfeld Oncology is committed to keeping you comfortable and informed every step of the way.
This simple flowchart lays out the main things to take care of before you even arrive at our clinic.
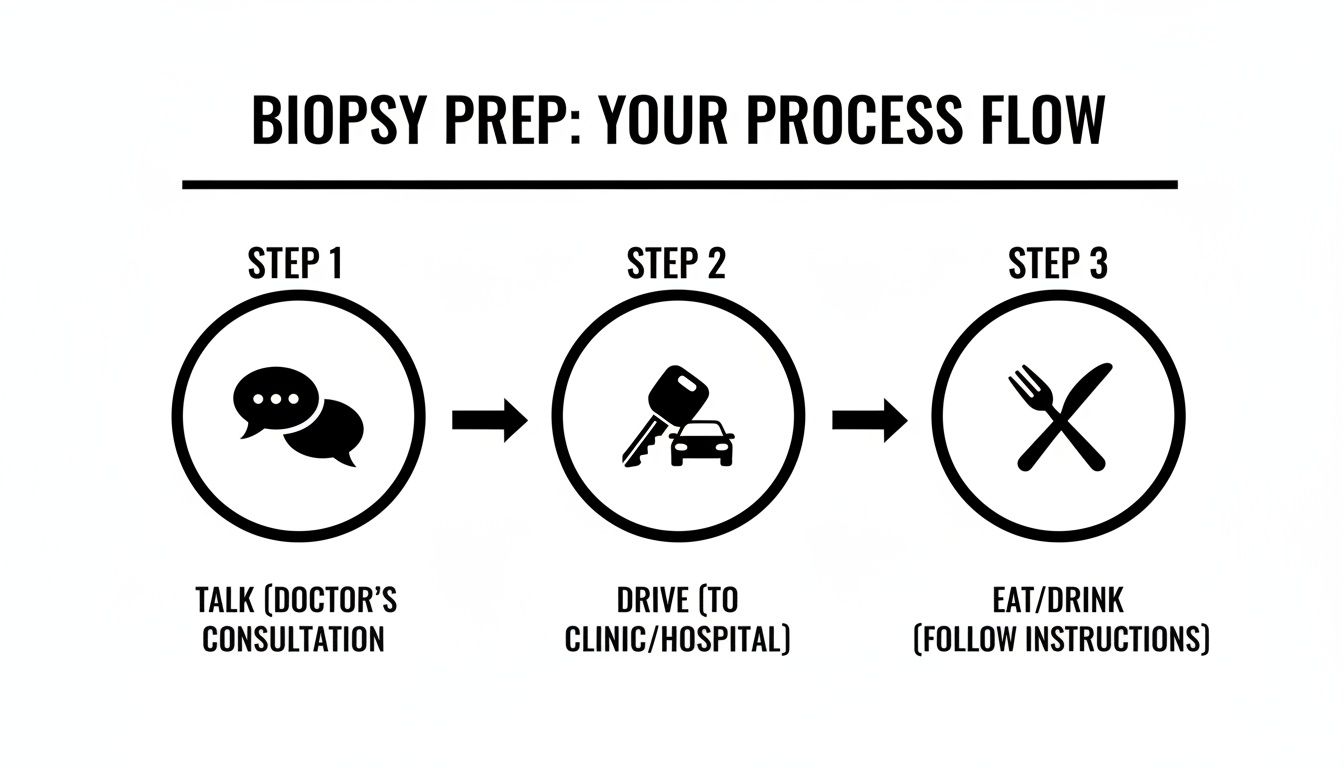
Taking care of these details beforehand—like discussing your medications, arranging for a ride, and knowing whether you can eat or drink—helps ensure everything goes smoothly on the day of your biopsy.
Getting Positioned and Numbed
When you're settled in the procedure room, we'll have you lie down, usually on your stomach or side. This position gives us the safest and most direct access to the back of your hip bone, a spot called the posterior iliac crest. It's the standard site for this procedure.
First things first, we'll clean the skin over your hip with an antiseptic solution. It might feel a bit cold, but it’s a quick and essential step to keep everything sterile.
Next comes the part that ensures your comfort: numbing the area. We use a local anesthetic, much like the novocaine you get at the dentist. We'll inject it into the skin and down to the surface of the bone. You’ll probably feel a brief sting or a slight burning sensation as the medicine goes in, but that feeling disappears quickly as the numbness takes over.
The Aspiration and Biopsy Process
Once we're certain the area is completely numb, your doctor will make a tiny incision in the skin. It’s just large enough for the special biopsy needle to pass through. You might feel some movement, but you shouldn't feel any pain.
The actual collection happens in two distinct parts.
The Aspiration: A thin needle is guided through the hard outer layer of the bone into the soft marrow inside. A syringe is then attached to draw out a small sample of the liquid marrow. This is the part where most people feel a strange, dull ache or a deep pulling sensation. It only lasts for a few seconds, but it's a unique feeling. We’ll let you know right before it happens.
The Core Biopsy: Right after the aspiration, we use a slightly different needle to get the solid sample. The doctor will gently twist the needle to capture a tiny, solid cylinder of marrow tissue. Just like with the aspiration, you'll likely feel pressure, but not sharp pain.
We believe in constant communication. We will talk you through every single step, telling you what we’re doing and what you can expect to feel next. Your peace of mind is just as important as your physical comfort.
The collection itself only takes a few minutes. We encourage you to focus on your breathing and tell us how you're doing. Our team is right there with you, and we can always add more anesthetic or simply pause to give you a moment.
Finishing the Procedure
As soon as both samples are collected, the needle is removed. We'll immediately apply firm pressure to the site with a sterile dressing to make sure there's no bleeding. After holding pressure for a few minutes, we'll place a secure bandage over the area.
And that’s it—the biopsy itself is done. We'll have you rest for a little while so we can monitor the site and make sure you're feeling okay. Then, we'll go over the aftercare instructions, and you'll be all set for your ride home. The whole appointment is designed to be as efficient and comfortable as possible.
Your Recovery and Aftercare Plan
Once the biopsy is done, we'll shift our focus entirely to making sure you have a smooth, comfortable recovery at home. The great news is that the aftercare is usually pretty simple, and most of our patients are back to their normal rhythm in no time. We’ll give you a detailed set of instructions before you head home, but here’s a look at what you can generally expect.
For the first 24 to 48 hours, your only jobs are to rest up and keep the biopsy site clean and dry. We'll place a secure bandage over the area, and you'll need to leave it on for at least the first 24 hours. That means no showers, baths, or swimming during that initial window—we want to keep moisture away to prevent any chance of infection.
Managing Discomfort and Activity
It’s completely normal to feel some soreness at the biopsy site, almost like a deep bruise. This is typically mild and easily handled with over-the-counter pain medicine like acetaminophen (just be sure to use what your doctor has approved). Applying an ice pack for 15-20 minutes at a time can also do wonders for any swelling or tenderness.
Plan on taking it easy for the first day. This isn't the time for heavy lifting, a hard workout, or any strenuous physical tasks. A gentle walk is perfectly fine, but the most important thing is to listen to your body. If you were given a sedative for the procedure, you absolutely cannot drive, operate machinery, or drink alcohol for the rest of that day.
Your body needs a moment to heal. The best thing you can do for a quick, uneventful recovery is to give yourself permission to simply rest for a day.
What to Watch For After Your Procedure
Complications are quite rare, but it's always wise to know what to look for so you can act quickly if anything seems unusual. Bone marrow biopsies have an excellent safety record, which is why they are such a vital tool in cancer care. In fact, a study of 1,252 procedures found the complication rate was just 6.15%, with most issues being minor pain or bleeding. You can explore the full study on bone marrow biopsy safety to get a better sense of its reliability.
Give our office a call right away if you notice any of the following:
- Bleeding: The site is bleeding through the bandage and doesn't stop when you apply firm pressure.
- Signs of Infection: You see increasing redness, swelling, or warmth, or any pus-like drainage from the site.
- Fever: Your temperature hits 100.4°F (38°C) or higher.
- Severe Pain: You’re experiencing discomfort that isn't getting better with your approved pain medication.
Again, these symptoms are uncommon, but your health is our top priority. Never hesitate to reach out if you're concerned about anything. We’re here to support you every step of the way, and that includes your recovery at home.
Understanding Your Biopsy Results
The waiting period after your bone marrow biopsy is often the toughest part. During this time, your samples are in the hands of a pathologist—a doctor who specializes in analyzing cells and tissues. They'll meticulously examine your marrow under a microscope and run a series of advanced tests, compiling everything into a detailed pathology report.
At first glance, this report can feel overwhelming, packed with medical language that looks like a foreign tongue. But it's far more than just a technical document. Think of it as a detailed blueprint of what's happening inside your bones, giving your oncologist the crucial information needed to confirm a diagnosis and build a treatment plan specifically for you.
Translating the Language of Your Report
While your oncologist will sit down with you and explain everything, it can be empowering to familiarize yourself with some of the key terms you might see. This helps you follow along and ask more informed questions.
Cellularity: This simply refers to how "full" or "empty" your bone marrow is with blood-forming cells. In a healthy young adult, the marrow is about 50% cells and 50% fat. The report will note if your marrow is hypercellular (more crowded than expected) or hypocellular (less crowded), which can point to different conditions.
Dysplasia: This is a word pathologists use to describe cells that look abnormal—maybe they're the wrong size, shape, or just don't look mature. Seeing dysplasia can be an early clue for certain disorders, such as myelodysplastic syndrome (MDS).
Blasts: These are the most immature, baby-faced blood cells in the marrow. It’s perfectly normal to have a few, typically less than 5%. A higher number, however, can be a red flag for conditions like leukemia.
These are just a few of the core findings that help build the diagnostic picture. If you'd like to get more comfortable with these documents, we've put together a guide on how to read a pathology report that breaks things down even further.
Your pathology report is the cornerstone of personalized medicine. It translates the microscopic details of your cells into a clear, actionable roadmap that allows us to target your specific condition with precision and confidence.
How Your Results Shape Your Treatment Plan
Every single detail in that report directly influences your path forward. Your oncologist uses this information to do more than just name a condition; they use it to understand its aggressiveness or stage. For instance, the number of cancer cells found in the marrow can help stage a lymphoma, while identifying specific genetic markers can tell us exactly which targeted therapies will be most effective.
This is precisely why the bone marrow biopsy is such an indispensable tool in modern oncology. The insights we gain are becoming more powerful every year as technology advances. In fact, the market for bone biopsy systems is expected to reach USD 507.1 million by 2035. Needle biopsies are absolutely essential for confirming cancer in 42.2% of cases involving bone disease.
Ultimately, your results do one incredibly important thing: they turn uncertainty into a clear, hopeful path forward.
Answering Your Questions About the Procedure
Even with a good overview, it's natural to have more questions pop into your head. Let's walk through some of the most common things patients ask us. We want to clear up any lingering concerns so you can feel confident and prepared.
Does a Bone Marrow Biopsy Hurt?
This is usually the very first question people ask, and it's a completely valid concern. The short answer is that we do everything possible to minimize discomfort.
First, we thoroughly numb the area on your hip with a local anesthetic, much like what a dentist uses. You’ll feel a quick sting from the injection, but that fades fast as the area goes numb.
During the actual procedure, most patients describe feeling a sense of deep pressure or an odd, brief pulling sensation. It's not typically a sharp or intense pain. Afterwards, you can expect the site to be sore for a few days, almost like a deep bruise. This is usually managed easily with over-the-counter pain relievers.
How Long Does It Take to Get Results?
The waiting period can be the hardest part, and the timeline really depends on which tests the pathologist needs to run on the sample.
Sometimes, we can get a preliminary idea of what's going on within a few days from the initial look under the microscope. But for a complete and accurate diagnosis, a deeper analysis is almost always needed.
- Standard Pathology: A full, detailed report usually takes several days.
- Specialized Testing: More complex tests, like genetic or molecular analysis, can take one to two weeks to come back.
Your care team will give you a clear timeline for your specific case and will call you the moment we have the results to discuss. We know how stressful this time is, and we're committed to getting you answers as quickly as we can.
A bone marrow biopsy is considered a very safe procedure with a low risk of serious complications. The most common issues are minor, such as localized bruising, bleeding, or soreness, which resolve on their own.
Can I Drive Myself Home Afterwards?
This is an important safety question. Whether you can drive depends entirely on if you receive sedation.
If you only have the local anesthetic (the numbing injection), you should be perfectly fine to drive yourself home. However, many people opt for a mild sedative to help them relax. If you receive any type of sedation, you absolutely cannot drive. You will need to arrange for a friend or family member to take you home, as the medication will make you drowsy and impair your reflexes. It's always a good idea to have a ride planned, just in case.
What Are the Risks Involved?
Rest assured, a bone marrow biopsy is a routine and very safe procedure. The chance of a serious complication is extremely low. The issues we do see are almost always minor and easy to manage.
Here’s what you can realistically expect:
- Bruising and Bleeding: A bruise at the biopsy site is very common. More significant bleeding is rare, and we handle it by applying firm pressure.
- Soreness: As we mentioned, you can expect some mild to moderate soreness for a few days.
- Infection: This is very rare. We prevent this by carefully sterilizing your skin before we begin.
Because serious complications are so uncommon, this remains one of the most reliable and essential tools we have for getting a clear diagnosis.
At Hirschfeld Oncology, our commitment is to make sure you feel informed and supported through every step of your journey. If you have more questions or are ready to schedule a consultation, please contact our team. You can find more information and resources on our blog.





.png)


.png)
.png)




