Think of cancer as a complex lock. In the past, we often had to try many different keys—treatments like chemotherapy—hoping one would fit. But what if you could get a blueprint of the lock itself to find the one perfect key?
That’s essentially what cancer biomarkers do. They are like unique biological “fingerprints” left by a tumor, giving us a detailed roadmap of that specific cancer. These signals can be genes, proteins, or other substances that reveal your cancer's most intimate secrets, moving us far beyond one-size-fits-all medicine.
Unlocking Your Cancer’s Unique Blueprint

With biomarker testing, we are no longer guessing. We are analyzing the lock.
This powerful analysis provides your oncology team, like the experts at Hirschfeld Oncology, with a precise blueprint of the tumor. It shows us the specific genetic mutations or protein expressions that are fueling its growth. Armed with this knowledge, we can move from a broad attack to a highly strategic one.
The Power of a Personalized Approach
Understanding your cancer's unique fingerprint is the cornerstone of modern oncology. It's what allows your doctor to match you with advanced therapies that are not only more effective but often come with fewer side effects than traditional approaches.
This personalized strategy really helps in three main ways:
- Pinpointing Targeted Therapies: Biomarkers can identify the exact "target" on cancer cells, letting us use drugs designed to attack those cells directly while leaving healthy cells alone.
- Guiding Immunotherapy: Certain markers can tell us how likely your own immune system is to respond to treatments that help it recognize and fight the cancer.
- Skipping Ineffective Treatments: Just as crucial, this testing helps us rule out treatments that simply won't work for your cancer, saving precious time and sparing you from unnecessary toxicity.
By uncovering a tumor’s specific vulnerabilities, biomarker testing turns cancer care from a process of elimination into a precise, targeted science. It’s the single most important first step toward a truly personalized treatment plan.
To make these concepts a bit easier to digest, here's a quick reference guide.
Quick Guide to Understanding Biomarkers
This table breaks down the core ideas behind biomarker testing into simple, straightforward terms.
Understanding your biomarkers is about gaining control by gaining knowledge.
From Diagnosis to a Clearer Path Forward
The information from these tests isn't just a lab report; it's a roadmap for your entire treatment journey. It brings clarity during a time of great uncertainty, creating a solid foundation for the decisions you and your doctor will make together.
At Hirschfeld Oncology, we use this detailed blueprint to design a strategy that is built for you and you alone.
This means we can identify the most promising treatments, whether that’s a specific targeted drug, an immunotherapy agent, or even a highly selective low-dose chemotherapy regimen. Understanding what are cancer biomarkers is the first step in seeing how this knowledge leads to smarter, more compassionate care designed to give you the best possible outcome.
The Journey from Discovery to Modern Personalized Medicine
The idea of using biological signals to understand cancer might feel brand new, but its story actually begins over 175 years ago. This long history isn't just a science lesson; it's the very foundation of trust for the biomarker-guided care we practice today. The advanced, personalized treatments we now rely on are the direct result of a steady, methodical journey of discovery, connecting those early breakthroughs to today’s life-changing therapies.
Believe it or not, this journey started back in 1846. A protein called Bence Jones protein was found in the urine of a patient with myeloma. That accidental discovery became the first documented tumor biomarker in history. It was a monumental shift, changing our view of cancer from a mysterious force to something with detectable biological signatures. Fast forward to the 1970s, and the field took another big step with markers like prostate-specific antigen (PSA), which quickly became a vital tool for prostate cancer screening.
Key Milestones on the Path to Precision
The leap from those initial discoveries to the precision medicine we have now was fueled by several critical breakthroughs. Think of each one as adding another layer of detail, allowing scientists and doctors to peel back the complexities of cancer one by one.
- The Rise of Genetic Markers: The 1990s were a game-changer with the discovery of the BRCA1 and BRCA2 genes. Finding these markers meant we could finally identify people with a high inherited risk for breast and ovarian cancers, opening the door to proactive screening and prevention for the first time.
- The Dawn of Targeted Therapy: In the late 1990s and early 2000s, we saw the first drugs designed to attack specific cancer-driving proteins, like HER2 in breast cancer. This was a true turning point. It proved we could create treatments that hit the cancer cell's "off switch" directly, leaving healthy cells largely alone.
- Unlocking the Genome: The completion of the Human Genome Project gave us an incredible road map of our DNA. This new understanding paved the way for powerful technologies that could quickly analyze a tumor's entire genetic makeup.
These milestones weren't just academic exercises; they were the practical, necessary steps that led directly to the powerful therapies we use here at Hirschfeld Oncology.
The history of cancer biomarkers shows a clear, logical progression. We went from observing broad signals in the body to pinpointing the exact genetic code driving a tumor's growth. That’s what makes truly personalized medicine a reality today.
From Historical Markers to Modern Tools
Today, that long and rich history of research has led to incredible testing methods that can analyze dozens, or even hundreds, of potential biomarkers all at once. Having the ability to see a tumor’s complete molecular profile is precisely what allows us to create such highly individualized treatment plans.
This evolution is most apparent in the power of modern testing. We've moved far beyond single-gene tests to comprehensive analyses like next-generation sequencing (NGS). You can learn more about how next-generation sequencing in clinical decision-making for cancer care is changing everything by giving us a complete blueprint of a tumor’s unique vulnerabilities.
This detailed view allows us to choose from a much wider range of targeted therapies and immunotherapies, ensuring your care plan is built on a solid foundation of scientific evidence that has been decades in the making.
Decoding the Different Types of Cancer Biomarkers
Think of how a mechanic uses different tools for different jobs—a wrench for bolts, a pressure gauge for tires. Oncologists use different types of cancer biomarkers in a similar way to understand and treat your cancer. Each marker gives us a unique piece of information. When we put all those pieces together, we get a complete picture that helps guide your care plan from start to finish.
It's important to know that not all biomarkers do the same thing. They generally fall into a few main categories, with each one answering a different, critical question about your cancer. Let's break them down.
Diagnostic Biomarkers: Answering “Do I Have Cancer?”
First up are diagnostic biomarkers. These are the detectives of the group. Their main job is to help confirm or rule out the presence of cancer.
They act like specific clues that point to a particular type of cancer, and sometimes they can raise a flag even before you feel any symptoms. A classic example is the Prostate-Specific Antigen (PSA) test for prostate cancer. While high PSA levels don't automatically mean cancer, they're a strong signal that we need to look closer.
These markers are absolutely essential for catching cancer early and making the diagnostic process faster and more accurate.
Prognostic Biomarkers: Answering “What Is My Cancer’s Likely Path?”
Once we've confirmed a cancer diagnosis, the next big question is about its personality. Is it aggressive or slow-growing? This is where prognostic biomarkers come into play. They act like a weather forecast for your cancer, helping predict its likely course and aggressiveness—independent of any treatment.
For instance, in certain early-stage breast cancers, looking at specific gene profiles can help us understand the chances of the cancer coming back. This information is vital. It helps us decide just how aggressive your treatment needs to be.
A prognostic marker gives us a baseline understanding of the tumor’s personality. It helps us gauge the level of risk, which directly informs how aggressive our treatment strategy needs to be from the very beginning.
A lower-risk prognosis might mean we can use a gentler therapy, sparing you unnecessary side effects. On the other hand, a high-risk prognosis tells us we need to be more assertive with treatment right away to stay ahead of the disease.
Predictive Biomarkers: Answering “Which Treatment Will Work Best?”
Finally, we have predictive biomarkers, which are arguably the most crucial for shaping your actual treatment plan. These are the strategists. They tell us precisely which treatments are most likely to be effective against your specific cancer.
These markers identify a tumor's "Achilles' heel"—a specific genetic mutation or protein that a targeted drug can attack. Think of it like a lock and key. The predictive biomarker is the unique shape of the lock on the cancer cell. If we know that shape, we can find the exact key (a targeted therapy or immunotherapy) that will work.
A perfect example is the HER2 protein in breast cancer. If a tumor has high levels of HER2, we know that drugs specifically designed to target HER2 will be highly effective. If it's HER2-negative, those same drugs won't work, so we won't waste precious time trying them. This gets you on the right treatment, faster.
To make these distinctions even clearer, here’s a simple breakdown of how each biomarker type informs your care:
Types of Cancer Biomarkers and Their Functions
Understanding what each biomarker tells us is the foundation of modern, personalized oncology. It's how we move beyond a one-size-fits-all approach.
At Hirschfeld Oncology, we use a combination of these biomarker types to build a complete, multi-dimensional view of your cancer. This integrated strategy—combining diagnosis, prognosis, and prediction—is what allows us to design a truly personalized and effective plan for every single person we see.
Common Biomarkers That Guide Advanced Cancer Treatment
Now that we’ve covered the different types of cancer biomarkers, let's move from theory to practice. It’s one thing to understand the concepts, but seeing how specific markers directly shape treatment decisions is where it all clicks. These aren’t just abstract lab values; they are powerful keys that unlock more precise, more effective therapies for many kinds of cancer.
When a tumor test reveals a particular biomarker, it’s like your oncologist just found a tailor-made instruction manual for attacking that specific cancer. This knowledge lets them bypass guesswork and select a treatment designed to exploit that exact vulnerability.
HER2 in Breast Cancer
One of the most well-known and impactful predictive biomarkers is the Human Epidermal growth factor Receptor 2 (HER2). Think of the HER2 protein as a gas pedal for cell growth. In some cancers, especially breast cancer, the cells have way too many copies of the HER2 gene. This overproduction leads to a glut of HER2 protein, essentially sticking the gas pedal to the floor and telling the cancer cells to grow and divide uncontrollably.
A "HER2-positive" test result is an incredibly clear signal. It tells us that drugs designed specifically to block that overactive HER2 protein will likely be very effective. Therapies like trastuzumab (Herceptin) and pertuzumab (Perjeta) are fantastic examples of treatments that can dramatically improve outcomes for patients with HER2-positive breast cancer, and sometimes stomach or esophageal cancers, too. To see this in action, understanding how breast cancer targeted therapy connects a biomarker test directly to a life-changing treatment is a great place to start.
EGFR in Lung and Colorectal Cancer
Similarly, the Epidermal Growth Factor Receptor (EGFR) is another critical protein that helps manage normal cell growth. But in some non-small cell lung cancers (NSCLC) and colorectal cancers, mutations in the EGFR gene cause this protein to get stuck in the "on" position, constantly telling cells to multiply.
Finding an EGFR mutation is often great news because it opens the door to a whole class of drugs called EGFR inhibitors. Medications like osimertinib (Tagrisso) for lung cancer or cetuximab (Erbitux) for colorectal cancer are built to do one thing: shut down that faulty EGFR signal. For patients with these specific mutations, this approach is frequently far more effective and easier to tolerate than traditional chemotherapy.
Finding a predictive biomarker like EGFR or HER2 doesn't just add a treatment option; it often points to the best first treatment option, allowing us to use a smarter, more targeted weapon from day one.
KRAS Mutations
The KRAS gene is a key player in the complex signaling network that tells cells when to divide. When it mutates, it can get jammed in the "on" position, driving relentless cancer growth. For many years, KRAS was considered "undruggable," a frustrating dead end that left patients with fewer targeted options.
Thankfully, that’s no longer the case. Recent breakthroughs have given us new drugs like sotorasib and adagrasib that can specifically target a common KRAS mutation known as G12C, particularly in lung and colorectal cancers. This is a massive step forward, opening up a new line of attack for a huge group of patients who previously had to rely on other treatments.
BRCA Mutations in Ovarian, Breast, and Prostate Cancer
You may have heard of BRCA1 and BRCA2. These are genes that function as our body's own tumor suppressors by helping repair damaged DNA. When a person inherits a mutation in one of these genes, their cells lose some of that repair capability. This difficulty in fixing DNA errors can lead to cancer—most famously breast and ovarian cancer, but also prostate and pancreatic cancer.
For patients whose cancer is linked to a BRCA mutation, a class of drugs called PARP inhibitors can be remarkably effective. These drugs create a "one-two punch." The cancer cells already have a faulty DNA repair system because of the BRCA mutation. PARP inhibitors work by knocking out a different DNA repair pathway. For a cancer cell, losing both repair mechanisms is a fatal blow, causing it to die while leaving healthy cells mostly unharmed.
PD-L1 and Immunotherapy
Finally, some biomarkers don't point to a drug that attacks the cancer directly, but instead predict whether a patient's own immune system can be unleashed to do the job. PD-L1 is a protein that some cancer cells display on their surface. It essentially acts as a "don't see me" flag, telling incoming immune cells to stand down.
If a tumor shows high levels of PD-L1, it's a strong clue that a treatment called immunotherapy might work well. Drugs known as checkpoint inhibitors—like pembrolizumab (Keytruda) or nivolumab (Opdivo)—block that PD-L1 signal. By doing this, they effectively take the brakes off the immune system, allowing it to recognize and attack the cancer. This biomarker is now routinely used to guide immunotherapy decisions across many cancers, including lung cancer, bladder cancer, and melanoma.
How Doctors Find Your Cancer's Biomarkers
Knowing that your cancer has unique biomarkers is one thing, but how do we actually find them? This is a question I hear all the time, and it’s a good one. The thought of more tests can be stressful, but the process is often much simpler than you might expect. It all boils down to one thing: getting a sample of the tumor to analyze its unique molecular signature.
This type of analysis falls under the umbrella of molecular testing, a powerful way to look deep inside your cancer cells and decode the very instructions that tell them to grow and spread. Think of it as moving from a general diagnosis to a specific, actionable blueprint for your treatment. We have a few different ways to get the material we need for that blueprint.
The Standard Approach: A Tissue Biopsy
For a long time, the go-to method has been a tissue biopsy. This is where a surgeon or radiologist takes a small sample of the tumor itself. This might happen during a surgery to remove the tumor, or through a targeted procedure using a needle to extract a tiny piece of tissue.
That tissue sample, which is full of cancer cells, is then sent off to a specialized lab. There, pathologists can run a whole battery of tests to map out its biomarkers. Because it's a direct sample of the tumor, a tissue biopsy is considered the "gold standard" for getting a reliable, high-quality picture of the cancer's makeup. The downside? It’s an invasive procedure and isn't always possible, especially if a tumor is in a tricky spot or if a patient isn't well enough for the procedure. Plus, it only gives us a snapshot in time—what the tumor looked like on that specific day.
The Modern Breakthrough: A Liquid Biopsy
This is where a much more patient-friendly and dynamic alternative comes in: the liquid biopsy. It sounds complex, but it’s really just a simple blood test that can do something truly incredible. As tumors grow, they shed tiny fragments of their DNA into the bloodstream, which we call circulating tumor DNA (ctDNA). A liquid biopsy is designed to find and analyze these fragments.
So, instead of needing a physical piece of the tumor, we can find its genetic fingerprint floating in your blood. The idea isn't brand new—scientists noticed cancer cells in blood decades ago—but the technology really came into its own in the 2000s. Today, it's a standard part of care for many cancers. In non-small cell lung cancer, for instance, a liquid biopsy can spot key EGFR mutations in 10-15% of patients, pointing us directly to targeted therapies that can more than double the time a patient lives without the cancer progressing.
This simple infographic helps visualize how the whole process works—from test to treatment.
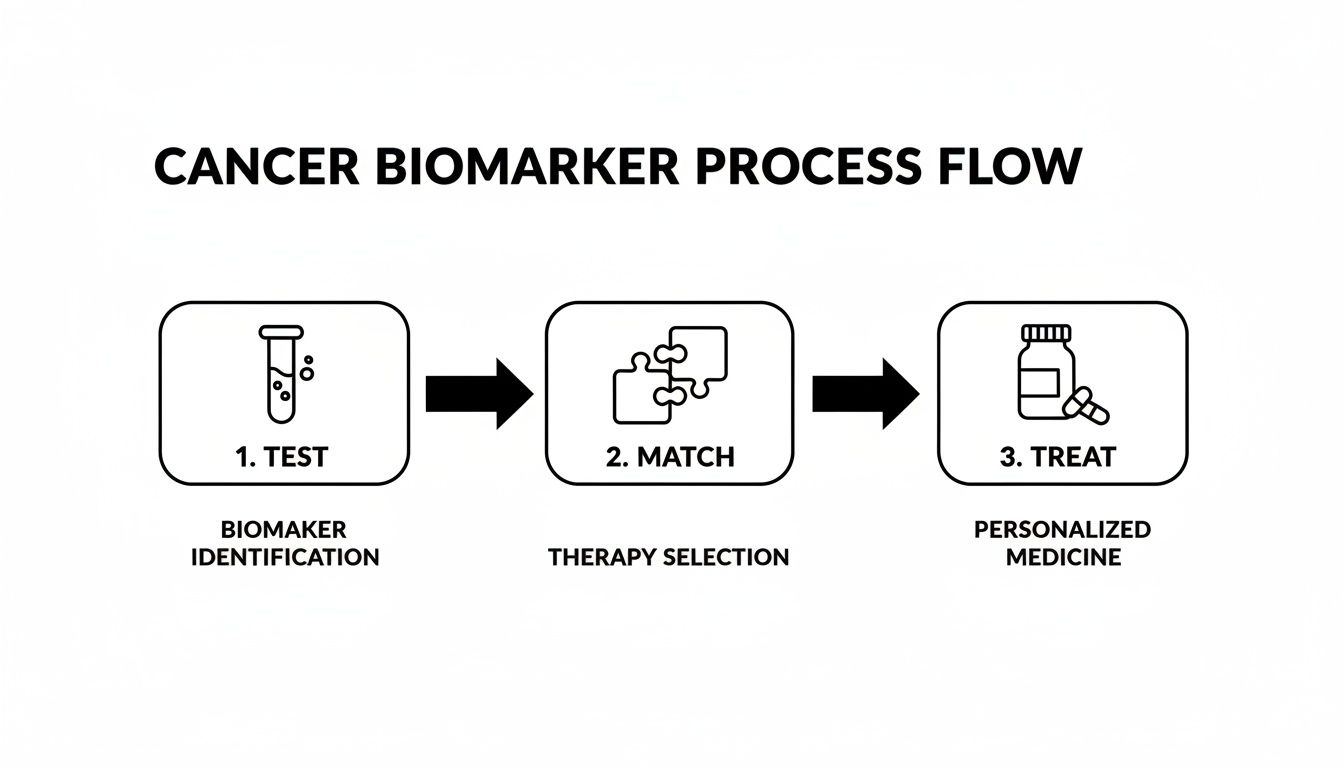
As you can see, the test provides the critical data needed to match you with a precise therapy, creating a clear and direct path to the right care.
Perhaps the biggest advantage of a liquid biopsy is the ability to monitor the cancer over time. Cancers are smart; they can change their genetic makeup to resist treatment. With a simple blood draw, your care team at Hirschfeld Oncology can stay on top of these changes, ready to adjust your treatment strategy the moment the cancer’s blueprint evolves. This lets us stay one step ahead.
To dig a little deeper, you can learn more about what molecular testing for cancer entails in our detailed guide. This ongoing vigilance is key to making sure your treatment plan stays as effective as possible throughout your journey.
Your Personalized Path Forward with Biomarker-Guided Care

Knowing what cancer biomarkers are is one thing, but seeing how they can forge a clearer, more hopeful path forward is what truly matters. All the science and testing we’ve talked about boils down to one simple goal: to craft a treatment plan that is as unique as you and your cancer. This is the very heart of personalized medicine, and it’s the core of how we practice at Hirschfeld Oncology.
Think of your biomarker profile as more than just a lab report. It’s a detailed blueprint that allows your care team to move beyond one-size-fits-all protocols. It gives us the intel we need to build a strategy aimed squarely at your cancer’s specific weaknesses.
A Collaborative and Compassionate Strategy
Your biomarker test results kick off a crucial conversation between you and your doctor. It's not about us telling you what to do; it's a collaborative process where we lay out all the possibilities and explain what each piece of information means for your treatment.
This discussion often uncovers pathways you may not have known existed. It empowers us to consider:
- Targeted Therapies engineered to attack the exact mutations fueling the cancer’s growth.
- Immunotherapies selected because your biomarkers suggest your own immune system can be activated to fight back.
- Innovative Low-Dose Chemotherapy regimens, chosen because they can be highly effective while minimizing side effects.
This way of thinking has completely reshaped modern oncology. Globally, FDA approvals for biomarker-guided drugs jumped from just 5% in 2000 to a staggering 45% by 2020. We see this impact every day. For instance, in certain esophageal and ovarian cancers, a biomarker like MSI-H can qualify patients for treatments that achieve response rates of up to 50%. You can learn more about the evolution of biomarker use in cancer treatment to see just how far we've come.
At Hirschfeld Oncology, we believe that advanced science and compassionate care go hand-in-hand. Your biomarker results give us the scientific tools; our experience and dedication ensure we use them to create a plan that respects your personal goals and quality of life.
Your Partner in Advanced Cancer Care
This level of detailed, personalized care isn’t some far-off concept—it’s available right here in New York City. For patients in Brooklyn, Williamsburg, Bushwick, and the surrounding areas, our team is here to translate complex science into a clear, actionable plan that can restore hope.
Facing a cancer diagnosis is a profound challenge, but you don't have to walk this path alone. By understanding your cancer’s unique biomarkers, we can fight smarter, together. We are committed to being your partner on this journey, armed with the expertise and compassion needed to chart the best course forward.
If you’re ready to explore how a biomarker-guided approach can shape your treatment, we invite you to schedule a consultation. Let’s start the conversation about your personalized path to better outcomes.
Frequently Asked Questions About Cancer Biomarkers
When you're navigating a cancer diagnosis, it can feel like you're being flooded with new information and complex terms. Understanding cancer biomarkers might seem overwhelming at first, but we've answered some of the most common questions to help bring some clarity and confidence to your conversations with your care team.
What if My Cancer Doesn’t Have a Known Biomarker?
This is a perfectly normal and common question. If your initial tests don't turn up a specific "actionable" biomarker, it's easy to feel discouraged, but it absolutely does not mean you're out of options.
First, knowing what isn't there is incredibly valuable in itself. This result helps your oncologist rule out certain treatments that simply wouldn't work, which saves you precious time and protects you from the side effects of an ineffective therapy.
Your treatment plan will then be built around other crucial factors—the specific type of cancer, its stage, and your overall health. This might mean a carefully selected chemotherapy regimen or other standard-of-care treatments that have a long track record of success. The science is always moving forward, and your care team will be on top of any new discoveries that could be relevant to you down the road.
Think of it this way: not finding a specific biomarker isn't a dead end. It’s a signpost that points your doctor toward the most promising path for you, based on all the available information.
How Often Will I Need Biomarker Testing?
Another great question. The first round of comprehensive biomarker testing is usually done on the tumor sample from your initial biopsy or surgery. This gives us a detailed baseline—a "blueprint" of the cancer right at the start.
But cancer can change over time, especially as it responds (or stops responding) to treatment. If a therapy that was once working becomes less effective, your doctor might recommend re-testing the tumor to see if its molecular profile has shifted.
This is where liquid biopsies are a game-changer. Because they're just a simple blood draw, they offer a non-invasive way to monitor the cancer's genetics over time. Here at Hirschfeld Oncology, we use this approach to stay one step ahead, adapting your treatment strategy to match any changes in the cancer's makeup.
Is Cancer Biomarker Testing Covered by Insurance?
For the vast majority of patients with advanced cancer, the answer is yes. Biomarker testing is now considered the standard of care for many cancer types because it’s the only way to match patients with life-changing, FDA-approved targeted therapies and immunotherapies.
Because of this, most major insurance plans and Medicare provide coverage for comprehensive genomic testing for cancers where it's indicated. While the fine print can vary from one plan to another, our team at Hirschfeld Oncology is very experienced in handling the insurance side of things.
We’ll work directly with your insurance provider to get the necessary approvals, taking that burden off your shoulders so you can focus on what matters most—your health.
At Hirschfeld Oncology, your unique biomarker profile is the cornerstone of the personalized, compassionate, and effective treatment plan we build for you. To learn more about our approach, please explore our oncology insights and resources.





.png)


.png)
.png)




