Breast cancer targeted therapy is a type of treatment that uses drugs designed to find and attack specific features of cancer cells. It's different from traditional chemotherapy, which tends to affect all fast-growing cells in the body. These therapies work by zeroing in on the unique molecules that cancer needs to grow and spread, giving us a more precise and often gentler way to fight the disease.
A Smarter Approach to Cancer Treatment

It helps to think about cancer treatment like finding the right key for a very specific lock. For a long time, chemotherapy was our best tool, but it acted like a master key. It opened—and affected—nearly every door in the body, including the ones on healthy cells. This is why chemo can cause such tough side effects, like hair loss and nausea.
Targeted therapy, on the other hand, is like a custom-made key. It's designed to fit only the unique locks found on or inside cancer cells. This modern strategy cleverly turns a cancer’s own biology into its biggest vulnerability.
Finding the Right Target
So, what exactly are these "locks"? In oncology, we call them biomarkers. These are specific proteins, genes, or other substances that act as fuel for a cancer’s growth. By running tests to identify a tumor’s unique biomarkers, we can choose a drug that directly targets that exact mechanism.
This approach gives us two major advantages:
- Better Efficacy: The treatment is aimed squarely at the engine driving the cancer.
- Less Collateral Damage: Because most healthy cells don't have these specific targets, they're largely left alone, which often means more manageable side effects for the patient.
This level of precision is why targeted therapy has become a pillar of modern cancer care. In fact, these treatments now command a 44.80% share of the global breast cancer market, a number that highlights just how central they've become. This isn't just about market statistics; it's a direct reflection of how these therapies are improving patient outcomes. You can learn more about the growth and impact of these advanced treatments.
The core idea is simple but powerful: instead of using a sledgehammer to crack a nut, targeted therapy uses a specialized tool designed for that one specific job. It allows for a much more focused and intelligent attack on the disease.
Comparing Treatment Philosophies
To really grasp the difference, it’s helpful to see how these two approaches stack up side-by-side.
Targeted Therapy vs. Chemotherapy: A Quick Comparison
This table offers a clear, at-a-glance look at how targeted therapy and traditional chemotherapy differ in their fundamental approach to fighting cancer.
Ultimately, targeted therapy for breast cancer represents a significant shift away from a one-size-fits-all model. It allows us to create a more personalized, effective, and tolerable treatment plan based on the unique blueprint of your specific cancer.
How Biomarker Testing Guides Your Treatment
Before we can even think about which targeted therapy is right for you, we need a detailed map of the cancer itself. That’s exactly what biomarker testing provides. It’s the foundational first step, moving us away from a generalized diagnosis and toward a treatment plan that is precisely matched to your tumor’s specific biological drivers.
Think of it like being a detective cracking a case. We take a small tissue sample, usually from your biopsy, and send it off to a specialized lab. There, pathologists analyze the cancer cells to uncover their unique "fingerprint"—the specific proteins and genetic mutations that are telling them to grow and spread. This isn't just a small detail; it's the entire roadmap for your treatment.
Identifying Your Cancer’s Unique Fingerprint
In breast cancer, a few key biomarkers act like on/off switches or fuel sources for the tumor. Finding out which ones are active is absolutely essential for modern, effective care. The main culprits we look for are:
- Hormone Receptors (ER/PR): We check to see if the cancer cells are covered in receptors for estrogen (ER-positive) or progesterone (PR-positive). If they are, it means the cancer is using your body's own hormones as fuel. This is actually good news, as it gives us a clear target: hormone-blocking therapies can effectively starve the cancer.
- HER2 Status: This test looks for an overabundance of a protein called HER2 (human epidermal growth factor receptor 2). When a tumor is HER2-positive, it means its cells are littered with these receptors, which act like accelerators, telling the cancer to grow and divide aggressively. Luckily, we have fantastic drugs designed specifically to shut down this signal.
- Gene Mutations: We can also screen for specific gene mutations, like those in the BRCA1 and BRCA2 genes, which can be either inherited or acquired. Finding one of these mutations reveals a specific weakness in the cancer cells that we can exploit with a powerful class of drugs known as PARP inhibitors.
This in-depth analysis gives us the exact coordinates we need to choose a therapy that will hit the cancer where it hurts. To learn more about the specifics of this process, you can explore our guide on what molecular testing for cancer involves.
Why This Step Is So Crucial
Honestly, without this information, treatment selection would be a shot in the dark. Biomarker testing is the difference between a blunt, one-size-fits-all approach and a sophisticated strategy designed just for you. It’s not an optional extra; it is the standard of care.
Biomarker testing transforms cancer treatment from a broad attack into a precision strike. It allows us to select a therapy that targets the cancer’s specific weaknesses while minimizing harm to healthy cells, leading to better outcomes and often more manageable side effects.
The results from these tests directly steer every decision that comes next. For instance, a tumor that is HER2-positive will almost always be treated with a HER2-targeted therapy—it’s a clear match. If we find a triple-negative breast cancer (ER-negative, PR-negative, and HER2-negative) that also has a BRCA mutation, a PARP inhibitor immediately becomes a leading option.
Ultimately, this testing empowers you and your care team to make the most informed, confident decisions possible. It ensures your treatment plan is built on a solid foundation of scientific evidence, giving you the best chance for success right from the start.
A Closer Look at Different Targeted Therapies
Once biomarker testing reveals the specific "locks" on your cancer cells, we can move beyond one-size-fits-all treatments. This is where the strategy gets personal. We're no longer using a sledgehammer; we're using a set of highly specialized keys designed for the unique molecular signature of your cancer.
Each type of targeted therapy works differently, honed to interfere with the exact pathways a tumor relies on to grow and spread. Let's walk through the main classes of drugs we use for breast cancer.
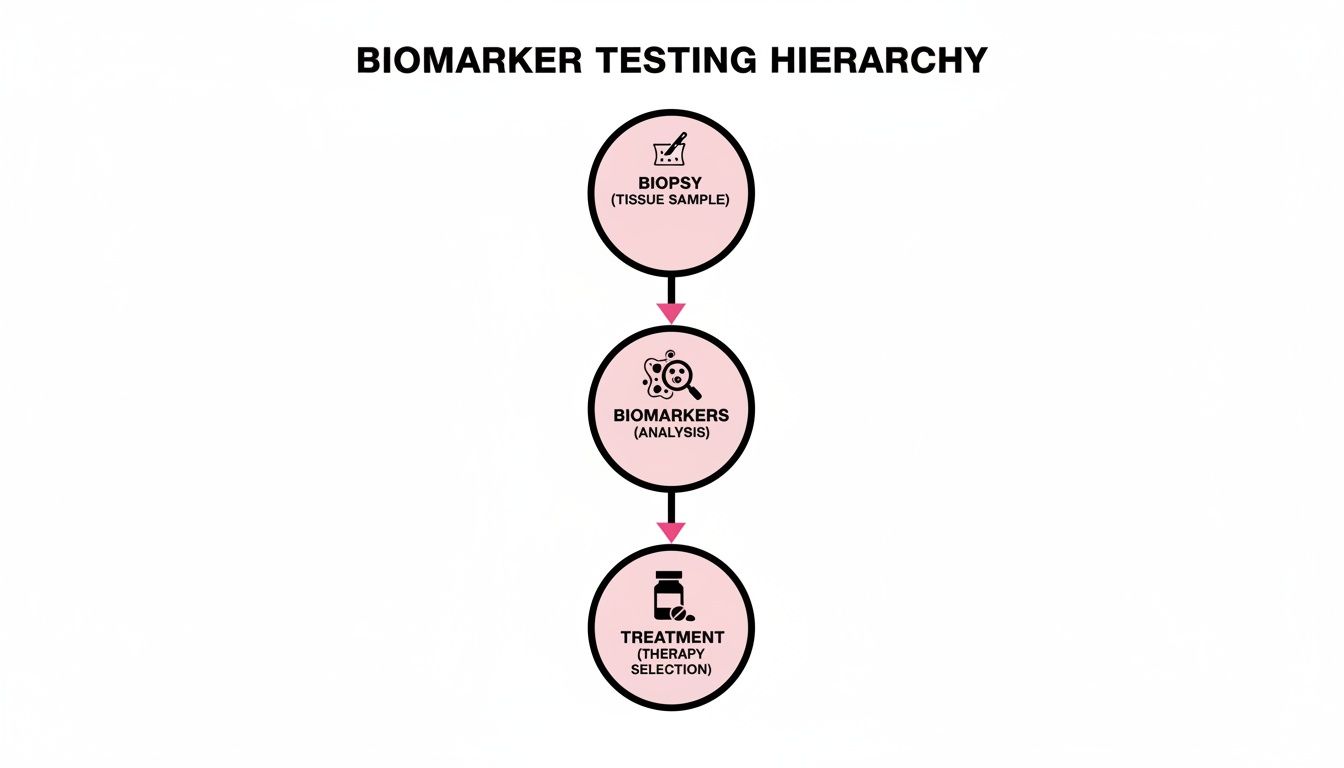
The path from a biopsy to a personalized treatment plan is a logical, step-by-step process. This visual shows how a tissue sample provides the crucial biomarker information that guides us to the most effective targeted therapy for you.
This really gets to the heart of modern oncology. Your unique biology is the roadmap for every treatment decision we make together.
HER2-Targeted Agents: Silencing the Growth Signals
About 15-20% of breast cancers are what we call HER2-positive. This means the cancer cells have far too many copies of a protein called HER2 on their surface. Think of these proteins as tiny accelerators stuck in the "on" position, constantly screaming at the cell to divide, divide, divide.
HER2-targeted drugs are designed to shut down this relentless signaling. They do this in a few clever ways:
- Monoclonal Antibodies: Drugs like trastuzumab (Herceptin) and pertuzumab (Perjeta) are like smart keys that fit perfectly into the external part of the HER2 protein. They physically block the protein from receiving growth signals and can even act like a beacon, flagging the cancer cell for destruction by your own immune system.
- Kinase Inhibitors: Other drugs, like lapatinib (Tykerb), are small enough to get inside the cancer cell. They work from within to disable the HER2 protein's internal machinery, stopping it from sending growth commands down the line.
By severing this critical communication pathway, these therapies can bring HER2-positive breast cancer to a screeching halt. They truly represent one of the biggest success stories in targeted therapy.
CDK4/6 Inhibitors: Pushing the "Pause" Button on Cell Division
The most common type of breast cancer is hormone receptor-positive (HR+), HER2-negative. For these cancers, a different engine is often driving growth. Inside the cell, two proteins called CDK4 and CDK6 act as crucial gatekeepers, giving the final green light for a cell to enter the division process.
You can imagine the cell cycle as an assembly line. CDK4/6 proteins are the final quality control supervisors who approve a cell to move on and replicate. In HR-positive cancer, these supervisors can become overactive, waving cells through far too quickly and leading to uncontrolled growth.
CDK4/6 inhibitors—such as palbociclib (Ibrance), ribociclib (Kisqali), and abemaciclib (Verzenio)—work by blocking these proteins. They essentially hit the 'pause' button on the cell's assembly line, preventing cancer cells from making copies of themselves.
These oral medications are almost always used alongside hormone therapy, creating a powerful one-two punch against the cancer. They have dramatically improved outcomes for patients with advanced HR-positive breast cancer. To understand more about how this approach differs from older methods, see our detailed comparison of targeted therapy vs chemotherapy.
PARP Inhibitors: Exploiting the Cancer's Achilles' Heel
Some breast cancers are tied to an inherited mutation in the BRCA1 or BRCA2 genes. Normally, these genes are the body's expert DNA repair crew. When they're mutated, the cancer cells are stuck with a faulty repair system, which makes them surprisingly vulnerable.
This is where PARP inhibitors shine. Healthy cells have several backup systems for repairing DNA damage. But cancer cells with a BRCA mutation become desperately reliant on a different repair protein called PARP. It's their last line of defense.
PARP inhibitors, including olaparib (Lynparza) and talazoparib (Talzenna), are designed to knock out this last-resort repair mechanism. By taking away PARP, the drugs cause so much DNA damage to build up inside the cancer cell that it can no longer function and self-destructs. It's a brilliant strategy that exploits a specific weakness found only in the cancer cells, leaving most healthy cells untouched.
Antibody-Drug Conjugates: The "Smart Bomb" Approach
One of the most exciting frontiers in breast cancer treatment is the rise of antibody-drug conjugates (ADCs). I often describe these to my patients as "smart bombs" because they merge the pinpoint accuracy of a targeted antibody with the raw power of chemotherapy.
Here’s the elegant, three-part design:
- The Antibody: This is the guidance system, engineered to seek out and latch onto a specific marker on the surface of cancer cells (like HER2 or Trop-2).
- The Linker: A stable chemical bond connects the antibody to a highly potent chemotherapy drug.
- The Payload: This is the chemotherapy agent itself—often too powerful to be given to a patient on its own through an IV.
The ADC circulates harmlessly through the body until its antibody finds and binds to its target on a cancer cell. Only then is the entire complex pulled inside the cell, where the linker releases its chemotherapy payload directly where it will do the most damage. This maximizes the effect on the tumor while dramatically minimizing the collateral damage to healthy tissues.
Drugs like sacituzumab govitecan (Trodelvy) and trastuzumab deruxtecan (Enhertu) are fantastic examples of ADCs that have completely changed the treatment landscape for many patients facing advanced or resistant disease.
When Doctors Recommend Targeted Therapy
One of the most common questions I hear is, "When is the right time for targeted therapy?" It’s a great question, because these powerful drugs aren't a one-size-fits-all solution. They're used very deliberately at specific points in the cancer journey, always based on what we've learned about your tumor's unique biology.
The decision always comes back to the biomarkers we find during testing. This lets us match the right drug to the right cancer, giving it the best possible chance to work, whether we're trying to prevent a recurrence or manage advanced disease.
Preventing Recurrence After Initial Treatment
For many people with early-stage breast cancer, the first steps are usually surgery, chemotherapy, or radiation. The goal there is to get rid of all the cancer we can see. But the job isn't done. The next, equally crucial, step is to track down and eliminate any microscopic cancer cells that might be hiding in the body, which helps lower the risk of the cancer ever coming back.
This follow-up phase is called adjuvant therapy, and it's where targeted drugs can be incredibly effective for certain cancers.
For example, if someone has an early-stage HER2-positive tumor, they will almost always receive a HER2-targeted drug like trastuzumab (Herceptin) for up to a year after their main treatment. We have years of data showing this approach dramatically cuts the chances of recurrence. It's become a true standard of care.
Managing Advanced or Metastatic Disease
When breast cancer spreads to other parts of the body—what we call metastatic or Stage 4 cancer—our treatment goals naturally shift. We move away from aiming for a cure and toward long-term management. The focus becomes controlling the cancer's growth, easing symptoms, and making sure you can live well for as long as possible.
In this situation, targeted therapies are often the main players. They are usually much easier to tolerate than traditional chemotherapy, which means they can be used for long stretches to keep the disease stable.
For metastatic cancer, targeted therapy helps us treat the disease more like a chronic condition. The idea is to turn a life-threatening illness into a manageable one, using precision drugs to keep it in check, often for years at a time.
A perfect example is someone with metastatic HR-positive, HER2-negative breast cancer. A very common and effective strategy is combining a CDK4/6 inhibitor with hormone therapy. This duo can control the disease for a long time with side effects that are typically manageable.
A Lifeline When Other Treatments Stop Working
Cancers can be stubborn. Sometimes, a tumor evolves and learns how to get around a specific treatment, which we call treatment resistance. Other times, a cancer is just aggressive and hard to treat from day one.
Targeted therapies can offer a critical lifeline in these tough situations. Take triple-negative breast cancer (TNBC), for instance. It accounts for 15-20% of all cases and has a reputation for being aggressive, partly because it lacks the usual hormone or HER2 receptors to target. But for TNBC patients who also have a BRCA mutation, PARP inhibitors have given us a powerful and much-needed tool. Finding these kinds of specific vulnerabilities is a huge focus in oncology research today, as detailed in reports about the breast cancer treatment market on PrecedenceResearch.com.
Likewise, when a cancer keeps growing after someone has already been through several different treatments, newer drugs like antibody-drug conjugates (ADCs) can step in and provide an entirely new way to attack the cells.
To help put it all together, this table shows how different scenarios often point to specific types of targeted therapies.
Targeted Therapy Applications in Breast Cancer
As you can see, the specific situation—from the cancer's stage to its unique genetic markers—is what guides our hand in choosing the right approach for you.
Weighing the Benefits and Side Effects of Targeted Therapy

When we talk about a successful treatment plan for breast cancer, we're really talking about a careful balance between two critical things: how well the treatment works and your quality of life while you're on it. Deciding on a breast cancer targeted therapy isn't just about fighting the disease—it’s about finding a way forward that lets you live your life as fully as possible.
To do that, we need to have an honest conversation about what the experience is really like. That means looking closely at both the major upsides and the potential downsides. Knowing what to expect is the first step toward feeling in control of your own health journey.
The Real Advantage of a Targeted Approach
The single biggest benefit of targeted therapy is its precision. Think of it less like a sledgehammer and more like a key designed for a specific lock. By zeroing in on the exact molecules that are telling cancer cells to grow, these drugs can be incredibly effective for the right patient.
And because they tend to leave healthy, normal cells alone, the side effects are usually less harsh and very different from what people experience with traditional chemotherapy.
This focused attack translates into real-world benefits:
- Higher Success Rates: We're not guessing. The treatment is matched directly to the cancer's known weaknesses.
- Less Collateral Damage: This often means you can avoid some of the toughest chemo side effects, like total hair loss or severe nausea.
- Better Quality of Life: With more manageable side effects, many people find they can keep up with work, family, and their daily routines.
The core idea is simple but powerful: we're shifting from a broad, carpet-bombing attack to a strategic, special-ops mission. This precision can lead to longer-lasting results and a much better overall experience, turning cancer into something that can be managed long-term, not just an acute crisis.
Navigating the Potential Side Effects
Now, while "targeted" often means "gentler," it’s crucial to know that it doesn't mean "side-effect-free." These drugs work by interfering with very specific pathways inside cells, and that can cause its own unique set of issues. This is where open, constant communication with your oncology team becomes absolutely essential.
What you might experience really depends on the specific drug you're taking.
- HER2-Targeted Agents: Can cause fatigue. In some cases, they might affect heart function, which is why we monitor you so closely.
- CDK4/6 Inhibitors: These can lower your white blood cell count (a condition called neutropenia), which raises your risk of infection. Fatigue and diarrhea are also common.
- PARP Inhibitors: Nausea and fatigue are frequent culprits here, and these drugs can also affect your blood cell counts.
A huge part of modern cancer care is being proactive. We don't wait for problems to start; we work to prevent them. Many side effects can be managed quite well with other medications, simple lifestyle changes, and good planning. At Hirschfeld Oncology, this is a top priority—we make sure you have the tools to stay ahead of any issues. For a more detailed look, you can learn more about managing targeted therapy side effects on our blog.
Still, side effects can be a real challenge. Some studies show discontinuation rates as high as 35% due to side effects, which highlights just how important it is to have good management strategies and to keep developing better drugs. This is especially true for patients who have already been through several other treatments. Finding a therapy that works and is tolerable is the ultimate goal.
In the end, understanding both the incredible potential and the possible challenges of targeted therapy is what makes you an active, empowered partner in your own care.
Taking the Next Step in Your Care
Feeling informed is the first step toward feeling empowered. Now that you have a clearer picture of what targeted therapy is and how it works for breast cancer, you’re in a much better position to have meaningful conversations about your own treatment. This is your care, after all, and your voice is critical in shaping a plan that feels right for you.
The key is turning this new knowledge into action. That starts with a productive, open conversation with your oncology team. A little preparation before your next appointment can make all the difference, helping you walk out of the clinic with clarity instead of more questions.
Questions to Ask Your Oncologist
To help you get the conversation started, here are a few key questions you can bring to your next appointment. Think of them as a launchpad for a deeper discussion about your unique situation.
- About Your Diagnosis: "Can you walk me through my biomarker report? What does being [HER2-positive, HR-positive, BRCA-mutated, etc.] specifically mean for the treatment options available to me?"
- Treatment Recommendations: "Based on my cancer's profile, what targeted therapy do you think is the best fit, and why? Are there any other options we should be thinking about?"
- Side Effect Management: "What are the most common side effects people experience with this drug? More importantly, what signs should I watch for, and when is it time to call your office?"
- Logistics and Lifestyle: "How is this therapy actually given—is it a pill or an infusion? How might it affect my day-to-day life with work and family?"
This kind of dialogue is what collaborative care is all about. Your questions tell your doctor what’s on your mind and what’s important to you, which is essential for building a plan that’s not just medically sound but also works for your life.
Your appointments are not just for receiving information; they are for building a partnership. By asking detailed questions, you help ensure your treatment plan is not only medically sound but also a good fit for your life.
This personalized approach is exactly why these treatments have become so central to modern oncology. The global market for breast cancer drugs, valued at USD 36.62 billion in 2024, is expected to nearly double to USD 69.72 billion by 2033. That incredible growth is largely fueled by the power of precision therapies. You can explore more data on the breast cancer drug market to get a sense of the scale.
Your Consultation in NYC
Here at Hirschfeld Oncology, we are firm believers that an empowered patient is a stronger patient. Dr. Hirschfeld and our entire team are here to make sure you understand every aspect of your care. We don’t just tolerate questions; we welcome them. Every consultation is a collaborative session.
If you are in the New York City area and want to discuss your options for targeted therapy, we invite you to request a consultation. We are here to provide clarity, explore all available treatment avenues, and help you find the best path forward.
Common Questions About Targeted Therapy
It’s completely normal to have practical questions when you're starting a new treatment plan. Thinking about the timeline, what-ifs, and other possibilities is a natural part of the process. Let’s walk through some of the most common questions we hear from patients about targeted therapy for breast cancer.
How Long Will I Be on This Treatment?
This is one of the first things most people ask, and the honest answer is: it really depends on your specific situation. There’s no one-size-fits-all timeline.
For early-stage breast cancer, we often use targeted therapy as a preventative measure after your main treatments are done. Think of it as an extra layer of security. In this case, you might be on a drug for a set period, like one year, to help make sure the cancer doesn't come back.
When we're treating metastatic (Stage 4) breast cancer, the goal is different. The plan is usually to stay on the targeted therapy for as long as it's keeping the cancer under control and any side effects are manageable. For many people, this can be for years.
What Happens If a Targeted Therapy Stops Working?
Cancer cells can be clever, sometimes finding ways to grow despite a drug that once worked well. If this happens, please know it’s not a failure. It’s a common challenge in long-term cancer care, and it’s something your oncology team is prepared for. It just means it's time for a new game plan.
When we see signs of resistance, we have several good options:
- Switching to a different drug: We can often pivot to another targeted therapy that works in a slightly different way, hitting the cancer from a new angle.
- Trying a combination: Sometimes, adding another drug—like a different targeted agent or chemotherapy—is enough to get things back on track.
- Exploring clinical trials: This can be a great time to look into newer treatments that aren't widely available yet but show a lot of promise.
We expect cancer to change over time. That’s why we monitor you so closely with scans and bloodwork. It lets us stay ahead of the curve and adjust your treatment strategy the moment it’s needed.
Are Clinical Trials an Option for Me?
Yes, absolutely. Every single treatment we use today, including all the targeted therapies, exists because of patients who participated in clinical trials. They are the driving force behind all progress in medicine.
Trials can be a fantastic option, particularly if your cancer is advanced or has become resistant to the standard therapies. They give you a chance to access the next generation of care before anyone else. Don't hesitate to ask your oncologist if there are any trials that could be right for your specific cancer, its biomarkers, and your treatment history. It’s a simple question that can open up a world of new possibilities.
At Hirschfeld Oncology, we know that understanding your care is just as important as the treatment itself. If you're weighing your options and have questions, we're here to help you find the answers. You can find more insights on the Hirschfeld Oncology blog.





.png)


.png)
.png)




