When you first hear the words "bone metastasis," it’s natural to feel overwhelmed. But the first step in taking control is understanding exactly what's happening. Bone metastases are not a new type of cancer; they are cancer cells that have traveled from their original location—like the breast, prostate, or lung—and settled in the bones.
This is a sign of advanced cancer, but it's absolutely a treatable condition. We have many ways to manage symptoms, slow the disease, and protect your quality of life.
Understanding Bone Metastases and Your Treatment Goals
Imagine a dandelion in a field. The wind catches its seeds and carries them to a different part of the meadow, where they can take root and grow. Bone metastasis works in a similar way. The original tumor is the dandelion, and stray cancer cells (the "seeds") travel through your bloodstream or lymphatic system. When they land in the supportive environment of your bones—the "new soil"—they can start to grow.
This is a really important point: bone metastasis is not the same as bone cancer. If you have prostate cancer that has spread to your hip, the cells in your hip are still prostate cancer cells. This is a crucial distinction because it dictates our entire treatment approach.
Primary Goals of Your Treatment Plan
Our focus isn't just on fighting cancer cells. It's about building a comprehensive plan that helps you live as fully and comfortably as possible. The main objectives are always centered on you:
- Controlling Symptoms: Relieving pain is almost always priority number one.
- Preventing Complications: We want to strengthen your bones to prevent fractures and other problems, which we call skeletal-related events (SREs).
- Slowing Cancer Growth: We use a range of therapies to manage the cancer's progression within the bones and throughout the body.
- Maintaining Your Quality of Life: Our ultimate goal is to help you keep up with your daily activities, stay mobile, and protect your overall well-being.
A metastatic cancer diagnosis can feel daunting, but modern therapies have transformed it into a condition that many people can live with for years. The goal is to control the disease, minimize its impact, and empower you to continue living a full life.
Which Cancers Commonly Spread to Bone
Just about any cancer can spread to the bone, but some do so far more often than others. In fact, managing metastatic bone disease has become a major focus in oncology over the last decade.
Research shows that for some cancers, like lung cancer, bone spread can be present right at the initial diagnosis (in about 18.05% of cases). However, for breast and prostate cancers, the bones are by far the most common site once the disease has metastasized.
Looking at patients with distant metastases, a staggering 64.20% of breast cancer cases and 59.89% of prostate cancer cases involved the bones. This makes them the two most common culprits. For men navigating this, understanding how we monitor the bones is key; you can read more in our detailed article about the role of a bone scan for prostate cancer.
Building Your Multilayered Defense Plan
When we talk about treating bone metastases, it’s never just about one single action. A better way to think about it is creating a strategic, multilayered defense plan designed to protect you from several angles at once. We combine therapies that work throughout your body with others that zoom in on the bones themselves, creating a strong, coordinated response.
This comprehensive approach is about fighting the cancer where it lives while also reinforcing your body’s own structures. By layering treatments, your oncology team can manage symptoms, slow the disease’s progression, and prevent serious complications—all with the goal of preserving your quality of life.
Systemic Treatments: The Body-Wide Approach
The first layer of defense is almost always systemic therapy. These are treatments that travel through your bloodstream, hunting down and fighting cancer cells wherever they might be hiding in the body, not just in the bones. This is absolutely critical because if cancer has spread to your bones, it’s likely present in other areas, too.
Systemic therapy isn't a single drug but a category of powerful tools:
- Chemotherapy: Uses potent drugs to destroy fast-growing cancer cells.
- Hormone Therapy: Works by blocking or lowering the specific hormones that certain cancers, like breast and prostate cancer, need to grow.
- Targeted Therapy: These are smarter drugs that identify and attack specific features on cancer cells, largely sparing healthy cells.
- Immunotherapy: A fascinating approach that revs up your own immune system, training it to better recognize and destroy cancer.
The right combination depends entirely on the type of cancer you originally had. The therapy for breast cancer that has spread to the bone will look very different from the one used for lung cancer in the same situation.
Bone-Targeted Agents: Reinforcing Your Skeleton
The next layer focuses specifically on protecting your bones. Think of these treatments as sending in reinforcements to strengthen a weakened wall. Cancer cells can throw off the natural, delicate balance of bone breakdown and rebuilding, leaving bones fragile and prone to fractures. Bone-targeted agents work to restore that crucial balance.
The two main types are:
- Bisphosphonates: These drugs slow down the cells responsible for breaking down bone tissue (called osteoclasts). This gives your bone-building cells a chance to catch up, making your bones denser and stronger over time.
- Denosumab: This is a different type of drug, a monoclonal antibody, that also blocks osteoclasts but through a different pathway. It is highly effective at reducing the risk of fractures and other skeletal complications.
These therapies aren't just about making bones stronger; they are a fundamental part of managing bone metastases. Their purpose is to prevent painful complications, keep you mobile, and protect your skeleton from further damage.
The cancers that most commonly spread to the bone are what make this multilayered defense so essential.
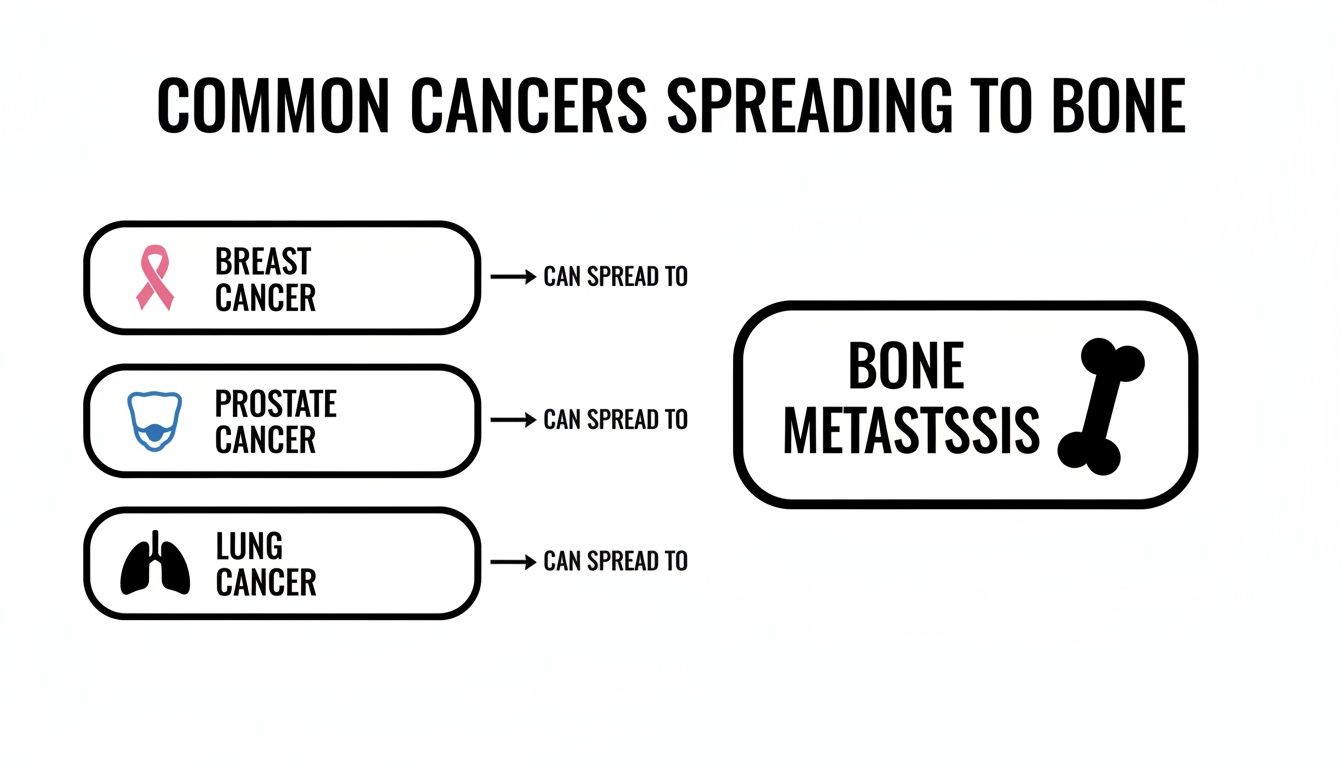
As this image shows, cancers originating in the breast, prostate, and lung are the most frequent culprits. Each one requires its own tailored mix of systemic and bone-directed therapies to be managed effectively.
Local Treatments: Targeting Specific Areas
Finally, the third layer involves local treatments, which are aimed at a specific tumor or problem area. These are like a high-precision toolkit we pull out to address an immediate issue, such as a particularly painful tumor or a bone that’s at high risk of breaking.
The most common local treatment by far is radiation therapy. It uses high-energy beams to shrink tumors, which can provide significant pain relief and help prevent a fracture in a weakened spot. In some situations, surgery might be needed to stabilize a bone with a metal rod or plate.
The following table provides a quick summary of these treatment categories and what you can generally expect from each.
Overview of Bone Metastases Treatment Approaches
This table helps illustrate how each piece of the treatment puzzle has a distinct role in your overall care plan.
Real-world evidence strongly supports this combined approach as the standard of care. For example, a large study of breast cancer patients with bone involvement found that 89.7% received systemic chemotherapy. At the same time, 86.5% of all patients were treated with bone-modifying agents like bisphosphonates or denosumab. This shows just how intertwined these therapies are in creating a robust defense. You can learn more by exploring the full research about multimodal care for bone metastasis.
A Closer Look at Advanced and Targeted Treatments
When we move beyond the first lines of defense, like systemic drugs and bone-strengthening agents, we enter the world of highly focused, powerful treatments for bone metastases. We typically turn to these advanced options in specific scenarios—perhaps a tumor is causing unbearable pain, it’s tucked away in a tricky spot, or it has simply stopped responding to other therapies. Think of these not as broad-spectrum attacks, but as precision strikes against the most troublesome cancer sites.
This is an incredibly dynamic area of oncology. In fact, the global market for bone metastasis treatment is on track to more than double over the next decade, jumping from USD 19.38 billion to an estimated USD 36.94 billion by 2032. That growth is fueled by the success of techniques like stereotactic radiotherapy and the development of new, smarter drugs. You can discover insights on the bone metastasis treatment market to see just how rapidly this field is evolving.
Stereotactic Body Radiotherapy (SBRT)
Imagine conventional radiation is like a broad flashlight beam, illuminating a general area. Stereotactic Body Radiotherapy (SBRT), in contrast, is like a swarm of laser pointers, all converging on a single, tiny point from many different directions. Using sophisticated imaging and GPS-like guidance systems, SBRT delivers an incredibly potent dose of radiation right to the tumor with breathtaking accuracy.
This pinpoint precision lets us hit the cancer cells with maximum force while carefully sparing the healthy tissue nearby, such as the spinal cord or other vital organs.
SBRT has been a genuine game-changer for controlling tumors in critical, hard-to-reach areas. Because the dose is so powerful and focused, we can often complete the treatment in just one to five sessions, a huge improvement over the weeks required for conventional radiation.
The results speak for themselves. Some studies show SBRT achieves local tumor control in 80–95% of spinal metastases. It’s a powerful tool for lasting pain relief and stopping a tumor's growth in its tracks.
Radiopharmaceuticals: The "Smart Bomb" Approach
Another sophisticated option in our toolkit is radiopharmaceuticals. The best way to think of these is as "smart bombs" engineered to seek and destroy cancer cells hiding in the bones.
These drugs are fascinating. They pair a radioactive particle with a molecule that is naturally attracted to areas of high bone activity—which is exactly what you find where metastases are growing.
Here's how it plays out:
- Injection: The radiopharmaceutical is given through a simple injection into the bloodstream, where it starts circulating through the body.
- Targeting: The "seeking" part of the drug acts like a homing device, locking onto the bone surfaces where cancer cells are disrupting the normal structure.
- Delivery: Once attached, the radioactive particle releases a small, localized burst of radiation directly into the cancer cells, effectively killing them from the inside.
Because these drugs travel throughout the entire body, they can treat multiple bone metastases all at once. This makes them an excellent choice when the cancer has spread widely across the skeleton. Radium-223 (Xofigo®) for prostate cancer and Samarium-153 for other cancers are two common examples.

Interventional and Surgical Procedures
Sometimes, radiation alone isn’t the right tool for the job. This is especially true if a bone has become so weak that it’s on the verge of breaking, or if a tumor is pressing on a nerve and causing severe pain. In these situations, we might call on our colleagues for an interventional procedure or even surgery.
- Cryoablation: This is a minimally invasive technique where an interventional radiologist guides a needle-like probe into the tumor. The probe then freezes the tumor solid, and the extreme cold creates ice crystals that destroy the cancer cells from within. It can bring remarkably fast pain relief for a single, painful spot.
- Minimally Invasive Surgery: If a bone in the spine or a major weight-bearing bone like the thigh bone (femur) is structurally unstable, an orthopedic surgeon can step in. They might stabilize the bone with metal rods, screws, or plates. In the spine, they can even inject a special type of bone cement—a procedure known as vertebroplasty—to strengthen a fractured vertebra.
It’s important to remember that these procedures aren't intended to cure the cancer. Instead, they are vital tools for managing pain, restoring mobility, and preventing a catastrophic fracture that could dramatically impact your quality of life.
Understanding all your options, from systemic drugs to these highly specialized local treatments, is key to making empowered decisions. For a deeper dive into one of the most critical systemic approaches, you can learn more about targeted therapy in our detailed guide.
Prioritizing Your Comfort and Quality of Life
When you're dealing with bone metastases, the treatment isn't just about fighting cancer cells—it's about protecting your quality of life. The two goals are completely intertwined. This means we take a direct, hands-on approach to managing pain and other symptoms so you can continue to live as fully and comfortably as possible.
You should never feel like you have to just "tough out" your symptoms. Managing how you feel day-to-day is a central part of your treatment plan, and your oncology team has a whole toolbox of strategies to help. The most important thing you can do is have honest, open conversations with us about what you're experiencing.

Comprehensive Symptom and Pain Control
Pain is often the most common and disruptive part of living with bone metastases, but it is also one of the most manageable. A good pain control plan isn't a one-size-fits-all prescription; it's a multifaceted strategy that combines medications with other supportive therapies to tackle discomfort from every angle.
Your personalized comfort plan might include:
- Pain Medication: This can range from over-the-counter options for milder pain to carefully managed prescription medications for more significant discomfort. We'll find what works for you.
- Targeted Radiation: As we've touched on, a few focused radiation treatments on a painful spot can bring about dramatic and lasting relief.
- Physical and Occupational Therapy: These specialists are experts in movement. They can show you safer ways to do daily tasks and recommend assistive devices that reduce strain on weakened bones.
- Palliative Care: Think of palliative care as a specialized team focused entirely on improving your quality of life. They work right alongside your oncologist to address not just pain, but also things like fatigue, nausea, and the emotional toll of a cancer diagnosis.
Palliative care is an extra layer of support that can begin at any point during a serious illness—it is absolutely not just for the end of life. Its only goal is to make you feel better and live more comfortably with your condition.
Many people confuse palliative care with hospice, but they are very different. Palliative care is a vital part of active cancer treatment. To see how they compare, you can explore the differences between palliative care vs. hospice care in our detailed guide.
Managing Common Treatment Side Effects
Every effective bone metastases treatment has the potential for side effects. The key is to know what they are, be prepared, and have a plan to manage them. This helps you stay on track with your therapy while maintaining your normal routine as much as possible.
Here are a few common side effects and how we can approach them together:
Fatigue
Systemic therapies can cause a profound, persistent exhaustion that sleep doesn't seem to touch. It might sound counterintuitive, but gentle exercise like a short walk can actually boost your energy. Learning to prioritize your daily tasks and schedule brief rest periods can also make a huge difference.
Dental Health with Bone-Targeted Agents
In rare cases, bisphosphonates and denosumab can affect the jawbone in a condition called osteonecrosis of the jaw (ONJ). Because of this, a full dental check-up is essential before you start these medications. Any major dental work, like extractions, needs to be done before your treatment begins.
Nausea and Appetite Changes
Chemotherapy and other drugs can sometimes throw your appetite off or cause nausea. Simple tricks like eating smaller, more frequent meals often help. We also have excellent anti-nausea medications that can prevent this from becoming a major issue.
Your oncology team is your partner through all of this. No symptom is too small or insignificant to bring up—there's almost always something we can do to help.
How to Make Informed Decisions with Your Oncology Team
Navigating the world of bone metastases treatment is a team effort, and you are the most important person on that team. Working closely with your oncologist is key. Making a truly informed decision goes beyond just knowing the medical facts—it's about choosing a path that genuinely aligns with your life and what matters most to you.
Think of your oncologist as an expert guide. They’re tasked with piecing together a complex puzzle, using all the information available to map out the best strategy. This isn't a one-size-fits-all process; it's a deeply personal journey shaped by your unique circumstances.
Key Factors Shaping Your Treatment Plan
Because every person's situation is different, every treatment plan has to be, too. Your care team will carefully weigh several critical factors to tailor a recommendation specifically for you.
Here’s what they’ll be looking at:
- The Original Cancer Type: The treatment always targets the primary cancer. For example, a treatment for prostate cancer that has spread to the bone is fundamentally different from one designed for breast cancer.
- Location and Extent of Metastases: Are the bone spots isolated to one or two areas, or are they more widespread? Are they affecting critical, weight-bearing bones like the femur or spine, which might pose a fracture risk?
- Your Overall Health: Your general fitness level, age, and any other health conditions you manage are big factors. They help determine which treatments your body can handle effectively and safely.
- Previous Treatments: What therapies have you already tried? Your treatment history is a crucial part of the puzzle, helping guide what will likely work best next.
Ultimately, the most important piece is you. What are your goals? Are you aiming for aggressive cancer control, focusing on maximum pain relief, or prioritizing your ability to keep up with work or hobbies? Your personal priorities are the foundation of every decision we make together.
Essential Questions to Ask Your Oncologist
The best way to feel in control is to be informed. One of the most powerful things you can do is come to your appointments prepared with questions. It helps ensure you walk away with clarity and confidence.
Here are a few ideas to get the conversation started:
- What is the main goal of this treatment? Are we trying to slow the cancer down, relieve pain, or strengthen my bones?
- What are the potential benefits and risks? What are the common side effects, and what’s our plan to manage them if they appear?
- How will this treatment impact my day-to-day life? Will I be able to keep working or doing the things I love?
- How will we know if it’s working? What kind of scans or tests will we do to track my progress?
- Are there other options we could consider? What are the pros and cons of those compared to what you’re recommending?
Your questions are never an interruption—they are an essential part of your care. The best patient-doctor relationships are built on open dialogue and mutual understanding, making sure the path forward feels right for you.
Asking these questions helps shift your role from simply receiving care to actively participating in your own health journey. You become an empowered partner.
Finding Your Path Forward at Hirschfeld Oncology
When you're dealing with a diagnosis of bone metastases, finding the right care team is about more than just medical charts and lab results. It’s about finding a true partner—someone who listens, understands your goals, and is committed to your well-being. That partnership is the heart of everything we do at Hirschfeld Oncology. We don’t just treat cancer; we create personalized, low-toxicity plans that fit you.
Our entire philosophy is built on moving past the idea of a one-size-fits-all approach. We carefully weave together sophisticated treatments like immunotherapy and targeted therapies to build a plan that hits the cancer hard while being as gentle as possible on your body. It's about looking at the whole person—your specific cancer, your health, and your life—to map out a strategy that truly makes sense.
A Patient-First Philosophy in Brooklyn
For our neighbors in Brooklyn, from Williamsburg to Bushwick and beyond, we offer this level of dedicated care in a setting that feels comfortable and close to home. An advanced cancer diagnosis is hard enough; the place you receive treatment shouldn't add to the burden. Our outpatient infusion center is designed to be a calm, supportive space where you feel respected and cared for.
We have deep experience in handling complex and advanced-stage cancers, especially in situations where other treatments may have stopped working. Dr. Hirschfeld's background means we know how to think outside the box and explore every available avenue for your care.
Hope is not just a feeling; it is a strategy. We are dedicated to finding a path forward, even in the most challenging cases, by applying deep clinical knowledge and a relentless focus on restoring your quality of life.
How to Start the Conversation
Taking that next step is simple. Whether you're looking for an initial consultation or a second opinion to see if there are other options, we've made the process clear and supportive. We firmly believe that every patient deserves to understand all their choices and make decisions with an expert they trust.
When you come in, we’ll do a deep dive into your medical history and have a real, honest conversation about the road ahead. This is your time to ask the tough questions and find a team that will stand by your side. We promise to explore every option that could offer a meaningful benefit, from proven standards of care to promising new treatments on the horizon.
If you’re ready to see what a truly personalized approach to cancer care looks like, we're here for you. Scheduling a consultation at Hirschfeld Oncology is the first step toward creating a new plan—one focused on managing your condition, improving your well-being, and giving you back a sense of control.
Answering Your Questions About Bone Metastases Treatment
When you're dealing with a complex diagnosis, it's natural to have a lot of questions. We've gathered some of the most common ones we hear from patients and their families about treating bone metastases. Our goal is to give you clear, straightforward answers so you can feel more prepared for the road ahead.
Can Bone Metastases Be Cured?
This is often the first question on everyone's mind. While bone metastases mean the cancer has advanced and isn't typically considered curable, it is absolutely treatable. The goal of treatment shifts from a cure to long-term control.
It's helpful to think of it like managing a chronic condition, such as diabetes or heart disease. We focus on slowing the cancer's growth, managing symptoms like pain, preventing complications like fractures, and—most importantly—protecting your quality of life. Many people live well for years with bone metastases, able to continue with their daily lives.
Will My Treatment Be Very Painful or Toxic?
Many people worry that cancer treatment will be harsh and draining, but modern oncology has come a long way. Your treatment plan is built around you, carefully balancing the need to control the cancer with your overall well-being.
Many of today's therapies are designed to be much more tolerable:
- Targeted therapies and immunotherapies are more precise, attacking cancer cells while often sparing healthy tissues.
- Low-dose chemotherapy regimens can be very effective with far fewer side effects than the high-dose approaches of the past.
- The pain from the bone metastases themselves is a top priority. Treatments like highly focused radiation can bring significant relief to specific spots.
We are always proactive about managing side effects. Honest, open communication is crucial—we have many tools and strategies to help you stay comfortable so you can stick with your treatment.
How Is the Right Treatment Plan Chosen for Me?
Deciding on the right bone metastases treatment is a true partnership between you and your oncologist. There's no one-size-fits-all "best" plan; the right strategy is the one that fits your specific situation.
Your oncologist will look at the whole picture, considering several key factors:
- The type of cancer you started with (e.g., breast, prostate, lung)
- Where the metastases are and how many there are
- Your overall health and any other medical conditions you have
- What treatments you've had before
- Your personal goals and what's most important to you
Your doctor will walk you through all the available options, discussing the potential upsides and downsides of each one. It's a collaborative process to make sure the final plan feels right for you.
What Kind of Doctors Will Be on My Care Team?
Effectively managing bone metastases is a team sport, with your medical oncologist acting as the quarterback. They coordinate your overall game plan, especially the systemic treatments like chemotherapy or targeted therapy.
But you'll likely work with other specialists to make sure all your bases are covered. Your team might include:
- A radiation oncologist to deliver radiation therapy for pain control.
- An orthopedic surgeon if a procedure is needed to strengthen a weakened bone.
- A palliative care specialist who adds an extra layer of support focused entirely on managing symptoms and improving your quality of life.
This team approach ensures every aspect of your health is looked after, giving you coordinated, complete care.
At Hirschfeld Oncology, we are committed to creating a personalized path forward for every patient. If you are exploring treatment options for advanced cancer, we invite you to learn more about our patient-first philosophy and how we can support you.





.png)


.png)
.png)




