Getting through breast cancer surgery is a huge step. It’s a moment that brings a wave of relief, but often, it also brings a new set of questions about what comes next. This next phase is about more than just healing from the incision; it’s a journey that unfolds in stages, from immediate recovery to potential follow-up treatments and, finally, a long-term focus on your health and well-being.
Knowing what to expect can make all the difference, helping you feel more in control as you navigate the path forward.
Mapping Your Journey After Breast Cancer Surgery
Finishing surgery is a major milestone, but it’s also the starting line for the next chapter: recovery and doing everything possible to prevent a recurrence. While every person’s experience is unique, the journey after breast cancer surgery generally follows a predictable pattern of healing, adjuvant (additional) therapy, and ongoing monitoring. Think of this guide as your roadmap, breaking down each phase into clear, manageable steps.
The first few days and weeks are all about the physical side of things—managing pain, caring for your surgical sites, and slowly getting back on your feet. After that initial healing period, you'll sit down with your oncology team to talk about the next line of defense, which often involves treatments designed to find and eliminate any cancer cells that might be left behind.
This visual timeline gives you a bird's-eye view of the key phases ahead: healing, therapies, and long-term wellness.
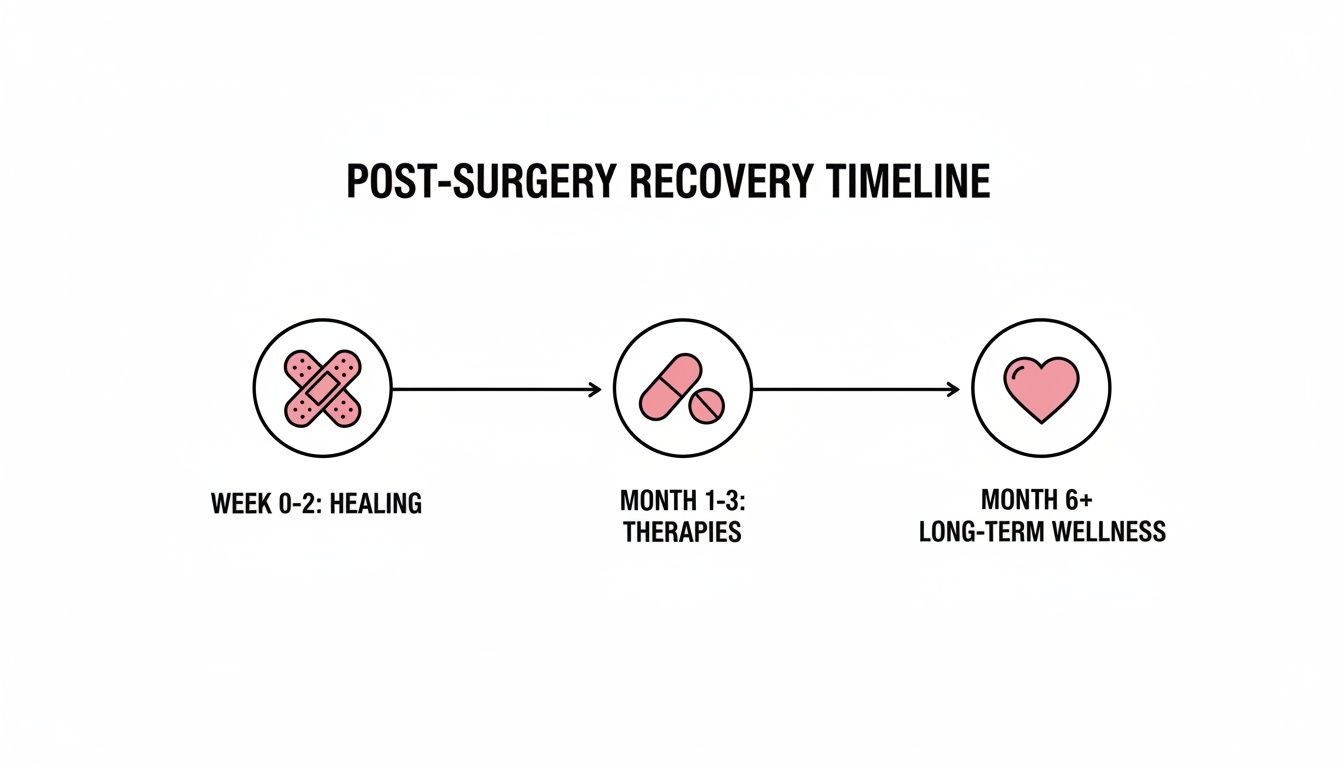
As you can see, your focus will gradually shift from the immediate physical recovery to a broader, lifelong commitment to your health.
Your Immediate Post-Surgery Recovery Timeline
To help you feel prepared, let's break down what that first month often looks like. Everyone heals at their own pace, but having a general timeline can help set realistic expectations for you and your caregivers, which goes a long way in reducing anxiety.
The table below offers a snapshot of what to anticipate as your body begins to heal.
Remember, recovery isn't a straight line. You'll have good days and bad days, and that's completely normal. The first week is usually the toughest, as your body is doing the hard work of healing and your movement is most limited. Be patient with yourself, listen to your body, and give yourself the grace and time you need to heal properly.
Navigating Your Immediate Recovery and Wound Care

The first few weeks at home after breast cancer surgery are all about one thing: healing. Your only job is to rest and give your body the space it needs to mend. This time is a mix of managing discomfort, keeping a close eye on your incisions, and learning to work with some new, temporary physical limits.
It can feel a little overwhelming, but it helps to think of this recovery period as a project with clear, manageable steps. Knowing what's coming and how to handle it can make all the difference, turning anxiety about the unknown into confidence. The first week is usually the toughest, but you'll start to see small improvements every day, and those little wins add up fast.
Mastering Your Wound and Drain Care
Learning how to care for your surgical sites and any drains is probably the most hands-on part of your early recovery. Your surgical team will walk you through everything you need to know, but the basic goals are always the same: keep the area clean, dry, and protected to head off any chance of infection.
You might go home with surgical drains, which are small tubes placed near your incision to channel away the excess fluid that naturally collects after surgery. This is a normal part of the healing process, and getting that fluid out helps reduce swelling and pressure, allowing the incision to heal better. While they can seem a bit intimidating at first, managing them quickly becomes just another part of your daily routine. For a deeper dive, check out this guide on caring for drains after mastectomy.
One of the biggest questions we hear is, "How do I know if what I'm seeing is normal?" It's completely typical to have some bruising, redness, and mild swelling. But if you notice the redness spreading, the area feeling warm to the touch, any foul-smelling drainage, or if you develop a fever, those are your cues to call your doctor right away.
It's so important to know the difference between normal healing and a potential issue. For instance, a seroma—a collection of clear fluid under the skin—can sometimes appear after drains are removed. It might feel like a little fluid-filled pocket or a water balloon. They are usually harmless, but you should always let your surgical team know if you find one.
Managing Pain and Daily Activities
Staying on top of your pain is a top priority. Your team will give you a prescription for pain medication, and the key is to take it on schedule, especially for that first week. This helps you stay ahead of the pain instead of chasing it. Most people only need the stronger medication for a short period before switching to over-the-counter options.
You'll definitely notice that your arm movements on the surgery side are limited. A great tip from survivors is to set up a "recovery nest" before your surgery day.
- Bring your world closer: Put essentials like your phone, charger, water bottle, medications, and the TV remote all within easy arm's reach.
- Plan your post-op wardrobe: Think about clothes that are easy to get into. Shirts that button or zip up the front and loose, comfy pants will be your best friends.
- Create a comfy sleep setup: Getting in and out of bed can be tricky. Many people find that sleeping in a recliner or propping themselves up with a wedge pillow in bed offers the best support and comfort.
These activity restrictions are there for a reason—to protect your incisions as they heal.
- No Heavy Lifting: For several weeks, you'll be told not to lift anything heavier than a gallon of milk, which is about 8-10 pounds.
- Driving: Plan on holding off on driving until you are no longer taking narcotic pain medication and can move comfortably enough to operate the car safely.
- Gentle Movement: While you can't hit the gym, short, gentle walks are fantastic. Walking helps prevent blood clots and can be a real mood-booster.
Above all, listen to your body. Fatigue is real, and it’s your body’s way of telling you to rest. This initial phase of breast cancer after surgery recovery is a marathon, not a sprint. Be patient with yourself, follow your team's advice, and you'll create the best possible foundation for a smooth and successful healing journey.
Understanding Your Next Line of Defense: Adjuvant Therapies
Surgery is a huge and critical step—it’s how we remove the primary tumor. But the work doesn’t stop there. Think of the surgery as putting out the main fire. Now, we need to bring in a specialized team to find and stamp out any stray embers that might have escaped.
This is exactly what adjuvant therapies do. They are the additional treatments given after surgery to track down and eliminate any microscopic cancer cells that might be lingering in the breast, lymph nodes, or even elsewhere in the body. The goal is simple but incredibly important: to dramatically lower the chances of the cancer ever coming back.
Your oncology team will look closely at the pathology report from your surgery—things like the tumor’s size, grade, and receptor status—to design a treatment plan that’s built specifically for you. It's never a one-size-fits-all approach; it’s a strategic defense tailored to your unique situation.
Chemotherapy: A Systemic Cleanup Crew
Chemotherapy, or "chemo," works like a cleanup crew that travels through your entire bloodstream. This is a crucial distinction because tiny cancer cells can sometimes break away from the original tumor and travel to distant parts of the body, far too small to ever be picked up by a scan.
Chemo drugs are designed to hunt down and destroy rapidly dividing cells, which is the classic behavior of cancer. Because this is a body-wide treatment, it can also affect your healthy, fast-growing cells—like those in your hair follicles or the lining of your stomach. This is why side effects like hair loss and nausea are common. To learn more about what to expect, check out our in-depth guide to breast cancer chemotherapy.
Chemo is typically recommended for more aggressive cancers, like triple-negative or HER2-positive types, or if the cancer has spread to the lymph nodes. It’s usually administered in cycles over several months, which gives your body a much-needed break to recover between treatments.
Radiation Therapy: A Targeted Spot Treatment
If chemo is the wide-ranging crew, then radiation therapy is the precision specialist. It uses high-energy beams, similar to powerful X-rays, to zero in on and destroy any cancer cells that might still be hiding in the breast, chest wall, or nearby lymph nodes after surgery. It’s a local treatment, meaning it only affects the specific area being targeted.
Picture it as a highly focused spotlight that makes absolutely sure no cancer cells are left behind in the surgical area. This is a very common and effective step after a lumpectomy (breast-conserving surgery) to prevent a local recurrence. The data on this is really encouraging.
A comprehensive analysis showed that breast-conserving surgery followed by radiation results in remarkably low local recurrence rates, at just 4.6% over five years. Rates were even lower for certain subtypes, with HER2+ tumors at 3.4% and ER+ or PR+ tumors at 4.0%.
Radiation is usually given in daily sessions, five days a week, for a few weeks. You won't feel a thing during the treatment itself, but side effects like skin redness and fatigue tend to build up gradually over the course of your treatment schedule.
Hormonal and Targeted Therapies: The "Smart Drugs"
Not all breast cancers are created equal. Some have very specific characteristics—like a lock that only a certain key can open. This is where "smart drugs" come in, offering a much more precise way to fight cancer than traditional chemotherapy.
Hormonal Therapy (Endocrine Therapy)
This approach is only an option for hormone receptor-positive (ER+ or PR+) breast cancers. These cancers use the body’s natural hormones, estrogen and progesterone, as fuel to grow. Hormonal therapy cleverly cuts off that fuel supply in one of two ways:
- Blocking Receptors: Drugs like tamoxifen work by sitting on the cancer cell's estrogen receptors. This essentially blocks the "docking station," so the hormone can't attach and tell the cell to grow.
- Lowering Estrogen Levels: For postmenopausal women, drugs called aromatase inhibitors (AIs) work by stopping the body from making estrogen in the first place.
This therapy is typically a daily pill that you take for 5 to 10 years, and it has proven to be an incredibly powerful tool for preventing recurrence in hormone-sensitive cancers.
Targeted Therapy
These drugs are designed to identify and attack a specific vulnerability found in certain cancer cells. The most well-known example is for HER2-positive breast cancer. In these cancers, the cells have an overabundance of a protein called HER2, which acts like a gas pedal stuck to the floor, telling the cells to grow and divide uncontrollably.
- HER2-Targeted Drugs: Medications like trastuzumab (Herceptin) and pertuzumab (Perjeta) are specifically designed to find and block the HER2 protein, effectively taking the foot off the gas and stopping the cancer's growth signal.
These therapies are often given through an IV, sometimes alongside chemotherapy, and they have completely changed the outlook for patients with HER2-positive breast cancer. Your pathology report is the key that unlocks which of these targeted treatments might be the right fit for you.
Exploring Your Reconstruction Choices and Timing
After a lumpectomy or mastectomy, one of the most personal decisions you'll face is how you want your chest to look and feel. This is a central part of your journey of breast cancer after surgery, and there is absolutely no "right" or "wrong" answer. The only thing that matters is choosing the path that feels right for your body, your lifestyle, and your own sense of self.
Whether you're thinking about rebuilding the breast or embracing a flat closure, the first step is simply understanding what's possible. This decision isn't just about what to do, but also when to do it, as the timing has to be carefully coordinated with your other cancer treatments.
Three Primary Paths Forward
Your surgical team will walk you through three main avenues after a mastectomy: using implants, using your own body tissue, or choosing to go flat. Each option comes with its own unique set of considerations, from the number of surgeries involved to the long-term feel and maintenance.
Implant-Based Reconstruction: This is the most common route. It's usually a two-step process where a surgeon first places a tissue expander to gently stretch the skin. Later, in a second surgery, the expander is swapped for a permanent saline or silicone implant.
Autologous (Tissue Flap) Reconstruction: This sophisticated technique uses your own skin, fat, and sometimes muscle—often taken from the abdomen, back, or thighs—to create a new breast. While it’s a more complex surgery, the result is a breast that often feels more natural and will age and change with the rest of your body.
Aesthetic Flat Closure: Many people know this as "going flat." This isn't just about forgoing reconstruction; it's a specific surgical choice to create a smooth, contoured chest wall. It's done with the goal of an aesthetically pleasing flat result.
Weighing the Timing of Your Reconstruction
Just as important as the type of reconstruction is when you have it done. This decision often hinges on whether you need additional treatments like radiation, which can affect skin and tissue and, in turn, impact surgical outcomes.
The conversation around reconstruction is one of the most individualized parts of the cancer journey. Your goals—whether they are aesthetic, functional, or emotional—are the most important factors in guiding your decision alongside your medical team.
Generally, reconstruction falls into one of three timelines:
- Immediate Reconstruction: The rebuilding process starts during the same operation as the mastectomy. For many, this offers a psychological lift, as you wake up with a breast mound already in place.
- Delayed Reconstruction: You can choose to have reconstruction months or even years after your mastectomy. This gives you time to heal, complete other treatments like chemo or radiation, and make the decision without feeling rushed.
- Phased Reconstruction: This is a very common middle ground, especially with implants. The first step (placing the tissue expander) happens at the time of the mastectomy, but the final step (placing the permanent implant) is delayed until later.
Researchers are always looking at how reconstruction type might relate to cancer recurrence. One review of studies found that autologous reconstruction was associated with a lower local recurrence rate (2.9%) compared to implant-based reconstruction (5.6%). This kind of data can help inform your conversations with your doctor, and you can dig deeper into recurrence patterns after mastectomy to better understand the statistics.
Comparing Your Main Reconstruction Options
Sometimes, seeing the key differences laid out side-by-side can make things clearer. The table below offers a simple breakdown of implants versus using your own tissue.
Comparing Breast Reconstruction Options Implants Vs Autologous Tissue
Ultimately, this is your choice, and you are in the driver's seat. Take all the time you need, arm yourself with questions for your surgical team, and try to connect with others who have walked these paths to hear their stories.
Focusing on Long-Term Wellness and Monitoring

Once the most intense parts of surgery and treatment are behind you, your journey with breast cancer after surgery enters a new and important phase. This is the shift into survivorship, where the focus moves from actively fighting the cancer to proactively monitoring your health for the long run.
Think of it as graduating from the crisis phase to building a sustainable, lifelong partnership with your oncology team.
This next chapter is all about your personalized survivorship care plan. This document is essentially your roadmap forward. It neatly summarizes your diagnosis and treatments while laying out a clear schedule for future check-ups, so everyone on your healthcare team is always on the same page.
Your Follow-Up and Monitoring Schedule
Your follow-up schedule is your safety net, carefully designed to keep a close watch on your health and catch any potential issues as early as possible. While the exact timing will be customized for you, most schedules follow a similar pattern.
- Physical Exams: You can expect to see your oncologist every 3-6 months for the first few years. After that, these visits usually become annual. They're a crucial time to discuss how you're feeling and for your doctor to perform a thorough physical exam.
- Mammograms: Annual mammograms are still a key part of your care. If you had a lumpectomy, both breasts will be screened. If you had a single mastectomy, the remaining breast will be monitored just as closely.
This consistent oversight is designed to give you peace of mind and ensure you remain in the best possible health for years to come.
Staying Vigilant: Recognizing Signs of Recurrence
Learning the signs of a possible recurrence is incredibly empowering. It isn’t about living in fear; it's about being an informed, active partner in your own health. Knowing what to look for allows you to be proactive without creating unnecessary anxiety.
A recurrence can happen in one of three areas:
- Local: The cancer returns in the original breast tissue or the chest wall. You might notice a new lump, skin changes like redness or thickening, or unexpected nipple discharge.
- Regional: It comes back in the nearby lymph nodes, often under the arm or near the collarbone. This could present as a new lump or swelling that doesn't go away.
- Distant (Metastatic): The cancer has traveled to another part of the body, most commonly the bones, liver, lungs, or brain. The symptoms here can be more general and might include persistent pain, unexplained weight loss, a nagging cough, or severe headaches.
It's so important to remember that everyday aches and pains are just a normal part of life. What you're looking for are symptoms that are new, persistent, and don't have an obvious explanation. When in doubt, your first call should always be to your oncology team.
Even with the best care, recurrence is a possibility we have to be aware of. For instance, young women with high-risk factors can face a 15.65% recurrence rate even after a mastectomy. One study showed a 5-year recurrence-free survival rate of 86%, which means that while most people do very well, a percentage will face a relapse.
Managing Persistent Side Effects from Treatment
The side effects of treatment don’t always disappear when your last infusion is done. Some can linger for months or even years, becoming a part of your "new normal." Finding good strategies to manage them is a huge part of maintaining your quality of life.
Some of the more common long-term side effects include:
- Lymphedema: This is a chronic swelling in the arm or hand on the side where you had surgery. It’s often managed with compression garments, specialized massage, and targeted exercises.
- Chronic Pain or Neuropathy: This can feel like lingering nerve pain, numbness, or tingling in your hands and feet. It's often a leftover from either chemotherapy or the surgery itself.
- Fatigue: This isn't just being tired—it's a deep, persistent exhaustion that rest doesn't seem to fix. Learning to pace yourself and incorporating gentle exercise can make a world of difference.
Nutrition also plays a massive role in managing these effects and boosting your overall wellness. For some practical ideas, you might find our guide on https://honcology.com/blog/what-to-eat-during-chemotherapy helpful, as many of the same principles apply to long-term survivorship. Learning to navigate these challenges is a vital part of your ongoing health plan.
When It’s Time to Look for More Specialized Oncology Care
Most of the time, the journey after breast cancer surgery follows a familiar path of healing and established therapies. But what about those times when it doesn't? What if the cancer is unusually aggressive, doesn't seem to be responding to the first line of treatment, or comes back when you thought it was gone for good?
That’s when it’s time to consider looking for more specialized oncology support. Thinking about a second opinion or more advanced care isn't a sign that something went wrong—it's about taking control of your health. It’s a way to make sure you’ve looked at every single option, especially when dealing with advanced, recurrent, or stubborn breast cancer.
Finding a Path Beyond the Standard Playbook
Specialized oncology centers are often the places that handle cases requiring a different approach. They’re set up to offer treatments and strategies that might not be available at every hospital, opening up new doors for patients who need more than the standard of care.
Some of these advanced strategies include:
- Targeted Therapies: These aren’t your typical chemo drugs. They’re designed to zero in on specific weak spots in cancer cells, which are often found through detailed genetic testing of the tumor.
- Immunotherapy: This is a fascinating approach that essentially trains your own immune system to better identify and destroy cancer cells.
- Low-Dose Chemotherapy: Sometimes called "metronomic" chemotherapy, this method involves giving smaller, more frequent doses. The goal is to choke off the cancer's blood supply and slow its growth, often with far more manageable side effects.
When you're up against a complex diagnosis, you need a team that sees you, not just a chart or a scan. The real goal is to work together on a plan that fits your life and your values, one that offers both hope and a focus on your well-being.
For patients and families in the New York City area facing these kinds of tough situations, please know that these options are out there. At Hirschfeld Oncology, we focus on creating personalized, research-driven treatment plans for complex cancers. If you're looking for a dedicated team to help you figure out what’s next, we invite you to request a consultation and learn more about our individualized care and outpatient infusion services.
Common Questions About Life After Breast Cancer Surgery
The days and weeks after breast cancer surgery are a time of transition, and it's completely normal for your mind to be buzzing with practical questions. As you start to find your footing again, getting clear, straightforward answers can make all the difference, helping you feel more in control as you navigate this new chapter.
Let's walk through some of the most common concerns that come up during this time. Remember, recovery isn't a race; it's a gradual process, and everyone's timeline looks a little different.
How Soon Can I Get Back to Normal Activities Like Driving and Exercising?
This is one of the first things people want to know, and the answer really depends on the type of surgery you had and how your own body is healing. Your surgeon will give you specific guidelines, but there are some general rules of thumb.
When it comes to driving, most surgeons recommend waiting 2-4 weeks. The key is that you must be off any narcotic pain medication and able to turn the wheel or brake suddenly without pain or hesitation. Safety comes first.
Gentle movement, like slow and steady walking, is fantastic and usually encouraged right away. It gets your blood flowing and helps prevent clots. But for anything more intense, you'll need to hit pause.
- Lifting is a no-go for a while: Plan on not lifting anything heavier than a gallon of milk (about 8-10 pounds) for at least 4-6 weeks. This gives your incisions and internal tissues the time they need to heal properly.
- Hold off on intense workouts: Things like running, high-impact aerobics, or heavy weight training should wait until you get the official all-clear from your surgeon, which is typically around 6-8 weeks post-op.
Your surgical team knows the ins and outs of your procedure, so always stick to the timeline they give you.
What Is Lymphedema and Am I at Risk?
Lymphedema is something we watch for carefully. It’s a chronic condition that causes swelling—usually in the arm, hand, or chest on the side where you had surgery. It happens when your lymphatic system, which is like your body's plumbing for fluid, gets backed up. Removing or radiating lymph nodes can sometimes create a blockage, sort of like a traffic jam, causing fluid to build up.
Your personal risk level is tied to how many lymph nodes were involved. Someone who had an axillary lymph node dissection (where many nodes are removed) has a higher risk than someone who only had a sentinel node biopsy (just a few key nodes removed). Getting radiation to the armpit area also nudges that risk up.
While there’s no foolproof way to prevent lymphedema, you can absolutely take steps to lower your risk. It’s all about protecting your arm from injury—things like cuts, burns, or bad bug bites—maintaining a healthy weight, and just generally being aware of any changes.
If you ever notice that your arm feels heavy, achy, or looks persistently swollen, let your care team know right away. They can get you connected with a certified lymphedema therapist who has specialized techniques to manage it.
How Will Adjuvant Therapy Affect My Daily Life?
Adjuvant therapies—the treatments that come after surgery to reduce the risk of cancer returning—can fit into your life in very different ways. For example, hormonal therapy is often a daily pill, and for most people, the side effects are quite manageable.
Radiation, on the other hand, usually means daily trips to the treatment center for several weeks. The biggest complaint is often fatigue, but many people find they can work out a modified schedule to keep up with work and life. Chemotherapy tends to have the most significant impact on daily routines. It's given in cycles, and the side effects, like fatigue or nausea, might mean you need to plan for time off from work to rest and recover.
I'm Feeling Completely Overwhelmed Emotionally. Is This Normal?
Yes. Absolutely, 100% normal. It is incredibly common to feel a whole tidal wave of emotions after going through breast cancer after surgery. Anxiety, sadness, fear, and even anger are all valid and expected parts of this journey. You’ve been through something enormous, both physically and emotionally, so it’s more than okay to not feel okay.
This is precisely why support is not just a "nice to have"—it's a critical part of your healing. Please don't hesitate to tell your oncology team how you're feeling. They are your lifeline and can connect you with fantastic resources, from social workers and support groups to therapists who specialize in helping people navigate the emotional side of a cancer diagnosis.
At Hirschfeld Oncology, we believe that true healing addresses you as a whole person—physically and emotionally. If you're navigating a complex diagnosis and looking for a collaborative team, we invite you to explore our patient-centered approach and advanced treatment options by visiting us at https://honcology.com/blog.





.png)


.png)
.png)




