Nausea is one of the most dreaded side effects of cancer, and for good reason. It’s a deeply unsettling feeling that can disrupt every part of your day, but understanding why it happens is the first real step toward getting it under control. It's not just a random symptom; it's your body's a biological response to major changes.
Why Do Cancer and Nausea Go Hand-in-Hand?
For so many patients, the words "cancer" and "nausea" feel inseparable. This isn't just a mental association—it’s a physical reality rooted in how both the disease and its treatments interact with your body. At the heart of it, two things are usually at play: the cancer itself, and the powerful therapies used to fight it.
Think of the constant communication happening between your gut and your brain. It's a delicate system. Both cancer and treatments like chemotherapy can interrupt these signals, sending a "panic" message to the part of your brain that controls nausea, known as the chemoreceptor trigger zone. This miscommunication is what leaves you feeling sick.
How Cancer Treatments Trigger Nausea
By far, the most common culprit behind cancer-related nausea is the treatment. Therapies like chemotherapy and radiation are incredibly effective because they target rapidly dividing cells—a hallmark of cancer. The problem is, they aren't always great at telling the difference between a cancer cell and other healthy, fast-growing cells, like those lining your stomach and intestines.
When these healthy cells get damaged, they release chemicals into your bloodstream. Your brain picks up on these signals and interprets them as a sign that something is wrong, triggering the nausea reflex to protect you. It’s an unfortunate case of friendly fire. In fact, chemotherapy-induced nausea and vomiting (CINV) is a major issue, affecting up to 80% of patients and seriously impacting their quality of life. You can learn more about the broader scope of CINV and its management on Cognitive Market Research.
When the Cancer Itself is the Cause
Sometimes, nausea isn't a side effect of treatment but a direct result of the cancer itself. This can happen in a few different ways:
- Location, Location, Location: A tumor in or near the digestive system—like in the stomach, pancreas, or intestines—can create a physical blockage or irritation that makes you feel sick.
- Pressure in the Brain: A tumor in the brain can increase pressure inside the skull, directly impacting the body's nausea control center.
- Chemical Messengers: Some tumors produce and release hormones or other substances that travel through the blood and tell the brain it's time to feel nauseous.
The important thing to remember is that nausea is a real, physiological response—not something you just have to endure. It’s a predictable and understandable part of the cancer journey for many, and knowing that makes it less frightening and much more manageable.
Once we understand the specific cause, your care team here at Hirschfeld Oncology can create a plan to anticipate and control your symptoms, helping you feel more like yourself during treatment.
Understanding the Types of Treatment-Related Nausea
Not all nausea is created equal, and figuring out what you're dealing with is the first step toward feeling better. When you receive cancer treatment, it can stir things up with your body’s natural "nausea control center" in the brain and the sensitive lining of your digestive system. This creates a chain reaction of signals that make you feel sick, but the timing can be very different from person to person.
Getting a handle on these patterns helps you and your oncology team get ahead of the nausea, often preventing it before it even starts. This shifts symptom control from just reacting to feeling sick to proactively keeping you comfortable, which makes a huge difference in your quality of life during treatment.
This concept map helps visualize how treatment sets off a cascade of events inside the body that leads to nausea.
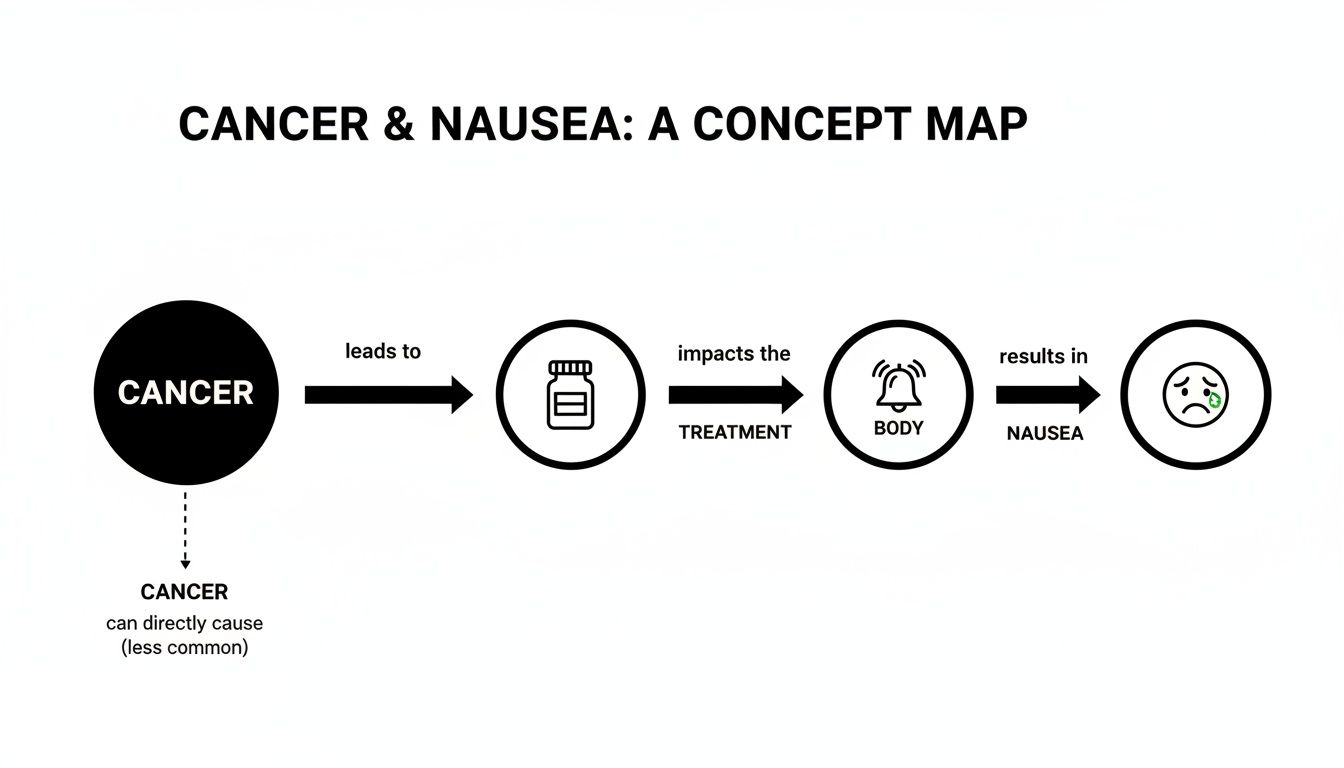
It’s a good reminder that what you’re feeling is a real, physical response to the powerful therapies working to fight cancer.
To make management easier, we can group nausea into three main patterns. Knowing which one you’re experiencing is crucial because the approach to managing each is quite different.
Three Patterns of Treatment-Induced Nausea
Let's break down what each of these feels like and why they happen.
Acute Nausea
This is the one that hits fast. Acute nausea usually shows up within a few minutes to a few hours after a treatment like chemotherapy or radiation. The good news is that it typically fades within the first 24 hours.
What’s happening here is an immediate chemical reaction. As treatment affects cells in your digestive tract, they release substances like serotonin. Your brain picks up on this sudden spike, interprets it as a sign of something toxic, and triggers the nausea reflex to protect you. Thankfully, modern anti-nausea medications are excellent at blocking these signals before they start.
Delayed Nausea
Just when you think you’re in the clear, delayed nausea can show up. This type emerges more than 24 hours after treatment is over and can linger for a few days, catching many people off guard. It’s a bit like how muscle soreness peaks a day or two after a hard workout.
Delayed nausea is caused by different biological processes than the acute kind. It's often linked to specific chemotherapy agents that create a slower, more drawn-out inflammatory response in the body. You can learn more about how these treatments work in our guide on chemo and radiation therapy. Because the root cause is different, we often use a different set of medications on a carefully planned schedule to manage it.
Anticipatory Nausea
This one can be the trickiest because it’s a mind-body connection. Anticipatory nausea is a learned response where you start to feel sick before you even receive your treatment. Simply walking into the clinic, the smell of rubbing alcohol, or even just thinking about your next appointment can be a trigger.
It’s not just a case of "being nervous"—it's a real, conditioned reflex. If you’ve had a tough time with nausea in the past, your brain creates a strong link to protect you from going through it again. This anticipatory nausea and vomiting (ANV) can impact around 29% of patients on chemotherapy, making an already difficult situation even tougher.
The Big Picture: By knowing if your nausea is acute, delayed, or anticipatory, your oncology team can create a much more precise prevention plan. This means giving you the right medicines at the right time to stop the nausea cycle before it gets a chance to start.
Here at Hirschfeld Oncology, we focus on personalized regimens designed to be less toxic, targeting cancer cells with more precision to minimize the collateral damage that causes these side effects. By understanding your specific nausea pattern, we can fine-tune your care plan even further, helping make your treatment as comfortable as it is effective.
Your Medical Toolkit for Managing Nausea

When we’re building your treatment plan, we have a powerful set of tools designed to protect your comfort and quality of life. The single most important principle in modern nausea management isn't just treating symptoms—it's prevention. Trust me, it’s far easier to stop nausea before it starts than it is to chase it down once it has already taken hold.
This proactive approach centers on a class of medications called antiemetics. Your oncologist will map out a personalized schedule for these drugs, often telling you to take them even when you feel perfectly fine. This isn't an oversight; it's a very deliberate strategy to stay one step ahead of the chemical signals in your body that trigger that awful queasy feeling.
Key Types of Antiemetic Medications
Think of antiemetics as a team of skilled defenders, with each one guarding a different pathway that nausea signals can travel. Depending on your specific treatment and how your body responds, we might use one or a combination to create the strongest defense.
Here are some of the most common and effective players on the team:
Serotonin (5-HT3) Antagonists: These are our frontline defense against that immediate, acute wave of nausea. When chemotherapy damages cells in your digestive tract, they release a flood of serotonin, which sends a "feel sick" message straight to the brain. Drugs like ondansetron essentially act as roadblocks, stopping that message from ever being delivered.
NK-1 Receptor Antagonists: These are the champions against delayed nausea. They work by blocking a completely different chemical messenger in the brain called Substance P. This substance is the main culprit behind the slower, more prolonged nausea that can creep up a day or two after your infusion.
Corticosteroids: You might know medications like dexamethasone as powerful anti-inflammatories, and that’s exactly why they work so well here. They help calm the overall inflammatory response that treatment can trigger, significantly reducing nausea, especially when paired with other antiemetics.
We also have other medications in our back pocket, like dopamine antagonists and benzodiazepines, which can be brought in to address specific situations or help ease the anxiety that often makes nausea feel so much worse.
The Power of NK-1 Receptor Antagonists
The development of the NK-1 receptor antagonist drugs was a major breakthrough for patient comfort. But a groundbreaking study in Norway, which analyzed data from 13,811 women with early-stage breast cancer, uncovered a powerful and unexpected benefit.
The anti-nausea medication aprepitant, an NK-1 receptor antagonist, was associated with a stunning improvement in survival outcomes. Over a 10-year follow-up, its use was linked to an 11% reduction in the risk of cancer recurrence and a 17% reduction in breast cancer-related death. You can explore more about these significant findings and what they mean for cancer care.
This remarkable link shows us that managing side effects isn't just about feeling better—it can be fundamental to achieving better long-term results. By keeping you stronger and better able to stick with your prescribed treatments, we give you the best possible chance for success.
At Hirschfeld Oncology, we believe that aggressive symptom management is a core part of effective cancer treatment. Your comfort is not a secondary goal; it is integral to the success of your entire care plan.
Sticking to Your Medication Schedule
Following your prescribed antiemetic schedule is one of the most important things you can do during treatment. That schedule is designed with the specific timing of your cancer therapy in mind, anticipating exactly when your body is most likely to produce those nausea-inducing chemicals so we can block them ahead of time.
It's tempting to skip a dose when you're feeling okay, but this can unfortunately allow the nausea cycle to start, making it much harder to get back on top of it. Something as simple as a medication log or setting alarms on your phone can make a world of difference.
And if you do experience nausea despite following the plan—what we call breakthrough nausea—it’s crucial to let your care team know right away.
This immediate feedback is what allows us to make precise adjustments. We might tweak the timing of your medication, add a different type of antiemetic to your regimen, or give you a "rescue" medication to take as needed. This partnership ensures your plan is always working for you, keeping you as comfortable and resilient as possible throughout your journey.
Practical Nutrition and Lifestyle Adjustments for Nausea

While your anti-nausea medications are doing the heavy lifting, the choices you make every day with food and lifestyle can provide a powerful backup. Think of it this way: the medicine is your first line of defense, but your daily habits are what reinforce those defenses, giving you a greater sense of control and well-being.
When you're dealing with cancer and nausea, it's not just about what you eat, but also when and how. The main goal is to keep your body nourished without triggering an already sensitive system. You'd be surprised how much of a difference a few simple, practical changes can make.
Choosing the Right Foods
When nausea strikes, the last thing you want to think about is a big, complicated meal. This is the time to lean on bland, simple foods that are easy for your body to process. There's a reason why the BRAT diet—bananas, rice, applesauce, and toast—is a go-to recommendation. These foods are gentle and give you the energy you need without causing trouble.
On the flip side, some foods are well-known troublemakers. Anything that’s overly greasy, fatty, spicy, or packed with sugar can be tough on your stomach. Strong smells are another huge trigger, as treatment can often make your sense of smell extra sensitive. For a deeper dive, check out our guide on what to eat during chemotherapy.
To help you out, here’s a quick-reference table. It’s a simple guide to help you pick foods that are more likely to soothe your system and identify those that might make you feel worse.
Nausea-Soothing Foods vs Potential Trigger Foods
This isn't a strict list of rules, but more of a starting point. Pay attention to what works for you and what doesn't.
Rethinking Your Mealtime Routine
Sometimes, how you eat is just as important as what you eat. Sitting down to a large meal can force your digestive system into overdrive, which is the last thing you want when you're already feeling off.
The "grazing" method can be a game-changer. Eating five or six small, snack-sized meals throughout the day keeps your stomach from getting too empty or too full, both of which can trigger nausea.
This approach helps keep your blood sugar stable and gives your body a steady stream of nutrients without the heavy workload. It helps to keep simple snacks, like a few crackers or pretzels, within arm's reach so you can eat a little something the moment hunger kicks in.
Simple Lifestyle Habits for Better Control
Beyond your diet, a few other small habits can make a big impact on managing nausea.
- Prioritize Hydration: Getting dehydrated will absolutely make nausea worse. Try sipping liquids slowly all day long instead of chugging a large glass at once. Water, broth, diluted juice, or flat ginger ale are all great choices.
- Get Some Fresh Air: Feeling stuffy can make nausea feel more intense. If you can, open a window or take a slow, gentle walk outside.
- Rest After Eating: Try to avoid lying down flat right after you eat. Resting in a reclined chair with your head elevated for at least an hour can help with digestion.
- Wear Loose-Fitting Clothing: Anything tight around your waist can put pressure on your stomach and make you feel more nauseous. Stick to comfortable, loose clothes.
By weaving these simple strategies into your routine, you create a more supportive environment for your body. It’s an empowering way to take an active role in managing your symptoms, working right alongside the medical care from your oncology team.
Using Complementary Therapies for Added Relief

Beyond your medical treatment plan, another layer of support can help you feel more comfortable and in control. These are known as complementary therapies, and they are designed to work with your prescribed anti-nausea medications, not replace them.
Think of these therapies as reinforcements for your main line of defense. They can add extra comfort without ever getting in the way of your primary cancer treatment. It’s absolutely essential to see them as supportive tools to ease the experience of cancer and nausea, not as a substitute for your oncologist's plan.
An open, honest conversation with your doctor is always the first and most important step before trying anything new.
Mind-Body Practices for Nausea Control
Several non-invasive therapies have shown real promise in helping patients get a handle on treatment-related nausea. Many of these practices work by calming the body’s stress response, which can have a direct and powerful influence on how intensely you feel nausea.
- Acupuncture and Acupressure: These time-tested techniques focus on stimulating specific points on the body. Acupuncture uses thin needles placed by a trained practitioner, while acupressure uses firm, steady pressure. A well-known point for nausea, called P6, is found on your inner wrist, and activating it can help settle the stomach.
- Aromatherapy: Your sense of smell can be a powerful ally. Aromatherapy uses essential oils from plants to create a calming environment. Gentle scents like peppermint, ginger, or lavender are often very helpful. Even a few drops on a tissue for light inhalation can distract from clinical smells and ease that queasy feeling.
- Mindfulness and Deep Breathing: Nausea and anxiety often go hand-in-hand, creating a vicious cycle. Mindfulness techniques, like guided meditation or simple deep-breathing exercises, can help break that loop. Focusing on your breath grounds you, calming your nervous system and easing the physical tension that makes nausea feel so much worse.
By bringing these practices into your routine, you’re embracing a more complete approach to your own comfort. Managing side effects isn't just about medication; it's about supporting your overall well-being throughout your treatment.
Finding the Right Complementary Approach
Not every therapy works for every person, and safety is always the top priority. Some herbal supplements, for instance, can interfere with chemotherapy, which is why total transparency with your care team is non-negotiable.
If you’re interested in learning more about how to safely combine these practices with your medical care, our guide on integrative therapies to manage side effects offers some great insights.
The ultimate goal is to build a personalized toolkit that supports you physically and emotionally. Starting a conversation with your oncologist at Hirschfeld Oncology is the best way to explore which options might be a good, safe fit for you. This collaborative approach ensures every aspect of your care is aligned, helping you move through treatment with greater comfort and confidence.
Working with Your Oncology Team for Better Nausea Control
Throughout your cancer treatment, think of your care team as your most important partner. This isn't just a group of people giving you medicine; it's a collaborative relationship, and your voice is the most critical part of it. After all, you’re the only one who truly knows what you’re feeling.
Your team brings the medical expertise, but you bring the real-world data. When you share openly and honestly about your nausea—when it happens, what it feels like, what helps, what doesn’t—you give them the exact information they need to help you. A simple notebook or a note on your phone can make a world of difference.
Your Voice Is the Most Important Tool
When you speak up about nausea early on, you allow your care team to get ahead of the problem. Instead of playing catch-up once you’re already miserable, they can make small, proactive adjustments to your anti-nausea medications, suggest a new dietary strategy, or even look into other potential causes.
This back-and-forth is what makes a treatment plan truly yours. What worked like a charm during your first chemo cycle might not be enough by the third. Your feedback is the only way your team can know that it’s time for a change.
Your quality of life during treatment isn't a "nice-to-have"—it's a critical part of the plan. Keeping nausea and other side effects under control is just as important as the cancer-fighting therapies, because it helps you stay strong enough to continue them.
Building a Proactive Partnership
So, how do you create this kind of strong, working relationship? It really comes down to a few simple but powerful actions that put you in control of your own comfort.
- Ask Anything and Everything: Never feel like a question is too small or silly. If you're wondering why you're taking a certain pill or what a new feeling means, ask. Understanding your plan helps you follow it with confidence.
- Report Nausea Right Away: Don't try to tough it out or wait until you feel completely overwhelmed. The moment you feel that "breakthrough" nausea, let your team know. It’s so much easier to get it back under control when you catch it early.
- Share Your Whole Picture: Be sure to tell your doctor about everything you're taking or trying. This includes vitamins, herbal supplements, or any complementary therapies. This ensures nothing will interfere with your treatment and that your whole care plan is working together.
You are never on this journey alone. By communicating openly with your team at Hirschfeld Oncology, you ensure your treatment is constantly being fine-tuned to keep you feeling your best. It's a partnership that empowers you, knowing you have a dedicated team fighting right alongside you, every single day.
Your Questions About Cancer and Nausea, Answered
When you're dealing with cancer treatment, it's completely normal to have a lot of questions about side effects like nausea. Getting straight answers can help you feel more in control. Here are some of the most common things patients ask us.
When Should I Call My Doctor About Nausea?
The most important rule is: don't wait until you're in a crisis. Nausea is much easier to manage when we get ahead of it.
You should call your oncology team right away if you’re experiencing any of these issues:
- You haven't been able to keep any food or liquids down for more than 24 hours.
- You're vomiting frequently, like three or more times in a single hour.
- You're seeing signs of dehydration—things like feeling dizzy or weak, having a very dry mouth, or noticing your urine is dark.
- The nausea is so bad that you can't even take your other prescribed medications.
Calling us early means we can quickly tweak your anti-nausea plan or bring you in for IV fluids before dehydration becomes a serious problem.
Can We Really Prevent Chemo Nausea Altogether?
While promising that 100% of nausea can be avoided for every single person isn't realistic, modern medicine has come a long way. The anti-nausea medications we have today are incredibly good at what they do. Our real goal is to stop nausea before it ever starts, or at the very least, keep it at a level that barely registers.
By taking your antiemetic drugs exactly as prescribed—which almost always means taking them before a treatment session or before you even feel a hint of sickness—and pairing them with the other strategies we've discussed, most of our patients find they can manage their symptoms very well and continue to live their lives during treatment.
Are Natural Remedies Like Ginger Actually Safe?
Some natural aids can definitely help, but you absolutely have to clear them with your oncologist first. Something that seems harmless could interact with your treatment. For instance, ginger is well-known for calming an upset stomach and is generally safe in foods like tea, chews, or flat ginger ale. Peppermint can also have a wonderfully soothing effect.
But please remember, not all "natural" things are benign. Certain herbal supplements can interfere with how chemotherapy works or interact with other medications you're taking. Your doctor is the best person to help you figure out which complementary therapies are truly safe and effective for you.
Does Every Cancer Treatment Cause Nausea?
Absolutely not. The risk of feeling nauseous really depends on the specific treatment you're getting. It’s not a one-size-fits-all side effect.
Here’s a quick look at what to expect:
- Chemotherapy: The likelihood of nausea is tied directly to the specific chemo drugs being used. Some have a high risk, and some have a very low risk. We build your anti-nausea plan around the specific drugs in your regimen.
- Radiation Therapy: Nausea is much more common when radiation is targeted at the stomach, pelvis, or brain. If you're getting radiation on an arm or leg, for example, it's far less likely to be an issue.
- Targeted Therapy and Immunotherapy: These newer treatments can still cause nausea, but it tends to be less frequent and less severe than with some of the more traditional chemotherapies.
Your oncologist considers all of these factors when putting together your symptom management plan. We customize your defense to match your specific treatment.
At Hirschfeld Oncology, we believe that managing side effects proactively is a core part of effective cancer care. If you have more questions or feel your plan needs a second look, we encourage you to request a consultation. See how our patient-first approach can make a difference in your treatment journey by learning more on our blog.





.png)


.png)
.png)




