When people think of chemo, nausea is often the first side effect that comes to mind. It’s one of the most feared aspects of cancer treatment, and for good reason—it’s a powerful biological response. The drugs designed to kill fast-dividing cancer cells can’t always tell the difference between a tumor and the healthy, fast-dividing cells that line your digestive tract.
This confusion inadvertently triggers your body’s built-in “poison control” center, setting off a cascade of unpleasant symptoms.
Why Chemo and Nausea Go Hand-in-Hand
Think of your body as having a sophisticated security system. If you ingest something harmful, that system sounds an alarm, sending signals from your gut straight to the "vomiting center" in your brain to get the threat out. Fast.
Chemotherapy, while doing its vital work against cancer, can trip that same alarm.
As the drugs travel through your bloodstream, they irritate the sensitive cells lining your stomach and intestines. In response, these cells release chemicals—most notably serotonin—that act like distress flares. These flares race to receptors in both your gut and your brain, creating a powerful, two-pronged alert that tells your brain something is very wrong and needs to be expelled. The result is that overwhelming feeling of nausea, often followed by vomiting.
A Hardwired Biological Response
This reaction isn’t a personal failing; it’s your body’s ancient survival programming kicking into gear. It's simply responding to a trigger it perceives as a threat.
Chemotherapy-induced nausea and vomiting (CINV) remains one of the most distressing side effects for patients, impacting an estimated 70-80% of people undergoing treatment. This is exactly why advanced oncology practices like ours focus so heavily on prevention with finely tuned, low-dose regimens that minimize this kind of collateral damage, particularly for patients with complex cases.
It's also why modern cancer care is all about getting ahead of the problem. We don’t wait for you to feel sick. We use our understanding of how these drugs work to build a defensive strategy before your first infusion even starts.
"Your body is just reacting logically to what it thinks is a toxin. Our job is to anticipate that reaction and essentially cut the wires to the alarm system before it ever has a chance to go off. We do that with targeted anti-nausea medications that block those distress signals at the source."
Once you understand this biological connection, it’s easier to see why managing nausea is a central part of your treatment plan. It’s a solvable puzzle, not a guaranteed sentence to feeling miserable.
You can learn more about how these powerful drugs function in our guide on how chemotherapy works. At Hirschfeld Oncology, we use this deep biological knowledge to build a proactive, personalized strategy that keeps you as comfortable as possible right from the start.
The Different Timings of Chemotherapy Nausea
When it comes to chemo-induced nausea, timing is everything. It’s not a one-size-fits-all symptom, and understanding when it shows up gives your oncology team critical clues to build the right defense for you. Think of it like a weather forecast—if we can predict when the storm is likely to hit, we can put the strongest protections in place.
The nausea you might feel is generally broken down into three different timelines. Pinpointing your own pattern is the first step toward getting ahead of this difficult side effect.
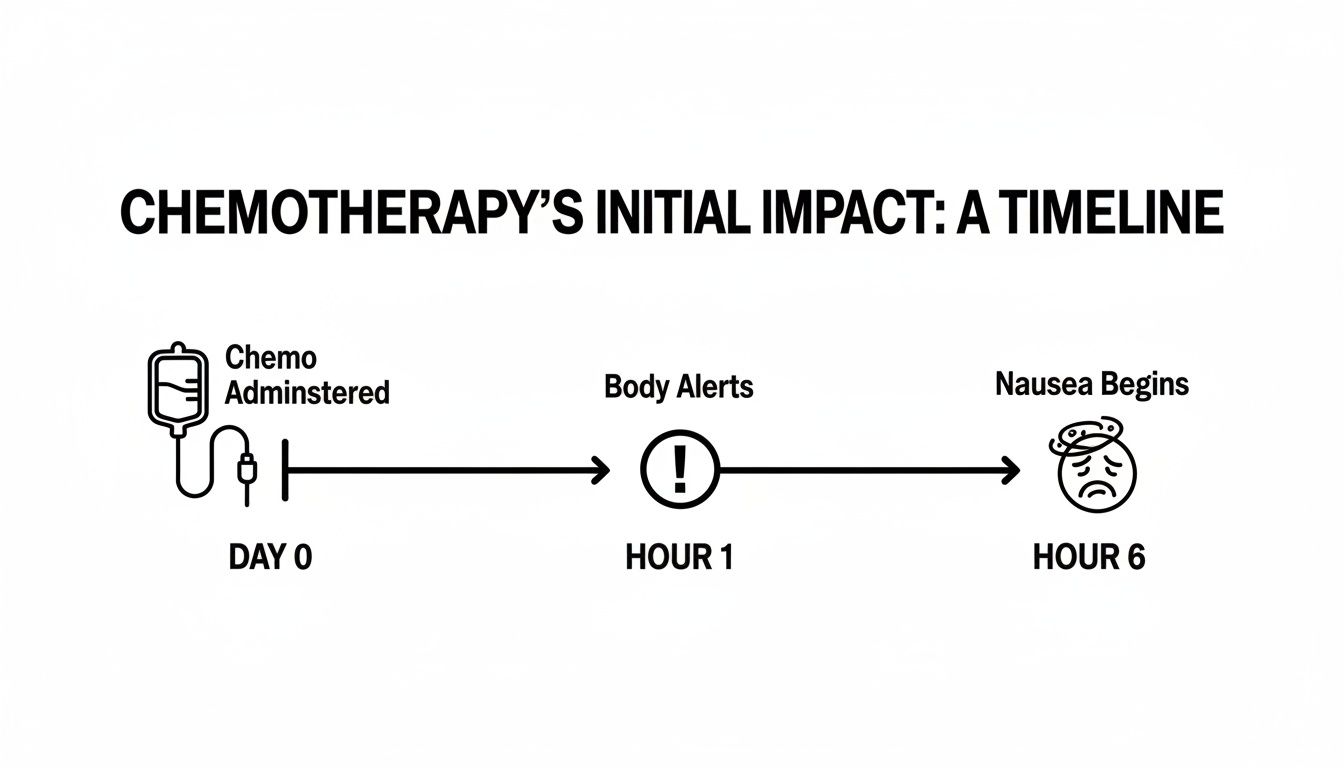
This visual shows just how quickly the body can react after treatment. That's why being proactive, not reactive, is the cornerstone of good nausea management.
Acute Nausea: The First 24 Hours
The first wave is what we call acute nausea, and it happens within the first 24 hours after your infusion. This is your body’s most immediate, direct response to the chemotherapy drugs.
What's happening here is a rapid-fire chemical reaction. The chemo drugs irritate the cells lining your digestive tract, causing them to release a flood of a chemical called serotonin. This serotonin surge acts like an alarm bell, sending urgent signals straight to the "vomiting center" in your brain, which triggers that first feeling of queasiness.
This is exactly why your care team gives you powerful anti-nausea medications before your infusion even starts. We’re essentially cutting the wires to that alarm system, blocking the serotonin signals before they ever have a chance to go off.
Delayed Nausea: The Aftershock
Just when you think you might be in the clear, a second wave can appear. This is delayed nausea, and it typically shows up more than 24 hours after treatment, sometimes lingering for a few days.
This delayed reaction is driven by a different process. It’s not about that initial serotonin rush. Instead, it’s tied to other chemical messengers involved in inflammation—think of it as the body’s cleanup crew arriving on the scene a day or two later. Unfortunately, their work can stir things up and cause symptoms of its own.
Delayed nausea can be sneaky. It often surfaces right when you’re starting to relax at home. That's why your anti-nausea plan usually includes a prescription for pills to take for several days after your infusion, specifically to target these different, slower-acting pathways.
Anticipatory Nausea: The Learned Response
Finally, there’s a fascinating—and frustrating—type of nausea that has nothing to do with the drugs themselves. Anticipatory nausea is a conditioned, psychological response that can start before you even walk through the clinic doors.
It works just like how the memory of a bad meal can make your stomach turn. If you’ve had a tough time with nausea in the past, your brain can start to associate the sights, sounds, and even smells of the treatment center with feeling sick. Soon, just the scent of an alcohol swab can be enough to trigger real, physical nausea.
This isn’t just “in your head”; it’s a powerful, learned physical reaction that affects an estimated 29% of patients. Interestingly, while newer anti-nausea drugs developed in the 1990s dramatically reduced vomiting, they had less of an impact on this kind of nausea. You can read more about this phenomenon in detailed reports on chemotherapy side effects at cancer.gov.
Tackling anticipatory nausea often requires more than just medication. We use strategies like relaxation techniques, guided imagery, or sometimes anti-anxiety medications to help your brain break those connections and calm the nervous system.
The timing of nausea provides a roadmap for managing it. This table breaks down the different types of CINV by when they happen, helping you identify and describe your symptoms for better management with your care team.
Understanding the Timeline of Chemotherapy Nausea
Knowing these distinctions helps you and your doctor anticipate and treat your symptoms more effectively, making each cycle more manageable than the last.
Your Medical Toolkit for Preventing Nausea
When it comes to managing nausea from chemotherapy, the best defense is a great offense. We don't wait for nausea to show up; we work to prevent it from ever starting. The most effective strategy is a proactive one, using a powerful combination of medications that acts like a multi-layered security system for your body. Your oncology team will carefully select these drugs to disarm nausea triggers long before your infusion even begins.
Imagine your body’s nausea response is a sophisticated alarm system. Chemotherapy can trip this alarm in two main places: in your gut (think of it as a "local sensor") and in your brain (the "central command center"). To give you complete protection, we need to place guards at both locations. This is precisely why a multi-drug approach has become the gold standard in modern cancer care.
At Hirschfeld Oncology, we tailor this toolkit for every single patient. By understanding how each medication works and why we use them together, you can feel more confident and in control of your treatment.
The Frontline Guards: 5-HT3 Antagonists
Our first line of defense targets the gut, where the initial alarm is often sounded. These medications are called 5-HT3 receptor antagonists.
Think of them as guards posted all along your digestive tract. When chemotherapy irritates the gut lining, it causes a flood of a chemical messenger called serotonin (or 5-HT3). These guards are specifically trained to block that serotonin from docking at its receptor, effectively stopping the "intruder alert" signal from ever leaving the gut.
This class of drugs is incredibly effective at preventing acute nausea—the kind that hits within the first 24 hours of treatment.
Common Examples of These Medications:
- Ondansetron (Zofran): A very common anti-nausea medication, often given through your IV right before chemo and then as a pill to take at home.
- Granisetron (Kytril): Another effective option that works in a similar way to block those serotonin signals.
- Palonosetron (Aloxi): This is a longer-acting version that can provide protection against both immediate and delayed nausea for several days with a single dose.
By getting these guards on duty before your infusion, we can shut down one of the main triggers for chemo-induced nausea right at the source.
Securing Central Command: NK-1 Receptor Antagonists
While the 5-HT3 antagonists are excellent guards for the gut, some nausea signals can bypass them and originate directly in the brain. For this, we need a different kind of security—one that works at the central command level. This is where NK-1 receptor antagonists come in.
These medications work in a very specific part of the brain called the "chemoreceptor trigger zone," which is responsible for initiating the vomiting reflex. They block a completely different messenger, a neuropeptide called Substance P, from binding to its NK-1 receptor.
If the 5-HT3 drugs are the guards at the perimeter, the NK-1 drugs are the agents inside the command center, ensuring that even if a signal slips through, it can't activate the final alarm.
These drugs are absolutely crucial for preventing delayed nausea—the kind that can creep up a day or two after treatment. Their development was a major leap forward in making many chemotherapy regimens far more tolerable for patients.
Adding an NK-1 antagonist to your regimen provides a much stronger shield, which is why we almost always use them for chemotherapy protocols known to have a high risk of causing nausea.
Reducing the Overall Alarm: Corticosteroids
The final piece of our security detail is often a corticosteroid, with dexamethasone being the one we use most commonly for nausea prevention. You might know steroids for their anti-inflammatory power, but they also have a potent anti-nausea effect.
Think of a corticosteroid as a tool that reduces the overall "sensitivity" of the entire alarm system. It works in several ways at once, including decreasing inflammation in both the brain and the gut and even boosting the effectiveness of the other anti-nausea medications.
This three-pronged strategy—blocking signals in the gut, blocking them again in the brain, and turning down the system's overall sensitivity—creates a robust, layered defense. This approach ensures you are protected from multiple angles, dramatically increasing the chances of getting through treatment with little to no nausea. The specific combination we choose is always based on your unique chemo drugs, your personal history, and our unwavering commitment to your comfort.
Practical Strategies for Everyday Nausea Relief
While your anti-nausea medications are the heavy lifters, don't underestimate the power you have to influence how you feel day-to-day. A handful of practical, non-medical strategies can work beautifully alongside your prescribed regimen, giving you a greater sense of control and comfort when dealing with chemo-induced nausea.
Think of these daily adjustments not as a replacement for your medical plan, but as a way to strengthen it. By being thoughtful about your diet, your surroundings, and even your state of mind, you create a much more stable foundation for your body to navigate treatment.

Mindful Eating and Hydration Habits
How you eat and drink can make a world of difference. The main goal is to avoid the extremes—you don't want your stomach to be completely empty, but you don't want it to be over-full either. Both can make queasiness worse.
Instead of three large meals, try switching to five or six smaller "mini-meals" or snacks spread throughout the day. This keeps your digestive system chugging along steadily without getting overwhelmed. An empty stomach is notorious for producing acid that triggers nausea, which is why keeping a few plain crackers on your nightstand to nibble on before you even get out of bed can be a game-changer.
When it comes to food choices, think bland and gentle. Your gut is extra sensitive right now, so foods that are easy to digest are your best friends.
- Good Choices: Things like plain toast, rice, bananas, applesauce, and yogurt are usually well-tolerated and easy on the stomach.
- Foods to Avoid: It's smart to steer clear of anything greasy, fried, spicy, or packed with sugar. These are common culprits for upsetting a sensitive system.
Staying hydrated is absolutely vital, but chugging a big glass of water can ironically make you feel full and nauseated. The trick is to take small, frequent sips of clear fluids all day long. Water is great, but clear broths and diluted juices are also excellent choices.
Dehydration is a major amplifier for nausea and fatigue. Simply keeping a water bottle with you at all times and sipping from it consistently is one of the easiest and most effective things you can do to feel better during treatment.
Calming Your Mind and Body
The connection between our minds and our guts is incredibly powerful, and that's especially true when you're under the stress of cancer treatment. Learning a few simple mind-body techniques can help soothe your nervous system, which directly helps in settling your stomach.
Deep, slow breathing is a fantastic tool to have in your back pocket. Try inhaling slowly through your nose for a count of four, holding your breath for a moment, and then exhaling slowly through your mouth for a count of six. This simple act can hit the pause button on your body's stress response and dial down that feeling of nausea.
Another technique many people find helpful is acupressure, which involves applying firm pressure to specific points on the body. The P6 (or Neiguan) point on the inner wrist is famous for its anti-nausea effects.
How to Find and Use the P6 Point:
- Hold one hand out with your palm facing up.
- Place the first three fingers of your other hand across your wrist, right at the base of your hand.
- The P6 point is right below your index finger, nestled between the two prominent tendons you can feel in your forearm.
- Use your thumb to apply firm, steady pressure to this spot for 2-3 minutes. Then, switch and do the same on the other wrist.
Managing Your Environment
During chemotherapy, it’s common for your senses to go into overdrive. Smells that never bothered you before can suddenly become overwhelming. Creating a calm, neutral-smelling space can make a huge difference.
Strong cooking odors are a very common trigger. If you can, try to avoid the kitchen when meals are being prepared. You might also find that cold or room-temperature foods are more appealing, as they tend to have much less of an aroma than hot foods. Cracking a window to let in fresh air can also work wonders to clear out any lingering smells.
Finally, don't forget that other side effects can be connected. Constipation, for instance, can contribute to a general feeling of discomfort and make nausea worse. If that’s an issue, exploring different approaches, including some natural remedies for constipation, might offer some relief.
For a deeper dive into nutrition, check out our guide on what to eat during chemotherapy. By layering these simple, practical tactics into your daily routine, you can build a much stronger defense against nausea.
How Your Oncology Team Personalizes Nausea Care
Let's be clear: managing nausea from chemotherapy is never a one-size-fits-all prescription. Your experience is yours alone, and your anti-nausea plan should reflect that. A truly dedicated oncology practice looks at you as a whole person, not just a diagnosis, to build a prevention strategy that’s made just for you.
Think of it as a collaborative partnership. Your oncology team acts like an architect, designing a custom support system to get you through treatment. They start with a detailed blueprint, mapping out several key factors to make sure the final plan is as strong and effective as possible. Here at Hirschfeld Oncology, this is the heart of how we care for our patients.
Building Your Unique Nausea Prevention Plan
The first thing we look at is the specific chemotherapy regimen you'll be receiving. This is the foundation. Different drugs carry different risks for nausea—some are almost certain to cause it, while others rarely do. We know the emetogenic (nausea-inducing) potential of every drug and use that knowledge as our starting point.
Next, we need to understand your personal history. It gives us crucial clues. Do you get terrible motion sickness on boats or in cars? Did you struggle with morning sickness during pregnancy? These past experiences can signal a higher sensitivity to nausea, telling us we might need to be more aggressive with your preventative medications right from the start.
Finally, we consider your emotional and psychological well-being. It’s a well-known fact that high anxiety can physically turn up the dial on nausea. We see this most clearly with anticipatory nausea. Knowing your anxiety level helps us build in supportive strategies that can help calm both your mind and your body.
The Power of Your Feedback
Once we have an initial plan, the real work begins—and it relies completely on you. Your feedback is the secret sauce that lets us fine-tune everything. Honestly, one of the most helpful things you can do is keep track of your symptoms.
A simple symptom journal, whether it's in a notebook or a phone app, provides invaluable information. Try to jot down:
- When you feel nauseous (a few hours after chemo? the next morning?)
- How severe it is on a scale of 1 to 10.
- What you were doing when it hit (e.g., right after eating, when smelling food).
- What made it better or worse, if anything.
This isn't just a diary; it's a direct feedback loop. It gives your care team the precise details we need to make smart, targeted adjustments.
Open communication is the engine of personalized care. When you share the specifics of your experience, you give your team the power to fine-tune your regimen—maybe by adding a "rescue" medication for breakthrough symptoms, adjusting a dose, or changing the timing of your pills.
This ongoing conversation ensures your nausea plan evolves right along with you. If something isn’t working perfectly, that’s not a failure. It’s just a new piece of information that gets us one step closer to the ideal solution for you. We might add a drug from a different class or suggest new non-drug strategies based on what you tell us is triggering your symptoms. To see more about how we use this collaborative process, take a look at our approach to personalized symptom management strategies during cancer treatment.
This proactive and responsive approach is all about protecting your comfort and quality of life. By treating you as an active partner in your care, we work to keep you feeling as well as possible throughout your entire journey.
When You Should Call Your Doctor About Nausea
Knowing when to pick up the phone and call your oncology team is a huge part of managing your treatment well. We work hard to create a plan that keeps chemo-related nausea from taking over your life, but sometimes, your body has other ideas.
Calling your doctor isn't admitting defeat; it’s being a smart, proactive partner in your own care. It’s how we keep you safe and stop small problems from turning into big ones. Your care team expects to hear from you if your symptoms are getting out of hand.
![]()
Clear Signs to Make the Call
Please don't "tough it out" if you're experiencing any of the following. These are red flags that your current anti-nausea plan isn't enough, and we need to step in to prevent complications like dehydration.
- Vomiting multiple times an hour for several hours: This is a clear signal that your body is losing fluids and essential electrolytes way too fast.
- Inability to keep any fluids down for more than 24 hours: This is the fast track to dehydration, which can become a serious medical issue surprisingly quickly.
- Feeling dizzy, weak, or lightheaded when you stand up: These are classic symptoms of dehydration setting in. Your body is telling you it needs help.
- Urinating less often or noticing dark, concentrated urine: Your urine is one of the best real-time indicators of your hydration level. Dark yellow or amber means you need more fluids.
Remember, your oncology team has a deep toolbox for fighting nausea. If plan A isn't cutting it, we have a plan B, C, and D. Our goal is always to find what works for you to keep you safe and feeling as good as possible.
Other Important Symptoms to Report
Beyond the most urgent signs of dehydration, there are a few other situations that absolutely warrant a call to your clinic.
Let us know right away if you have:
- Vomited your oral chemotherapy pills or other crucial medications.
- Started having significant stomach cramping or pain alongside the nausea.
- Developed a fever of 100.4°F (38°C) or higher.
Your team is here to help you through this. Open and honest communication is what allows us to tweak your plan and make sure you can get through treatment safely and with the best quality of life possible.
A Few Common Questions About Chemo and Nausea
It's completely normal to have questions as you prepare for chemotherapy, especially about a side effect as well-known as nausea. We hear these concerns all the time, so let's walk through some of the most common ones to give you a bit more clarity and peace of mind.
Is It Guaranteed That I Will Get Sick From Chemo?
Not at all. The old image of every chemo patient being constantly sick is thankfully very outdated. Whether you experience nausea really comes down to the specific drugs in your regimen, the dose you receive, and your own unique biology.
The truth is, modern cancer care is all about preventing nausea, not just treating it after it starts. Many of our patients get through their entire treatment course with little to no nausea whatsoever. At Hirschfeld Oncology, your anti-nausea plan begins before your first infusion, because getting ahead of the problem is the absolute best way to manage it.
Are Anti-Nausea Medications Safe to Take Regularly?
Yes, they are. The antiemetics we prescribe are a safe and essential part of your chemotherapy plan. Your oncology team chooses these medications carefully, matching them to your specific treatment and overall health.
We’ll keep a close eye on you for any side effects from the anti-nausea meds themselves, which are usually minor things like a headache or constipation. When you weigh that against the benefits of preventing severe nausea and avoiding serious issues like dehydration, these supportive drugs are a clear winner.
Key Takeaway: Don't think of your anti-nausea pills as an optional extra. They are a core part of your treatment, there to protect your quality of life and help you stay strong enough to complete your therapy successfully.
Can Changing My Diet Really Make a Difference?
Absolutely. While medication is your main defense, your diet is its powerful partner. The right food choices work alongside your prescriptions to keep nausea at bay and can make a huge difference in how you feel day-to-day.
A few simple shifts can have a surprisingly big impact:
- Eat Small, Frequent Meals: Instead of three big meals, try five or six smaller ones. This strategy keeps your stomach from getting too full or too empty, both of which can be major nausea triggers.
- Choose Bland Foods: Think simple. Crackers, toast, rice, and bananas are easy on the stomach and won't overwhelm your system.
- Avoid Triggers: It’s best to steer clear of anything greasy, spicy, heavily sweetened, or with a strong smell. These are the usual suspects when it comes to upsetting a sensitive stomach during chemo.
Staying hydrated is just as important. Taking small, slow sips of water or other clear liquids all day long is often much easier to tolerate than chugging a large glass. These small, consistent steps with food and drink can genuinely help you feel much better.
At Hirschfeld Oncology, we know that managing the side effects of treatment is just as important as the treatment itself. If you have more questions or want to learn about our personalized approach to cancer care, we invite you to explore our resources. Find out more at https://honcology.com/blog.





.png)


.png)
.png)




