Hearing you need chemotherapy naturally brings up one huge question: "What should I expect?"
The short answer is you can expect a planned journey. It starts with consultations to map out your treatment, moves into regular infusion sessions to receive the medication, and then into a recovery phase focused on helping you feel your best. While every person's experience is unique, modern cancer care is built around preserving your quality of life through it all.
Understanding Your Chemotherapy Journey
Starting chemotherapy can feel like being handed a map to a place you never planned to visit. Think of this guide as your compass. It's here to give you a clear, patient-focused look at what chemotherapy is, how it works, and what the road ahead might look like.
At its core, the idea behind chemotherapy is actually pretty straightforward.
Imagine your body is a garden. Cancer cells are like aggressive weeds that grow much faster and stronger than the healthy plants. Chemotherapy works like a highly targeted weed killer, with powerful medicines designed to find and stop these rapidly growing cells.
This selective approach is what makes it so effective. But, because some of your healthy cells also happen to be fast-growers—like the ones in your hair follicles or the lining of your digestive system—the treatment can sometimes impact them, too. This is what causes side effects.
Your Chemotherapy Journey at a Glance
Breaking your treatment down into phases can make the whole process feel much more manageable. Each stage has a clear purpose, from the initial planning sessions to your long-term wellness. To help you see the big picture, here's a high-level overview of the key stages you can expect.
While your specific timeline will be unique to you, most chemotherapy journeys follow a similar, structured pattern.
Setting Realistic and Hopeful Expectations
It's completely normal to wonder about how effective treatment will be. The statistics can offer real hope. For breast cancer, the overall five-year survival rate is a remarkable 90%, with chemotherapy being a critical tool in later stages.
Even in tougher situations, like pancreatic cancer where stage 4 five-year survival is typically under 3%, modern chemotherapy has made a significant difference. Advanced regimens have pushed the median survival in clinical trials from six months to over eleven months, showing just how much impact the right treatment can have. You can find more details in this overview of chemotherapy statistics.
The goal of modern oncology is not just to treat cancer, but to do so in a way that preserves your dignity and daily life. It’s about finding the right balance between powerful medicine and gentle care.
At Hirschfeld Oncology, we are dedicated to changing these expectations for the better with individualized, lower-toxicity approaches. We truly believe that effective cancer treatment should not have to come at the expense of your well-being.
By personalizing your treatment plan and keeping a close eye on your progress, we aim to minimize side effects while getting the best possible results. These modern strategies also influence how often chemotherapy is given, which you can read about in our detailed guide. This journey is a partnership, and our team will be right there with you, every step of the way.
How to Prepare for Your First Infusion
The time leading up to your first chemotherapy infusion can feel like a blur of nerves and logistics. That's completely normal. The best way to quiet some of that anxiety is to focus on what you can control. Getting organized now will make the treatment day itself feel much less intimidating.
Think of these next few days as your opportunity to set the stage for a smoother experience. A little preparation goes a long way, both for your time at the infusion center and for your comfort back at home.
Your Pre-Treatment Checklist
Your care team will give you a lot of information before your first appointment, and it’s easy to feel overwhelmed. Don’t try to memorize everything at once. Instead, just break it down into a simple checklist.
- Confirm Your Schedule: It sounds simple, but double-check the date, time, and location of your infusion. It’s also smart to ask how long the appointment is expected to last so you can plan your day and let others know.
- Arrange Transportation: You might feel perfectly fine after treatment, but you also might feel tired or a bit "out of it." It's a really good idea to arrange for a friend, family member, or ride-share service to get you home, especially this first time.
- Prepare Your Home: Set up a comfortable spot for yourself before you go. Stock your kitchen with simple, easy-to-digest foods and drinks. Have cozy blankets and pillows ready, and make sure things like the remote, your phone charger, and any medications are within easy reach.
- Review Insurance Details: Give your insurance provider a quick call to confirm your coverage for chemotherapy. Ask about co-pays or any pre-authorizations you might need. Getting this sorted out ahead of time prevents any unwelcome financial surprises.
Taking care of these small details frees you up to focus on yourself on treatment day.
Questions to Ask Your Oncology Team
Your oncologist and nurses are your partners in this. There is no such thing as a silly question, so please, ask away! The more you know, the more you'll feel like an active participant in your own care.
Clear communication isn't just a nice-to-have; it's a core part of a good treatment plan. When you ask questions, you give your team the insight they need to truly personalize your care.
It helps to jot down your questions as you think of them in a notebook or on your phone so you don't forget them during your appointment.
Questions About Your Treatment
- Can you tell me the name of the specific chemotherapy drug (or drugs) I’ll be getting?
- What is the main goal of this treatment for my type of cancer?
- How often will my infusions be, and how many cycles are we planning for right now?
Questions About Side Effects
- What are the most common side effects people experience with this particular regimen?
- When do those side effects usually start, and about how long do they last?
- Which symptoms are serious enough that I should call the clinic right away?
Getting these answers will help you know what to watch for and how to manage things as they come up.
Why Baseline Tests Are So Important
Before your first infusion, your care team will need to run a few tests, usually starting with blood work. This isn't just a formality—it's a critical safety step that gives us a clear picture of your health before we introduce any new medication.
These tests measure important things like your white and red blood cell counts, platelets, and how well your kidneys and liver are working. Think of it like a mechanic checking all the fluid levels in a car before taking it on a long road trip. We need to know that your body is in a good starting position.
This baseline data allows your oncologist to precisely tailor your chemotherapy dose, making sure it's strong enough to be effective but also as safe as possible for your body. If any of your levels are off, your team might adjust your treatment schedule or dosage to protect your health. This is personalization in action.
What Happens on a Chemotherapy Treatment Day
Walking into a cancer infusion center for the first time can feel like stepping into the unknown. It's completely normal to be a little anxious, but knowing the routine ahead of time can make a world of difference, replacing uncertainty with a sense of calm and control.
Your treatment day isn’t just a medical procedure; it’s a carefully managed process where your comfort and safety are the top priorities. You'll quickly get to know your infusion nurses—they are highly skilled oncology experts and, more importantly, your dedicated partners during every single visit.
Arriving and Getting Settled
A treatment day starts simply, a lot like any other doctor's visit: you'll check in at the front desk. From there, a team member will show you to your treatment chair, which is usually a comfortable recliner designed for you to settle in and relax.
Once you’re comfortable, your nurse will come by to check your vital signs. This is a quick but important checkup to make sure you’re ready for treatment. They'll measure your:
- Temperature to make sure there are no signs of infection.
- Blood pressure to get a baseline for the day.
- Pulse and breathing rate to check your overall stability.
- Weight, which is often used to calculate your precise medication dosage.
Starting the Infusion Process
Next, your nurse will establish vein access, usually with an intravenous (IV) line. This involves gently inserting a tiny, soft catheter into a vein in your hand or arm. If you have a port—a special device placed just under the skin for easier access—they’ll use that instead.
Before the chemotherapy itself begins, you’ll almost always receive pre-medications. These are supportive drugs given through your IV to head off potential side effects before they can even start. Most often, this includes anti-nausea medication and sometimes a steroid to help reduce inflammation. Think of it as a proactive step to keep you comfortable from the get-go.
The Infusion Itself: A Controlled Delivery
After the pre-meds are done, your nurse will begin the chemotherapy infusion. The best way to picture this is as a carefully controlled delivery. The medication flows through an infusion pump, a smart device programmed to deliver the exact dose at the precise rate your oncologist has ordered.
This pump ensures a safe, steady delivery over a specific period—which could be as short as 30 minutes or last for several hours, all depending on your treatment plan. Your nurse will be checking on you regularly throughout the entire infusion, making sure you’re feeling okay and that everything is running exactly as it should.
A chemotherapy infusion day is a quiet, steady process. The focus is on precision, safety, and your personal comfort, with your care team present every step of the way.
To help you visualize how to get ready, here’s a simple look at the key steps you can take before your treatment day.
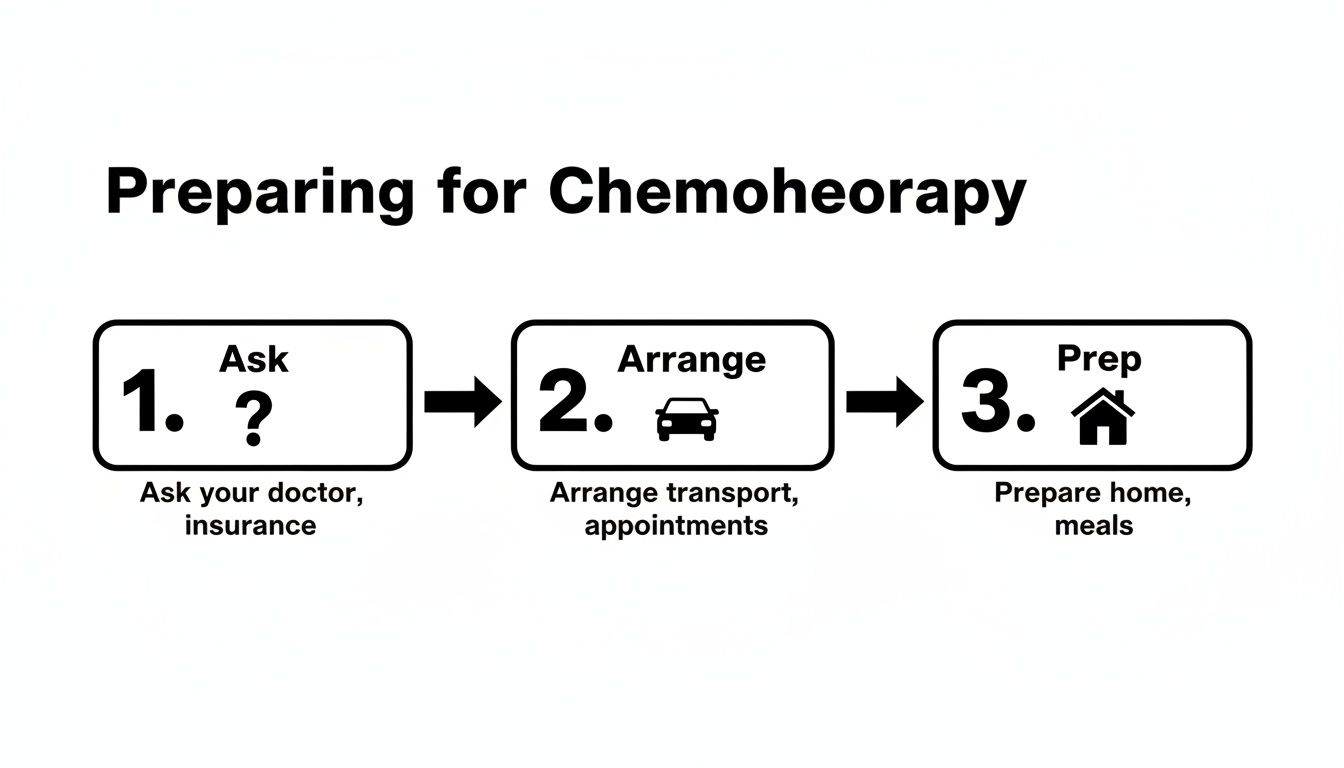
As you can see, preparing is all about asking the right questions, arranging your logistics, and getting your home prepped for comfort.
Making Your Time More Comfortable
You're not alone in this journey. In fact, chemotherapy is a central part of modern cancer care, and one study predicts the number of patients needing first-line chemo will rise by 53% to 15 million worldwide by 2040. All this experience has led to much better treatments and patient care, helping raise five-year cancer survival rates in the US from 75% to 90% in recent decades.
Since you might be at the clinic for a few hours, we always encourage you to bring things that help you feel relaxed and at ease.
What to Bring for Your Infusion
- Comfort Items: A warm blanket, a favorite pillow, or cozy socks can make all the difference.
- Entertainment: Pack a good book, a tablet with headphones for movies or music, or even a journal.
- Snacks and Drinks: We have some available, but having your go-to snacks and a water bottle is always a good idea.
- A Companion: You are more than welcome to bring a friend or family member for support and company.
Here at Hirschfeld Oncology, our team is here to walk you through every step, answer every question, and make sure you feel completely supported. To learn more about what to look for in a treatment facility, check out our guide on choosing a cancer infusion center near me.
Managing Common Chemotherapy Side Effects
When you're preparing for chemotherapy, one of the first things on your mind is often the side effects. The thought can be daunting, but understanding what might happen—and more importantly, knowing how you and your care team can manage it—can give you a real sense of control.
So, why do side effects happen in the first place? Chemotherapy is designed to be tough on fast-growing cancer cells. The problem is, it can't always tell the difference between those and your body's other fast-growing healthy cells. Think about the cells in your hair follicles, the lining of your mouth and gut, and your bone marrow.

The good news is that this impact on healthy cells is temporary. Most side effects fade away after treatment ends. And today, modern oncology has an incredible toolkit for preventing and soothing these symptoms, helping you maintain a much better quality of life through it all.
Understanding Fatigue and How to Cope
The fatigue that can come with chemo isn't just feeling tired. It's a bone-deep exhaustion that sleep doesn't always seem to fix. This is one of the most common side effects, affecting about 80% of patients. It happens because your body is working overtime to fight the cancer and repair the healthy cells affected by treatment.
Dealing with this kind of profound tiredness means rethinking your daily rhythm. It’s all about learning to conserve your energy for what truly matters to you.
- Listen to your body. Seriously. Don't try to power through the exhaustion. Give yourself permission to rest when you need it, even if that just means a few short naps.
- Prioritize your day. On days you feel a bit better, tackle your most important tasks. On low-energy days, let the less critical things slide. It's okay.
- Try some gentle movement. It sounds backward, but light activity like a slow walk around the block can actually boost your energy and lift your spirits.
Handling Nausea and Maintaining Nutrition
Nausea and vomiting are some of the biggest fears people have about chemo, but we've made huge progress here. With today's advanced anti-nausea medications, these symptoms are often controlled very well. Where over 70% of patients used to struggle with this, modern pre-medications have brought that number down drastically. Your care team will usually give you medicine right before your infusion to stop nausea before it even has a chance to start.
Even so, your appetite might not be what it used to be. The goal is simply to stay hydrated and get some nourishment in without overwhelming your system.
Practical Tips for Managing Nausea
- Eat small, frequent meals. Instead of three big meals, try five or six "mini-meals" throughout the day. This keeps your stomach from getting too full or too empty.
- Stick to bland foods. Things like crackers, toast, plain chicken, or rice are often much easier to handle when you're feeling off.
- Stay hydrated. Sip on clear liquids all day long. Water, broth, or ginger ale can work wonders. Dehydration is a sneaky culprit that can make nausea much worse.
Think of symptom management as a partnership. Your care team provides the medical tools, and your self-care provides the daily support. Open communication is the key that makes it all work together.
Hair Loss and Skin Changes
Hair loss, or alopecia, happens to about 65% of people on chemotherapy, but this is one side effect that really depends on the specific drugs in your regimen. Some treatments cause significant thinning or complete hair loss, while others cause none at all. Be sure to ask your oncologist what's typical for your treatment plan. If hair loss is likely, it usually starts two to four weeks after your first infusion.
Remember, this is almost always temporary. Your hair will grow back after your treatment is finished. In the meantime, many people find that scarves, hats, or wigs help them feel more like themselves.
Your skin may also get more sensitive during treatment, becoming dry or easily irritated. Treat it gently. Use mild, unscented soaps and lotions, and be religious about applying sunscreen—your skin will be much more sensitive to the sun.
When to Call Your Care Team
While you can manage most side effects at home, some symptoms need immediate medical attention. Your team is here to help you, and it is always, always better to call if you aren't sure about something.
Call your clinic right away if you experience:
- A fever of 100.4°F (38°C) or higher
- Chills or uncontrollable shaking
- Vomiting or diarrhea that just won't stop
- Shortness of breath or chest pain
- Any signs of an infection, like new redness, swelling, or a cough
At Hirschfeld Oncology, we build our treatment plans around innovative, lower-toxicity options designed to reduce these issues from the start. By focusing on approaches to minimizing side effects during cancer treatment, we can often achieve the same powerful results while helping you feel significantly better throughout your journey.
A Patient-First Approach to Chemotherapy
When most people hear the word “chemotherapy,” their minds often jump to a pretty harsh picture: aggressive, one-size-fits-all treatments with draining side effects. But that image is becoming more and more a thing of the past. At Hirschfeld Oncology, we champion a modern, patient-first philosophy that changes the entire experience.
We’re moving beyond the old-school idea that “more is better.” Instead, we focus on treatments that are just as effective against cancer but far gentler on your body. It's about finding that sweet spot where we can control the disease while preserving—and even improving—your quality of life.
Turning Down the Volume with Low-Dose Chemotherapy
One of the cornerstones of this approach is metronomic chemotherapy, which many people know as low-dose chemo. Imagine you’re listening to music. You don't have to blast it at full volume to hear every note. Sometimes, a lower, more consistent volume is just as powerful and much more comfortable. That’s exactly what metronomic chemo does.
Rather than hitting the body with the highest dose it can tolerate every few weeks, we use smaller, more frequent doses. This steady, gentle pressure attacks the cancer in a different way. It not only targets cancer cells directly but also works behind the scenes to disrupt the tumor's life-support systems, like its blood supply.
We think of it as a ‘less is more’ strategy. It often leads to far fewer and milder side effects, allowing you to keep living your life with energy and comfort while the treatment works.
This method can be a game-changer, especially for patients with advanced cancers or for anyone who might struggle with the intensity of traditional high-dose regimens. It shifts the experience from a grueling battle to a sustainable, manageable part of your life.
Your Treatment, Your Way
A truly patient-first approach means your treatment plan is designed specifically for you, and you’re a key partner in its design. This is a collaborative journey, and the plan can change and adapt based on how you’re feeling and what your goals are. We’re not just following a rigid protocol; we’re creating a personalized roadmap that makes sense for you.
This kind of partnership is built on a few important principles:
- Close and Continuous Monitoring: We keep a close eye on your progress through regular check-ins, blood work, and scans. This lets us make quick adjustments to your treatment on the fly, making sure it’s always working as effectively and gently as possible.
- Collaborative Decision-Making: You are the most important person on your care team. Your input—how you’re feeling, what’s important to you—is essential and directly shapes the decisions we make together.
- Proactive Symptom Management: We don’t wait for side effects to become a problem. We get ahead of them. Our goal is to prevent discomfort from the very beginning so you can feel your best throughout treatment.
Restoring Hope and Quality of Life
At the end of the day, our modern approach to chemotherapy is about so much more than just fighting cancer. It’s about restoring hope. We believe that your well-being, your ability to enjoy your hobbies, and your time with family are just as important as any lab result.
By focusing on strategies that reduce toxicity and prioritize your comfort, we can fundamentally change what it means to go through chemo. It becomes a treatment that works with your body, not against it. This gives you the best shot at a great outcome while letting you live the life you love.
Your Top Questions About Chemotherapy, Answered
Starting chemotherapy brings up a lot of questions—not just about the medicine itself, but about how it will fit into your real, day-to-day life. Getting straight answers can help you and your family feel more prepared and in control.
Here are some of the questions we hear most often from patients just like you.
Can I Still Work During My Chemotherapy Treatment?
For many people, the answer is yes, though it almost always requires a few adjustments. Whether you can keep working really depends on the type of treatment you’re receiving, how you feel, and what your job entails.
Our lower-toxicity approach is actually designed with this in mind—to help you maintain your quality of life, which for many, includes continuing to work. It’s pretty common for us to schedule treatments on a Friday, for example, giving you the weekend to rest and recover before heading back to work on Monday.
Ultimately, the best advice is to listen to your body. Don't push yourself too hard. Being open with your employer about what you need and keeping your care team in the loop is the key to finding a rhythm that works for you.
How Will We Know if the Chemo Is Working?
Figuring out if your treatment is effective is a team effort—a continuous conversation between you and your oncology team. It's not a one-time check, but a series of checkpoints that build a clear picture of your progress.
We use a few key tools to see how your body is responding:
- Regular Blood Tests: We look for specific "tumor markers"—substances that can signal the presence of cancer activity.
- Imaging Scans: CT or PET scans, usually done every few cycles, give us a direct look at the tumors to see if they are shrinking.
- How You Feel: This one is just as important as any test result. A drop in cancer-related symptoms, like pain or fatigue, is often one of the best signs that the treatment is doing its job.
Your doctor will walk you through all of these results, every step of the way, explaining what they mean and how they help us plan what’s next for your care.
Think of it as a constant feedback loop. Your test results and how you’re feeling work together, giving your care team the information they need to keep your treatment precisely on track.
What Is the Difference Between Low-Dose and Standard Chemo?
The main difference comes down to the dose and the schedule, which completely changes the experience for the patient.
Imagine standard chemotherapy as a powerful but infrequent blast. It often uses the maximum tolerated dose of a drug, followed by a long break to let your body recover from the intensity.
On the other hand, low-dose (or 'metronomic') chemotherapy is a steadier, more continuous approach. We use much smaller doses of medication given more frequently. The goal isn’t just to hit the cancer cells hard; it’s also to disrupt their supply lines, like cutting off their blood supply and helping the immune system keep them under control.
This gentler, more consistent method is usually much easier on the body, leading to far fewer and less severe side effects. This allows you to maintain a much better quality of life while still fighting the cancer effectively.
How Important Is My Diet During Treatment?
What you eat is a genuinely powerful part of your cancer care. Your body is working overtime to heal and fight, and it needs the right fuel—especially extra calories and protein—to keep up. But we also know that treatment side effects can make eating feel like a real chore.
The best strategy is often to shift from three large meals to several small, frequent ones throughout the day. This can help keep nausea at bay and your energy levels much more stable.
Simple Nutrition Tips During Chemo
- Stay Hydrated: This is non-negotiable. Being dehydrated can make fatigue and nausea so much worse. Keep water, clear broths, or electrolyte drinks handy and sip on them all day.
- Make Every Bite Count: When your appetite is low, focus on nutrient-dense foods. Things like avocados, nut butters, eggs, and full-fat yogurt pack a lot of nutrition into a small package.
- Go Bland When Nauseous: If your stomach is upset, simple foods are your best friend. Crackers, toast, rice, and plain baked chicken are often much easier to tolerate.
Don’t ever hesitate to talk to your care team about challenges with eating. We can give you more specific advice or connect you with a nutritionist to build a plan that truly supports you.
At Hirschfeld Oncology, we believe answering your questions is one of the most important things we do. If you have more questions or want to explore a personalized, lower-toxicity treatment plan, we invite you to learn more on our blog.





.png)


.png)
.png)




