When you're facing a bile duct cancer diagnosis, it’s easy to feel lost. But it's important to know that clinical trials can be a powerful, proactive step forward in your treatment. These aren't just experiments; they are carefully planned research studies that open the door to the very latest in medical science, often years before these treatments are available to everyone.
Why Clinical Trials Matter for Bile Dect Cancer
For many people, particularly those with advanced or complex cholangiocarcinoma, a clinical trial can represent a new avenue of hope. It’s best to think of them not as a last resort, but as a chance to partner with top cancer experts on the cutting edge of research. Every single study is designed to find safer, better ways to treat this specific cancer.
Joining a trial is a true partnership. You get access to innovative therapies and receive care from specialists who are dedicated to finding the next breakthrough. At the same time, your participation adds to the collective knowledge that will help guide the treatment of every person diagnosed with bile duct cancer in the future.
Charting a New Path for a Rare Cancer
Because bile duct cancer is relatively rare, research has historically been challenging. This aggressive cancer accounts for only 3% of all gastrointestinal cancers worldwide, which has meant fewer clinical trials compared to more common cancers.
But the tide is turning. We're seeing a significant and encouraging shift. Patient enrollment in clinical trials for bile duct cancer has jumped to 7.1%, a huge leap from the 2-3% we saw in previous years. This signals a major increase in research focus and more opportunities to find new, effective therapies. You can discover more about this positive trend in cholangiocarcinoma trial participation on honcology.com.
This progress is happening because scientists now have a much deeper understanding of the disease's biology, which allows them to develop more precise and targeted treatments.
"A clinical trial is much more than an experiment; it's a structured, proactive, and powerful choice in your treatment journey. It's about exploring a new, promising map in the fight against cancer, where every participant helps define the path forward."
The Core Purpose of a Trial
Every single cancer treatment used today—chemotherapy, targeted therapy, immunotherapy—was first proven safe and effective in a clinical trial. These studies are built to answer very specific questions that directly improve how we care for patients. To get a broader look, you can check out our complete guide to cancer clinical trials.
The main goals usually boil down to a few key areas:
- Evaluating New Treatments: Does a new drug, like a targeted therapy or immunotherapy, work better than the current standard treatment?
- Finding Better Combinations: Can we combine existing treatments in a new way to get better results or cause fewer side effects?
- Improving Quality of Life: Can we find better ways to manage symptoms and treatment side effects, helping patients feel better during and after their therapy?
Understanding what a trial is—and what it isn't—helps you see it as an informed, empowered choice you make with your medical team, rather than a leap into the unknown.
How Different Phases of Cancer Trials Work
When we talk about clinical trials for bile duct cancer, it’s not a single event but a carefully planned journey broken into distinct stages. Think of it like a scientist running a series of experiments, where each one builds on the last. The absolute priority at every step is patient safety, followed closely by figuring out if a new treatment actually works.
This methodical process ensures that by the time a therapy is approved for widespread use, it’s been put through its paces. Each phase is designed to answer a different, crucial question.
Phase I: The Safety Check
The first stop is Phase I. These trials are small and laser-focused on one thing: safety. The main goal isn't to see if the treatment cures cancer, but to determine the safest dose and to watch for any serious side effects.
Researchers start with a very low dose and slowly increase it, monitoring participants incredibly closely. It's the essential groundwork. You have to know a treatment is safe before you can ever find out if it's effective.
Phase II: The Effectiveness Test
Once a safe dose is established in Phase I, the treatment moves on to Phase II. Here, the group of patients is a bit larger, and the big question becomes: does this actually work on bile duct cancer?
Investigators measure whether the treatment shrinks tumors or at least stops them from growing. This phase is a critical filter. A lot of promising ideas don't make it past this stage, but the ones that show a real, positive impact on the cancer are the ones that move forward.
A clinical trial is a carefully planned expedition, broken down into distinct stages. Each phase builds on the one before it, guided by one constant principle: keeping patients safe while determining if a new treatment truly works.
Phase III: The Comparison Stage
Phase III is the big one. These are large-scale trials, often involving hundreds, sometimes thousands, of patients across many different hospitals and cancer centers. The goal here is simple: comparison.
The new treatment goes head-to-head with the current "standard of care"—the best treatment that’s already available. To be considered a success, the new therapy has to prove it’s at least as good as, and ideally better than, what doctors are using today. This is the final, most rigorous test before a drug can be approved by regulatory bodies like the FDA.
The timeline below shows just how much the landscape for rare cancers like this has changed. We've gone from a period of scarcity to one of real, tangible momentum.
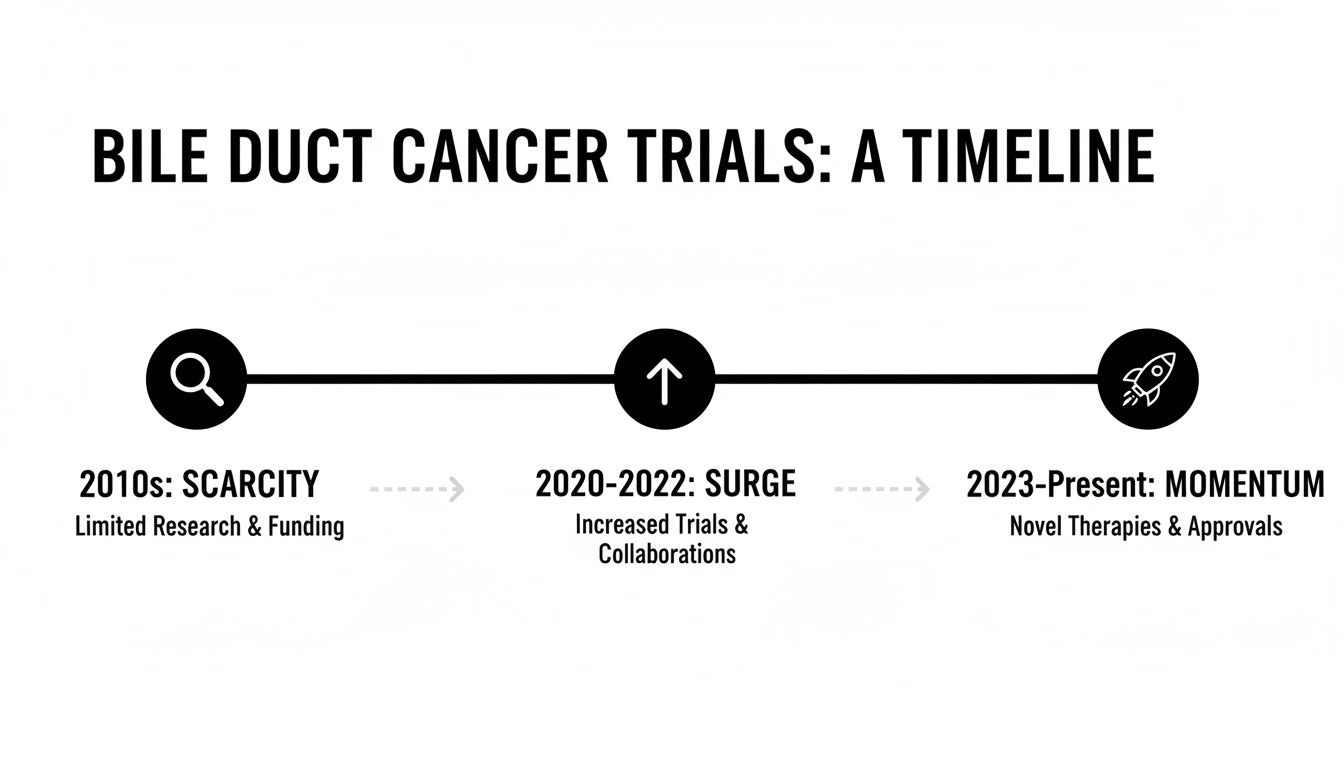
This incredible progress is largely thanks to the development of targeted therapies, which are giving new hope and encouraging more patients to participate in these vital studies.
To get a clearer picture, here’s a simple breakdown of what each phase sets out to accomplish.
Clinical Trial Phases at a Glance
As you can see, the process is designed to gather more and more evidence at each step, moving from small-scale safety checks to large-scale comparisons.
Phase IV: Long-Term Monitoring
Even after a drug is approved and available to patients, the research doesn't stop. Phase IV trials, often called post-marketing surveillance, continue to track the treatment's effects in the real world over many years.
This final step helps researchers find any rare or long-term side effects that might not have appeared in earlier trials. It’s all about ensuring the treatment remains a safe and valuable option for the long haul.
This careful, step-by-step process is what gives us confidence in new treatments. In fact, the success of targeted therapies coming out of these trials has led to a major jump in trial enrollment, now up to 7.1% from a historical average of just 2-3%. That's because these newer drugs are showing a 42% overall response rate for tumors with specific FGFR2 and IDH1 genetic changes. You can dive deeper into these advancements and the data behind them on the Cholangiocarcinoma Foundation website.
Is a Clinical Trial the Right Path for You?
Not every clinical trial is a fit for every patient, and that's by design. Before a study even begins, researchers lay out a very specific set of rules called eligibility criteria. It’s a bit like casting for a play—the director needs actors with particular traits to tell a coherent story. In the same way, researchers need a well-defined group of participants to produce clear, reliable results.
These rules fall into two main buckets:
- Inclusion Criteria: These are the must-haves. For instance, a trial might require you to have a specific type of bile duct cancer, be at a certain stage, or have already gone through a particular prior treatment.
- Exclusion Criteria: These are the factors that would unfortunately rule you out. This could be anything from having another health condition to taking a certain medication that might interfere with the study drug.
These criteria aren't there to create roadblocks. They are absolutely critical safeguards put in place to protect you and ensure the new treatment is a safe and appropriate match for your specific medical situation.
What Factors Determine Eligibility?
As you and your oncologist start exploring clinical trials for bile duct cancer, you’ll see that the eligibility criteria can get very specific. This isn't just bureaucracy; it's what makes modern cancer research so powerful. It allows scientists to test promising new drugs on the precise group of patients they are most likely to help.
Some of the most common factors you'll encounter are:
- Cancer Stage and Type: Is the cancer locally advanced or has it spread (metastatic)? One trial might be for one, and a different trial for the other.
- Treatment History: Some studies are designed for patients who are newly diagnosed and haven't had any treatment yet. Others are specifically for people whose cancer has progressed after standard chemotherapy.
- Overall Health: Researchers need to be confident that a participant is well enough to handle the potential side effects of a new therapy. Doctors often use a performance status scale to measure this.
This careful, structured approach is what makes the final data meaningful and scientifically sound.
"Think of eligibility criteria not as barriers, but as a blueprint for safety and scientific clarity. They make sure the right patient gets into the right study, which is the best way to maximize the potential for benefit while minimizing risk."
The Crucial Role of Genetic Markers
One of the biggest shifts in cancer care over the last decade has been the focus on a tumor's unique genetic profile. Today, many clinical trials for bile duct cancer are built around specific biomarkers or genetic mutations found within the cancer cells. If you're new to this concept, you can get up to speed with our guide explaining what cancer biomarkers are.
For cholangiocarcinoma, a few key markers can open doors to specific trials:
- FGFR2 fusions: We see these in about 10-16% of intrahepatic cholangiocarcinomas.
- IDH1 mutations: These are present in roughly 20% of intrahepatic cases.
- HER2 amplifications: This is an important target in a smaller group of patients.
If your tumor has one of these genetic "fingerprints," you could be a perfect candidate for a targeted therapy trial—a study testing a drug designed to attack that exact weakness. This is precisely why getting comprehensive genomic testing done on your tumor tissue is so incredibly important. It can reveal opportunities for personalized treatments that simply weren't on the table before.
Knowing this information allows you to have a much more focused, productive conversation with your oncologist about which trials might truly be the best fit for you.
How to Find and Access Bile Duct Cancer Trials
Finding the right clinical trial can feel like searching for a needle in a haystack, but you’re not alone in this. Your oncologist is your primary guide, but learning how to navigate the available resources yourself can be incredibly empowering. It puts you in the driver's seat.
The best place to start is almost always ClinicalTrials.gov. Think of it as the central library for medical research—a massive, government-run database that lists studies happening all over the world. It’s the most complete, up-to-the-minute picture of what's happening in cholangiocarcinoma research right now.

Using Online Databases Effectively
At first glance, a site like ClinicalTrials.gov can seem overwhelming. The key is using its filters to cut through the noise and zero in on what truly matters for your situation. With a methodical approach, you can quickly turn a huge list into a handful of real possibilities.
Here’s a simple way to get started:
- Start with Your Condition: In the "Condition or disease" box, just type "cholangiocarcinoma" or "bile duct cancer." This makes sure every result is relevant.
- Pinpoint Your Location: Use the filters to select your country, state, and even your city or zip code. This helps you find studies close to home.
- Find Open Trials: This is a crucial step. Under "Recruitment Status," make sure you select "Recruiting." This weeds out any studies that are no longer accepting new patients.
The search platform is designed to help you find trials that fit your life, both medically and geographically. Another fantastic resource is the National Cancer Institute (NCI) portal, which offers a curated list of cancer-specific trials and other helpful patient information.
How to Understand a Trial Listing
Once you have a list of potential trials, the next step is learning to read the listings. Every study has a detailed description, often called a protocol, that acts as its rulebook. The language can be technical, but focusing on a few key sections will give you the information you need.
- Purpose of the Study: This is a plain-language summary of what the researchers are trying to learn. Is it a new drug? A different combination of old drugs? This section tells you the "why" behind the trial.
- Eligibility Criteria: This is the most important part for you. It lists the specific "inclusion" and "exclusion" rules for who can join. Pay close attention to details like the stage of your cancer, what treatments you've had before, and if certain genetic markers are required.
- Locations and Contacts: This part is straightforward. It tells you exactly where the trial is being held and gives you contact info for a research coordinator—the person who can answer your initial questions.
Your oncologist is your best resource for decoding a trial listing. They can read through the protocol with you, translate the medical jargon, and quickly determine if a study is a good match, saving you time and focusing your efforts.
The Role of Your Oncology Team in NYC
While these online databases are powerful, they don’t replace the expertise of your oncology team. For patients in the New York City area, working with an experienced oncologist provides a real advantage. A specialist can help you interpret the complex details of a trial and may even know about studies at leading local institutions that you might not easily find on your own.
At Hirschfeld Oncology, we are dedicated to helping our patients explore every single option. We can sit down with you, review potential trials, and discuss how they fit into your specific diagnosis. We can also help facilitate connections with the right research centers here in the NYC area.
A consultation is often the best first step to clarifying your path forward. By combining the expertise of your doctor with these incredible online tools, you can confidently explore recent clinical trial highlights and find a study that is right for you.
Navigating the Enrollment Process

Finding a clinical trial that feels right is a major milestone. The next part of the journey is the enrollment process, which is carefully structured to protect you and ensure the research is solid. It boils down to two main stages: a detailed screening period to confirm you're a good fit and the informed consent process.
The whole thing starts with verifying your eligibility. Every trial operates on a strict blueprint, called a protocol, that lists out specific inclusion and exclusion criteria. It’s a bit like casting for a role—the researchers need participants with very particular characteristics to get clear, trustworthy results. This step is what allows them to confidently say whether the new treatment worked.
The Screening Process
Before you can officially enroll, you’ll go through a thorough screening phase. This involves a series of tests to double-check that the trial is both safe and appropriate for your specific health situation. It’s all about protecting you and preserving the integrity of the research data.
Typically, screening includes a few key steps:
- Medical History Review: The research team will take a deep dive into your health records, looking at past treatments, other conditions, and your overall medical journey.
- Physical Examination: You’ll have a complete physical to establish a baseline for your current health.
- Imaging Scans: Expect to get new CT, MRI, or PET scans. These give the team the most current picture of the cancer’s status.
- Blood and Tissue Samples: Lab work is crucial for checking things like your liver and kidney function. Often, a recent tumor biopsy is also required to look for the specific genetic markers the trial is targeting.
This whole process can take a few weeks. That wait can feel like an eternity, I know, but every single step is an essential safety check.
The Informed Consent Conversation
If the screening process confirms you’re a match, the next step is informed consent. This is so much more than just signing a piece of paper. It’s an open and ongoing conversation with the research team where you can get all your questions answered. The goal is to give you all the information you need to make a decision that you’re truly comfortable with.
Informed consent is a fundamental patient right. It guarantees you are an active partner in your care, fully aware of the trial’s purpose, what it involves, and the potential risks and benefits before you agree to anything.
You'll be given a consent form, which is a detailed document that lays out everything—the trial's goals, the treatment schedule, and a transparent discussion of potential side effects. Take it home. Read it over, discuss it with your family or a trusted friend, and write down any questions that pop into your head. Seriously, no question is too small or silly.
And remember, joining any clinical trial for bile duct cancer is completely your choice. You have the right to withdraw from the study at any time, for any reason, and it won't affect your access to standard medical care. This whole process is designed to build a partnership based on trust, putting you in the driver’s seat of your treatment journey.
2. Weighing the Benefits and Potential Risks
Deciding whether to join a clinical trial for bile duct cancer is a big decision, and it’s not always a straightforward one. It's a deeply personal choice that really comes down to balancing the hope for a medical breakthrough against the realities of testing something new.
Let's walk through both sides of the coin so you can get a clearer picture.
What Are the Potential Benefits of Joining a Trial?
For many people, the biggest draw is gaining access to treatments on the absolute forefront of science. These are therapies that could be years away from being widely available, offering a new potential option when standard treatments have run their course.
When you join a trial, you're not just a patient; you become a partner in the research process. You’ll be under the care of leading oncologists and scientists who live and breathe cholangiocarcinoma research. This often means incredibly close monitoring and a level of specialized attention that can be very reassuring.
But your participation reaches far beyond your own health. It’s an act that pushes the entire field of cancer research forward.
- You help advance medical knowledge. Your experience provides the real-world data researchers desperately need to figure out if a new therapy is safe and effective.
- You improve care for future patients. You become a direct part of the process that could establish a new standard of care, helping countless people who will be diagnosed down the road.
- You offer hope to the entire community. Your involvement sends a powerful message that we are all actively fighting for better answers.
This contribution is more vital than ever. The field is moving so fast, with new trials now targeting specific genetic markers like NTRK, RET, BRAF, FGFR2, and IDH1. This is why detailed molecular testing has become a game-changer, unlocking doors to these new treatment opportunities.
Understanding the Potential Risks and Downsides
It's just as important to be realistic about the potential downsides. The biggest unknown is that the new treatment simply might not work better than the standard of care—or it might not work for you specifically. A clinical trial is, by definition, an experiment, and a positive outcome is never a guarantee.
Side effects are another major consideration. Since the treatment is new, you might experience side effects that are unexpected or even more severe than those from standard therapies. The research team will be watching you like a hawk for any issues, but this is a critical conversation to have with your doctor and family.
Finally, you have to think about the practical side of things. Participating in clinical trials for bile duct cancer can be a significant commitment of your time and energy.
This could involve:
- More frequent trips to the hospital or clinic for treatments and follow-ups.
- Extra tests, like blood draws, biopsies, or scans, that are required by the study protocol.
- The possibility of travel if the trial site isn't located near your home.
These logistical hurdles are a very real part of the experience. Thinking through all of these factors—the scientific, the personal, and the practical—is the best way to make a fully informed decision that feels right for you.
Evaluating Participation in a Bile Duct Cancer Trial
To help put it all in perspective, here is a balanced look at the pros and cons you'll want to consider when making your decision.
Ultimately, weighing these points is a personal journey. There is no single "right" answer, only the one that aligns with your health goals, your support system, and your outlook.
Common Questions About Cancer Clinical Trials
Deciding whether to join a clinical trial is a huge step. It’s completely normal to have a lot of practical questions running through your mind. You're not just thinking about the science; you're trying to understand how this fits into your life, your finances, and your family's future. Let's walk through some of the most common concerns we hear from patients looking into trials for bile duct cancer.
Will My Insurance Cover a Clinical Trial?
This is usually the first question people ask, and thankfully, the answer is pretty straightforward. By law, most health insurance plans must cover the routine patient care costs when you're in a trial. Think of these as the medical services you’d need anyway, like standard doctor visits or hospital stays, even if you weren't in the study.
So, what about the new stuff? The trial sponsor—typically a research institution or a pharmaceutical company—is responsible for all the research-related expenses. That means the investigational drug itself, plus any extra tests, scans, or procedures required specifically for the study, are covered. Still, it's always a good idea to chat with the trial's financial coordinator and call your insurance provider to get a crystal-clear picture before you start.
Can I Leave a Trial After It Starts?
Yes, absolutely. Your participation is 100% voluntary from beginning to end. You have the right to leave a trial at any time, for any reason. Your decision won't affect your access to standard medical care in any way. This is a core patient right, and it's a huge part of the informed consent process.
If you do decide to withdraw, you just need to let the research team know. They’ll make sure you can stop the trial treatment safely and will help you transition smoothly to the next step in your care plan.
How Is Patient Safety Ensured?
Patient safety isn't just a priority in a clinical trial—it's the priority. The moment you enroll, you'll have a dedicated team of doctors and nurses watching over your health with incredible care, ready to jump in and manage any side effects that pop up.
In the United States, every single trial has to be approved and continuously monitored by an Institutional Review Board (IRB). This is an independent committee of doctors, scientists, and even people from the community whose entire job is to protect the rights and well-being of every participant.
What Happens When the Trial Ends?
Your care doesn't stop when the study does. Once the trial is over, the research team will sit down with you to discuss what comes next, based on your health and what they learned from the study.
If the new treatment worked well for you, you might be able to keep receiving it through a special access program. If it wasn't effective, your team will help you move back to standard care or explore other options, which could even include a different clinical trial. You will always have a clear, supportive plan for the road ahead.
This whole process is so important because researchers are constantly pushing for better therapies. The hard truth is that survival for bile duct cancer depends heavily on its stage. It drops from 35-45% at five years for an early-stage tumor that can be removed with surgery, down to almost zero for cancer that has spread. This is the reality that drives innovation in studies like the NCT04941287 trial, which is testing new treatment combinations for advanced cases. You can read more about the research driving these new approaches and their impact.
At Hirschfeld Oncology, we know that figuring out clinical trials can feel overwhelming. Our team is here to bring clarity, answer your questions, and help you explore every option on the table. To discuss what might be next for you, please visit us at https://honcology.com/blog.





.png)


.png)
.png)




