When you’re facing chemotherapy, one of the first questions that comes to mind is almost always, "How long will the side effects last?" It’s a completely valid and important question, but the answer isn't a simple one.
The reality is, your experience will be unique. While some side effects like nausea might hit quickly and fade before your next infusion, others, like fatigue, can stick around for weeks or even months after treatment ends. Everything depends on the specific drugs you receive, your dosage, your overall health, and how your body responds.
Understanding Your Chemotherapy Side Effect Timeline
Let's demystify what you can generally expect. Instead of a single, long road, think of the side effect timeline in distinct phases. Knowing what might happen—and when—can help you feel more in control and prepared.
This guide is here to walk you through those phases, giving you a clearer picture of the journey ahead so you can move from a place of uncertainty to one of empowerment.

Breaking Down the Recovery Process
It's helpful to think of the recovery process in waves. Some effects are immediate and intense, while others build slowly over time. We can generally group them into three main categories:
- Acute Effects: These are the reactions that show up right away, usually within the first 24 to 48 hours after a treatment session.
- Delayed Effects: This group includes symptoms that might not appear for several days or even a couple of weeks after your infusion.
- Long-Term Effects: Finally, some side effects can linger for months or years after all treatment is finished, sometimes requiring ongoing attention.
Getting a handle on these phases is the first step. While your path is your own, these patterns provide a framework for managing symptoms and having more productive conversations with your care team. If you want a broader look at the entire process, you can learn more about what to expect from chemotherapy in our comprehensive guide.
The goal is to move beyond the fear of the unknown. Knowing that some side effects are temporary and others follow a predictable course gives you a framework for your recovery, helping you focus on one day at a time.
It’s also important to remember that these timelines aren't set in stone. Modern, personalized treatment plans—like those we design at Hirschfeld Oncology—are specifically created to reduce the severity and shorten the duration of these challenges. By tailoring therapy to your unique cancer and individual health, our primary goal is to protect your quality of life every step of the way.
The Three Phases of Chemo Side Effects Explained
When you're trying to wrap your head around how long chemo side effects might last, it helps to stop thinking of it as one big, unpredictable event. It’s more like the ripples from a stone tossed into a pond—some are immediate and sharp, while others are slower, wider, and stick around for a while.
Thinking about it in phases gives you a kind of mental map for your treatment journey. It helps make sense of why some issues pop up right after an infusion while others don't show up for weeks, and why managing them is an ongoing process, not just a one-time fix.
Phase 1: The Acute Effects
The first wave of side effects are what we call acute effects. These are your body's immediate reactions to the chemotherapy drugs, typically showing up within the first 24 to 48 hours after an infusion. You can think of this as the initial shock to your system.
Some of the most common acute effects include:
- Nausea and Vomiting: This is often the most dreaded side effect, and it usually starts within hours of treatment. The good news is that modern anti-nausea medications are incredibly effective at either preventing it or dialing it way back.
- Allergic Reactions: During or just after an infusion, some people might experience flushing, a rash, or other signs of a reaction.
- Initial Fatigue: A first wave of tiredness can hit as your body starts to process the powerful drugs it just received.
These acute symptoms tend to be intense but don't last very long. Your oncology team has a whole arsenal of tools to manage them, often giving you pre-medications before your infusion even begins to stay ahead of any discomfort.
Phase 2: The Delayed Effects
Once the initial ripples have calmed down, a new set of waves can start to roll in. We call these delayed side effects, and they tend to develop several days or even a couple of weeks after a treatment cycle. This happens because chemo needs time to work on the lifecycle of both cancer cells and healthy, fast-dividing cells.
This is the phase where the treatment’s cumulative impact on your body’s various systems really starts to show.
A Note from Experience: The delayed phase is often when the real day-to-day impact of chemo is felt most strongly. While the acute effects feel like a sprint, the delayed ones can be more of a marathon, requiring patience and consistent self-care.
Common delayed side effects include:
- Profound Fatigue: This isn't just feeling tired. It's a deep, bone-wearying exhaustion that, for many people, becomes the most disruptive side effect of all.
- Mouth Sores (Mucositis): Painful sores can pop up on the lining of your mouth and throat about 5 to 14 days after treatment.
- Hair Loss (Alopecia): This usually starts 2 to 4 weeks after your first dose, as the drugs begin to affect your hair follicles.
- Changes in Blood Counts: Your levels of white blood cells, red blood cells, and platelets will dip, usually hitting their lowest point (what we call the nadir) around 7 to 14 days after treatment. This is when your risk of infection and fatigue is highest.
Phase 3: The Long-Term Effects
Finally, we have the effects that can stick around long after your last infusion. These are known as long-term or late side effects. They can persist for months, years, or, in some cases, become permanent. They’re often the result of cumulative damage to healthy cells over the entire course of your treatment.
The point of understanding these potential issues isn't to cause worry, but to empower you to be proactive about your health for years to come. This is a huge part of survivorship care.
Examples of long-term effects include:
- Peripheral Neuropathy: Nerve damage that causes tingling, numbness, or pain, most often felt in the hands and feet.
- Cognitive Changes ("Chemo Brain"): Many people describe lingering issues with memory, focus, and multitasking after treatment ends.
- Organ-Specific Issues: Depending on the specific drugs used, there can be lasting effects on the heart, lungs, kidneys, or your fertility.
The possibility of these lasting effects is exactly why a thoughtfully managed treatment plan is so essential. A good oncologist will always weigh a drug's benefits against its potential for long-term toxicity, making choices designed to protect your future health and quality of life.
A Realistic Timeline for Common Side Effects
Knowing about acute, delayed, and long-term side effects gives you a bird's-eye view, but when you're in the thick of treatment, you need a more granular map. Understanding the typical timeline for specific symptoms helps you set realistic expectations and see that your experience, while personal, usually follows a predictable pattern. This knowledge empowers you to plan your life, manage your energy, and talk to your oncology team more clearly about what you're feeling and when.
Think of this section as a practical calendar for your treatment journey—one that helps you anticipate the peaks and valleys between each cycle.
Fatigue: The Persistent Companion
Fatigue from chemo isn't just being tired; it's a deep, bone-wearying exhaustion that sleep doesn't always fix. It is, by a huge margin, the most common side effect of chemotherapy. Studies consistently show that between 80-87% of patients report this debilitating symptom during their treatment. One large study found that 80% of patients experienced fatigue, making it their number one complaint.
Unlike some side effects that get better between infusions, this exhaustion can stick around and even build up as treatment goes on, taking a real toll on daily life.
- When It Starts: Fatigue often creeps in within a few hours or days after an infusion.
- When It Peaks: It usually gets worse and hits its peak around 4-7 days post-treatment, which often lines up with when your blood counts are at their lowest.
- How Long It Lasts: This is where it really differs. While you might get a bit of a break before your next cycle, a low-grade fatigue often lingers and can become more intense with each round. After your final treatment, it can take anywhere from 3 to 12 months for your energy to get back to your pre-chemo normal.
Patient Perspective: So many people describe chemo fatigue as feeling like they're trying to walk through wet cement. It’s crucial to remember that this is a physiological response to the treatment—not a personal weakness. Giving yourself grace is the first step in managing it.
Nausea and Vomiting: Intense But Often Short-Lived
The fear of nausea is practically universal among patients starting chemo, but modern medicine has gotten incredibly good at controlling it. Your care team has a whole arsenal of antiemetic (anti-nausea) drugs that can either prevent it entirely or significantly dial it down.
- When It Starts: Nausea can begin within a few hours of your infusion and might hang around for 24 to 72 hours.
- Management Is Key: The timeline for nausea really depends on how well your preventative medications work. Your oncologist will almost always prescribe a combination of drugs—given before, during, and after chemo—to stay ahead of it.
- Post-Treatment: For most people, any significant nausea is gone within a few days of each cycle. It rarely becomes a long-term problem once treatment is complete.
For a deeper dive into handling this specific symptom, take a look at our guide on coping with chemo-related nausea.
This timeline shows how different side effects pop up at different points in your treatment journey.
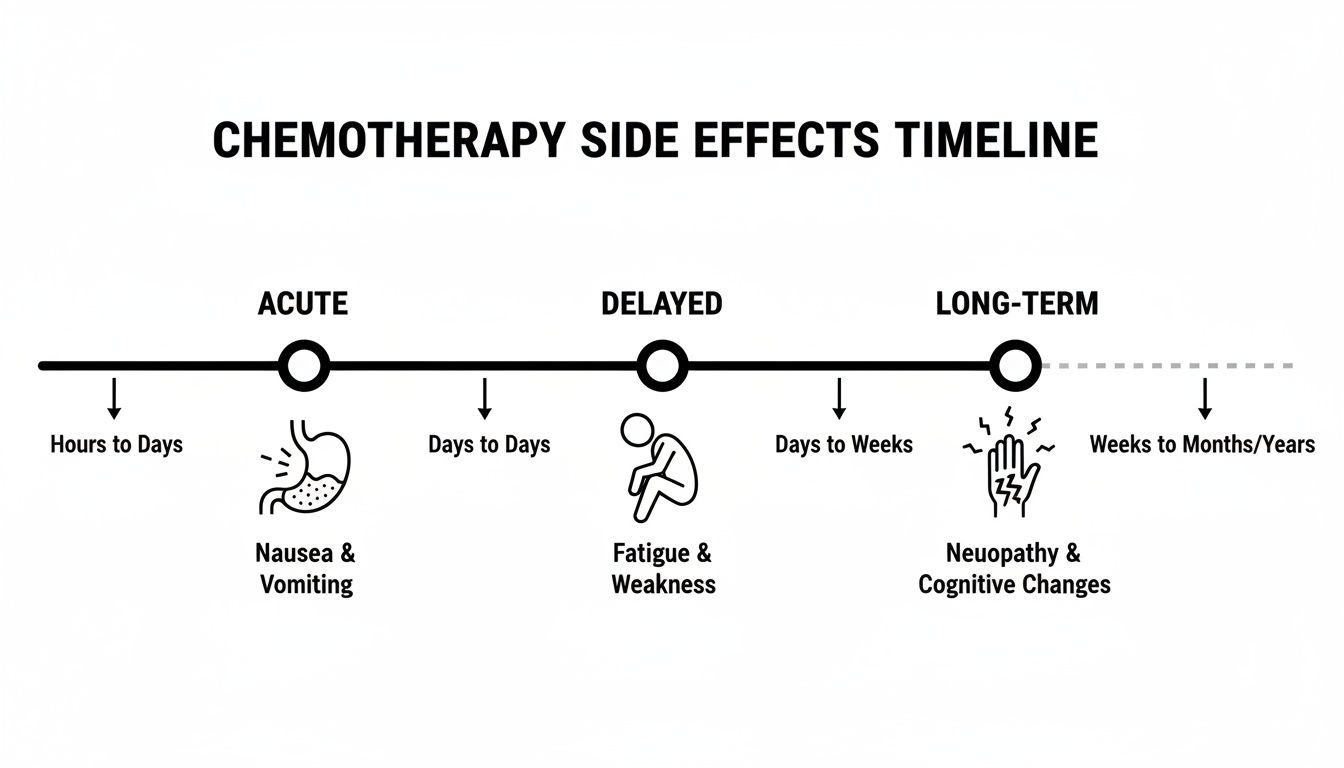
This visual helps clarify the shift from immediate issues like nausea to delayed challenges like fatigue and the potential for lingering effects like neuropathy.
Hair Loss: A Predictable Cycle
Losing your hair (alopecia) is one of the most visible and emotionally tough side effects, but its timing is fairly predictable. It's important to remember that not all chemo drugs cause hair loss, so always ask your doctor if it’s expected with your particular regimen.
- When It Starts: Hair loss usually begins about 2 to 4 weeks after your very first chemotherapy treatment. It might thin out gradually or come out more quickly in clumps.
- The Process: It can affect all body hair, not just the hair on your head. This includes eyebrows, eyelashes, and pubic hair.
- When It Returns: Here’s the good news. Hair typically starts to grow back within 3 to 6 months after your final chemo session. At first, you might notice a soft fuzz that slowly thickens. Don’t be surprised if its texture or color is different from what you had before.
The Dip and Recovery of Your Blood Counts
Chemotherapy goes after rapidly dividing cells, and that includes the cells in your bone marrow that produce blood. This leads to a very predictable cycle where your blood counts drop and then recover between treatments. That lowest point is called the nadir.
- White Blood Cells (Neutrophils): These are your infection-fighting soldiers. They usually hit their nadir 7 to 14 days after a treatment, which is when your risk of infection is highest.
- Platelets: These cells help your blood clot, and they tend to follow a similar timeline as your white blood cells.
- Red Blood Cells: These cells live longer, so anemia (low red blood cells) often develops more gradually over several treatment cycles.
Your care team will be monitoring your blood counts with regular lab tests to make sure they’ve recovered enough before you get your next scheduled treatment.
Chemo Brain and Neuropathy: The Lingering Effects
Some side effects are more subtle and can stick around a lot longer.
Cognitive Fog ("Chemo Brain"): This is a frustrating reality for many. It describes difficulties with short-term memory, finding the right word, or multitasking. It can happen during treatment and, for some, may persist for months or even a few years after treatment is over.
Peripheral Neuropathy: This is nerve damage that causes tingling, numbness, burning, or pain, most often in the hands and feet. It can be cumulative, meaning it gets worse with each dose. While it often improves after treatment stops, recovery can take 6 to 18 months or longer. In some cases, the damage can be permanent. It is absolutely crucial to report these symptoms to your oncologist as soon as you notice them, so they can adjust your treatment to prevent severe, long-term damage.
Key Factors That Influence Your Recovery Timeline
If you've ever wondered why your friend sailed through chemo with mild fatigue while another person struggled significantly, you're not alone. There's a simple reason for this: the timeline for side effects isn't a fixed map. It's a deeply personal journey, and understanding what shapes that path is the first step toward feeling more in control.
Think of it this way—your body is its own unique ecosystem. Chemotherapy introduces a powerful force into that environment, and the resulting impact depends entirely on the nature of that force and the existing health of the ecosystem. Some of these factors are about the treatment itself, while others are all about you.
The single biggest influence is, without a doubt, the specific chemotherapy regimen you're on. Not all chemo drugs are created equal. Just as a sledgehammer and a finishing hammer do very different jobs, different chemo agents attack cancer cells in different ways, leading to vastly different side effect profiles and timelines.
Your Specific Treatment Plan
The "what, how much, and how often" of your therapy are the core building blocks of your experience. A short, single-drug regimen is a world away from a year-long protocol involving multiple potent drugs.
- Type of Chemotherapy Drugs: Some drugs are notorious for causing immediate, intense nausea that fades relatively quickly. Others, like certain taxanes, are linked to neuropathy—numbness and tingling—that can build up over time and linger long after treatment ends.
- Dosage and Intensity: It’s a straightforward equation: higher doses generally lead to more intense and longer-lasting side effects. This is precisely why your oncologist meticulously calculates your dose based on your body size, organ function, and overall health.
- Length and Frequency of Treatment: The longer you're on treatment, the more some side effects can accumulate. Fatigue is a classic example of a cumulative effect—it often gets a little deeper and lasts a little longer with each successive cycle.
This is where a personalized, thoughtful approach makes all the difference. An experienced oncologist doesn't just pick a standard recipe; they select drugs and doses designed to be lethal to your cancer while being as gentle as possible on you. This directly shapes how long your chemo side effects last.
Your Personal Health Profile
Beyond the drugs themselves, your own biology plays a huge role. How well your body processes medications, repairs healthy cells, and manages stress are all critical pieces of the puzzle. Since no two people start from the exact same biological place, no two people will have the exact same recovery.
Key personal factors include:
- Age and Overall Health: A younger person or someone with no other health issues often bounces back faster. Their body's cellular repair crews are simply more robust. On the flip side, pre-existing conditions, especially those affecting the liver or kidneys, can slow the body's ability to clear chemo drugs, extending side effects.
- Genetics: Your unique genetic code can influence how you metabolize certain drugs. This can impact not only how well the treatment works but also how intensely you feel the side effects.
- Lifestyle Factors: Never underestimate the power of nutrition, hydration, and physical activity. A well-nourished body is far better equipped to rebuild healthy tissue and fight off the profound fatigue that chemo can cause.
It's a universal principle that individual factors shape recovery. Exploring articles on understanding healing timelines for physical challenges shows just how much our body's starting point dictates the healing journey, whether from an injury or a medical treatment.
Combination Therapies and Their Impact
Modern cancer treatment is rarely just about chemotherapy anymore. Your treatment plan will likely include other powerful strategies working in tandem, which can create a more complex side effect picture.
When do side effects hit the hardest? The most intense symptoms often appear 3-5 days after an infusion, but many can linger for weeks or months. One study highlighted just how common this is, finding that 86% of patients reported at least one side effect. For 67% of them, it was a battle on multiple fronts—they experienced six or more side effects at the same time, a number that often grew as treatment went on.
When different treatments are combined, their side effects can stack up or even amplify one another. For instance, receiving radiation at the same time as chemo can lead to more severe skin reactions and a deeper level of fatigue than you'd experience with either one alone. Targeted therapies and immunotherapies add their own unique side effects to the mix, too.
The good news is that your oncology team is trained to anticipate these interactions. A huge part of modern cancer care is skillfully layering these treatments to maximize their anti-cancer punch while proactively managing the combined toll on your quality of life.
Navigating Lasting Side Effects for Long-Term Wellness
While most side effects from chemotherapy thankfully fade away, a few can stick around long after treatment is over. These become part of your survivorship story. The idea isn't to cause worry, but to empower you with knowledge. Knowing what to look out for is your best tool for managing your long-term health proactively.

This awareness helps you and your care team get ahead of any potential issues, keeping your quality of life the top priority for years to come. Thinking ahead like this is a cornerstone of good oncology care.
Monitoring for Lasting Changes
Let’s be clear: long-term effects are not a given, but they are a possibility with certain chemotherapy drugs. Your oncology team weighs these risks carefully when designing your treatment plan from the very beginning.
Here are some of the key things we monitor for over the long haul:
- Peripheral Neuropathy: That persistent tingling, numbness, or even pain in your hands and feet can be more than just an annoyance. It can affect your balance and ability to do things like button a shirt.
- Cardiotoxicity: Some drugs can be tough on the heart muscle. That’s why your doctor might recommend heart function tests before you start and periodically afterward to establish a baseline and watch for changes.
- Pulmonary Changes: A small number of chemo agents can cause scarring or changes in lung tissue, so keeping an eye on your respiratory health is important.
- Risk of Secondary Cancers: This is a rare one, but certain chemo drugs can slightly increase the risk of developing a new, different cancer down the road.
It's crucial to remember that while these risks are real, many people—potentially more than half—come through chemotherapy with no lasting problems. The American Cancer Society notes that some complications can last for months, years, or even a lifetime, which really depends on the specific drugs used and your individual health.
The Role of Proactive Survivorship Care
A forward-thinking oncology practice doesn't just treat the cancer; it builds a plan for your long-term wellness right from the start. At Hirschfeld Oncology, this isn't an afterthought—it’s a core part of how we manage care for advanced-stage cancers.
This proactive approach involves a few key strategies:
- Thoughtful Drug Selection: When there are multiple effective options, we lean toward regimens known for having a lower risk of long-term toxicity.
- Protective Measures: In some cases, we can use "shielding" medications to protect vulnerable organs, like the heart or kidneys, from the harshest effects of chemotherapy.
- Smart Dose Adjustments: If we see side effects like neuropathy starting to creep in, we can adjust dosages to help prevent them from becoming permanent.
- Creating a Survivorship Plan: Before your treatment even finishes, we’ll work with you to create a clear roadmap for your future health. This outlines follow-up scans, monitoring for late effects, and provides guidance for your primary care doctor.
The goal of chemotherapy isn't just to treat the cancer in front of you, but to help you live a long, full, and healthy life afterward. A well-designed survivorship plan ensures that any lingering effects are caught early and managed well.
For those dealing with relentless exhaustion that just won't quit, exploring a natural treatment for chronic fatigue syndrome can offer additional coping strategies. In the end, understanding how long chemo side effects last is all about looking at the big picture—from the day of your first infusion to a lifetime of wellness.
How Personalized Oncology Care Can Change Your Timeline
The old way of thinking about chemotherapy—a rigid, one-size-fits-all protocol—is quickly becoming a thing of the past, especially for complex, advanced-stage cancers. When we start building a treatment plan around the person instead of just the diagnosis, the entire conversation about "how long chemo side effects last" changes.
This modern, patient-first philosophy is all about seeing you as a unique individual, not just a statistic on a chart. We move beyond the standard playbook, using sophisticated strategies designed to attack the cancer aggressively while sparing your body as much as possible. This is where the art and science of oncology truly come together.
Shifting from Standard Protocols to Individualized Regimens
The goal is simple but powerful: get the best possible results with the least amount of toxicity. This isn't just about handing out anti-nausea pills after the fact; it's about thoughtfully designing a regimen that is less likely to cause severe problems from the start.
We accomplish this through a few key approaches:
- Low-Dose Chemotherapy: Sometimes, less is more. Administering lower doses more frequently can be just as lethal to cancer cells but gives your healthy cells a much-needed break. This can significantly lessen the blow of side effects like debilitating fatigue and persistent nausea.
- Targeted Therapies: Think of these as smart drugs. They're engineered to seek out and attack specific weaknesses unique to the cancer cells, leaving most of your healthy tissues unharmed. This precision leads to a completely different—and often far more manageable—set of side effects.
- Carefully Managed Schedules: A treatment plan shouldn't be set in stone. We constantly monitor how your body is responding and aren't afraid to adjust the timing, dosage, or combination of drugs. This flexibility is crucial for keeping you strong and feeling as good as you can.
This meticulous, hands-on approach is the cornerstone of our practice at Hirschfeld Oncology. The result for our patients is often a shorter, less intense battle with side effects, which dramatically improves their quality of life during a difficult time. You can learn more about how we build these custom strategies in our guide to personalized oncology care.
True patient-centered care means that your tolerance and quality of life are considered just as important as the treatment's effectiveness. The two are not mutually exclusive; they work together.
This proactive, collaborative process puts you and your well-being at the heart of every decision. For patients in the New York City area who are navigating an advanced-stage cancer diagnosis, this path offers a more tolerable and hopeful way forward. Exploring a consultation can help you understand all the options on the table.
Frequently Asked Questions About Chemo Side Effects
Going through chemotherapy brings up a lot of questions, and that’s completely normal. Even after you’ve discussed the big picture with your doctor, the day-to-day uncertainties can be the most daunting. Let's walk through some of the most common questions I hear from patients about what it really feels like between cycles.
Getting answers to these practical concerns helps peel back the mystery of treatment. It turns fear of the unknown into knowledge you can use, helping you feel more in control of your own care.
Will I Feel Sick the Entire Time Between Chemo Cycles?
This is probably the number one fear people have, but thankfully, the answer is almost always no. For most people, there’s a predictable rhythm to it: a few tough days followed by a gradual recovery. The first few days right after your infusion are usually the most challenging. That's when the immediate side effects, like nausea and that first wave of fatigue, tend to hit hardest.
But after that initial hump, you should start feeling a little better each day. The whole point of the supportive medications and care we provide is to soften the blow of those tough days and give you as many "good days" as possible before your next treatment. A great tip is to track your symptoms on a calendar. It helps both you and your oncology team see the pattern and get ahead of it.
Can Diet and Lifestyle Choices Shorten Side Effects?
They absolutely play a huge supportive role. While a healthy diet or a walk around the block can't magically erase side effects, their impact on your resilience is undeniable. Think of it as giving your body the best possible tools for the job. Staying hydrated is non-negotiable—it helps flush the chemo drugs through your system. Eating nutritious, protein-rich foods gives your body the raw materials it needs to repair healthy cells that get caught in the crossfire.
And as for exercise, gentle movement can be your best friend. A short, slow walk can do more for chemo-related fatigue than just about anything else. It also helps with your mood and prevents muscle loss. Just be sure to run any new diet or exercise plans by your oncologist first to make sure they're right for you.
Remember, the goal isn't to run a marathon. It's simply to listen to your body and give it the fuel, hydration, and gentle movement it needs to bounce back as best it can.
When Should I Call My Doctor About a Side Effect?
First, let me be clear: we want you to call. Never feel like you're bothering your care team if you're worried about something. That said, some symptoms are red flags that need immediate attention. Your nurse will give you a very clear list of what to watch for before you even start.
As a general rule, you need to call your doctor’s office right away for any of these:
- A high fever. This can signal a serious infection, especially when your white blood cell counts are low.
- Nausea or vomiting you can't control. If you can't even keep water down, we need to know.
- Signs of an allergic reaction, like a rash, hives, swelling of the face or throat, or trouble breathing.
- Any new or severe pain that isn't touched by your prescribed medications.
When in doubt, make the call. It’s always better to get it checked out and be told it's nothing than to wait and let a small problem turn into a big one.
Do Side Effects Get Worse with Each Chemo Cycle?
It depends on the side effect. Some can build up over time, what we call a cumulative effect. Your body has a little less time to fully recover between each round, so certain issues can stack up.
Fatigue is the classic example; it often gets a bit deeper with each cycle. The same goes for peripheral neuropathy—that tingling or numbness in your hands and feet. The more exposure the nerves get to the drug, the more pronounced it can become. On the other hand, some side effects, like nausea, might actually get better. As we see how you react, your team can get much better at fine-tuning your anti-sickness medications. This is exactly why keeping that line of communication open with us is so important.
At Hirschfeld Oncology, we believe managing your side effects is just as important as fighting the cancer. By creating individualized, lower-toxicity treatment plans and staying in close communication, we work to make your journey more tolerable. To learn how our patient-centered approach can make a difference in your quality of life, we invite you to explore our blog. Find more information at https://honcology.com/blog.





.png)


.png)
.png)




