When you hear the term adjuvant chemotherapy, think of it as a "mop-up" crew that comes in after the main event. The primary treatment, usually surgery, has already removed all the cancer that we can see. Adjuvant chemotherapy is the critical follow-up step designed to hunt down any microscopic cancer cells left behind.
Think of it as an insurance policy against the cancer ever coming back.
What Is Adjuvant Chemotherapy and Why Is It Used?
Let's use an analogy. Imagine you've just finished weeding a garden. You’ve pulled out every single weed you can spot, and the garden bed looks completely clean. But what about the tiny, invisible seeds that might still be hiding in the soil, just waiting for a chance to sprout?
Adjuvant chemotherapy is like a special treatment for that soil. Its job is to find and neutralize those hidden seeds before they ever get a chance to grow.

This proactive strategy is incredibly important. Even after a surgeon successfully removes a tumor, tiny clusters of cancer cells, called micrometastases, can remain. These cells are far too small to show up on any scan or be found during a physical exam, but they pose a serious risk for the cancer returning down the road.
To help you quickly grasp the key points, here’s a simple breakdown:
Adjuvant Chemotherapy At a Glance
This table shows how adjuvant therapy is a defensive, preventative measure. It’s all about protecting your future health.
The Goal: Safety Through Prevention
The main objective here isn't to shrink visible tumors—those have already been dealt with. The entire focus of adjuvant chemotherapy is to lower the odds of the cancer returning.
By targeting those lingering, invisible cells, it acts as a powerful preventative measure. This approach is a standard, and often life-saving, part of the treatment plan for many common cancers, including:
- Breast cancer
- Colorectal cancer
- Pancreatic cancer
- Lung cancer
This treatment is fundamentally about playing defense. After the primary offense (surgery) has cleared the field, adjuvant therapy ensures no surprise players are left hiding on the sidelines, ready to re-emerge.
It’s a strategic decision made when a patient is technically "cancer-free," but the statistical risk of recurrence is high enough to justify taking this extra step.
This is different from other chemotherapy timings. For treatments given before surgery to shrink a tumor, you can learn more about what neoadjuvant chemotherapy is in our other guide. Understanding the "why" behind adjuvant chemotherapy helps clarify its vital role in a comprehensive care plan aimed at securing long-term health and giving you peace of mind.
How Doctors Decide If You Need Adjuvant Chemotherapy
It can feel strange, even confusing, to talk about chemotherapy when your surgeon has just told you they "got all the cancer." But after surgery, the big question is no longer about the tumor we can see, but about any microscopic cancer cells that might have escaped before the operation.
Think of these as "sleeper cells." They're invisible to scans and don't cause any symptoms, but they have the potential to grow into a new tumor months or even years down the road. The decision to recommend adjuvant chemotherapy is all about figuring out the odds of these cells being there and whether a course of treatment is worth it to wipe them out. It’s a careful, calculated risk assessment—never a guess.
Analyzing the Clues a Tumor Leaves Behind
To get a clear picture of your personal risk, your oncologist acts like a detective. They'll closely examine the pathology report from your surgery, which is filled with critical clues about the tumor's personality and behavior.
Here’s what they’re looking for:
- Cancer Stage: This is the big one. It tells us the size of the original tumor and, most importantly, whether it had spread to any nearby lymph nodes. If cancer cells reached the lymph nodes, it's a strong sign they were trying to travel, which automatically raises the risk of recurrence.
- Tumor Grade: Under a microscope, some cancer cells look a lot like normal cells, while others look chaotic and disorganized. A high-grade tumor is one that looks very abnormal, which tells us it's more aggressive and likely to grow back quickly.
- Lymphovascular Invasion: The pathologist will also check if any cancer cells have invaded the tiny blood vessels or lymph channels in and around the tumor. Seeing this is like catching the cancer cells red-handed as they were trying to get into the body's transportation systems.
These aren't just data points; they're puzzle pieces that help us build a profile of your specific cancer and estimate the likelihood that it could come back.
Weighing the Benefits Against the Risks
Once your oncologist has all this information, they can start to balance the equation. Is the risk of the cancer returning high enough to justify going through the side effects of chemotherapy?
If the clues point to a high risk of recurrence, adjuvant chemotherapy can be a powerful tool to protect your future health and give you the best shot at long-term, cancer-free survival. But if the risk is very low, the treatment might be more than you actually need.
This is always a conversation and a shared decision, not a command. We talk it through together. The proven success of this preventative approach is why we see its use growing worldwide. The demand for first-line chemotherapy, which includes adjuvant treatments, is projected to jump by 53% between 2018 and 2040, from 9.8 million people to 15 million annually. You can read more about the projected rise in chemotherapy demand at AJMC.com. This is largely because it's been so effective at preventing relapse in common cancers like breast and colorectal cancer.
Ultimately, the conversation is about statistics and personal goals. Adjuvant chemotherapy is a strategic move to stack the odds in your favor, giving you the best possible chance for a future free from cancer.
Our goal is to make sure you only go through more treatment if it offers a real, meaningful benefit, protecting your long-term health while respecting your quality of life right now.
Understanding Different Types of Chemotherapy
When you're facing a cancer diagnosis, the terminology alone can be overwhelming. You might hear words like adjuvant, neoadjuvant, and palliative chemotherapy, and it can feel like trying to learn a new language. But these terms aren't just medical jargon; they describe specific, strategic ways we use chemotherapy, and understanding them is the first step toward feeling in control of your treatment journey.
Think of adjuvant chemotherapy like a finishing coat of paint after building a house. The main structure—the tumor—has been removed by surgery, and everything looks good. But we add that extra layer of protection to make sure any tiny, unseen imperfections are sealed away, preventing future problems down the road. It's a proactive step taken after the primary treatment to give you the best possible long-term outcome.
The Three Main Timings For Chemotherapy
To really get a handle on your treatment plan, it helps to understand when each type of chemotherapy is used. The timing is everything, as it's directly tied to the specific goal we're trying to achieve.
- Adjuvant Chemotherapy (After Surgery): The main goal here is to hunt down and eliminate any microscopic cancer cells, known as micrometastases, that might still be lingering after surgery. It’s a clean-up mission designed to significantly lower the chances of the cancer ever coming back.
- Neoadjuvant Chemotherapy (Before Surgery): This approach is used to shrink a tumor before the surgeon operates. Making the tumor smaller can lead to a less invasive surgery, make the operation itself more successful, and in some cases, can even change the type of surgery you need.
- Palliative Chemoterapia (For Advanced Cancer): When cancer has spread and a cure isn't the primary objective, chemotherapy can still be a powerful tool. Palliative chemo is focused on managing symptoms, slowing the cancer's growth, and ultimately, improving your quality of life.
The decision to use one approach over another isn’t arbitrary. It’s based on a careful analysis of your specific cancer—its stage, grade, location, and unique characteristics. Your oncology team pieces together all this information to build your personalized plan.
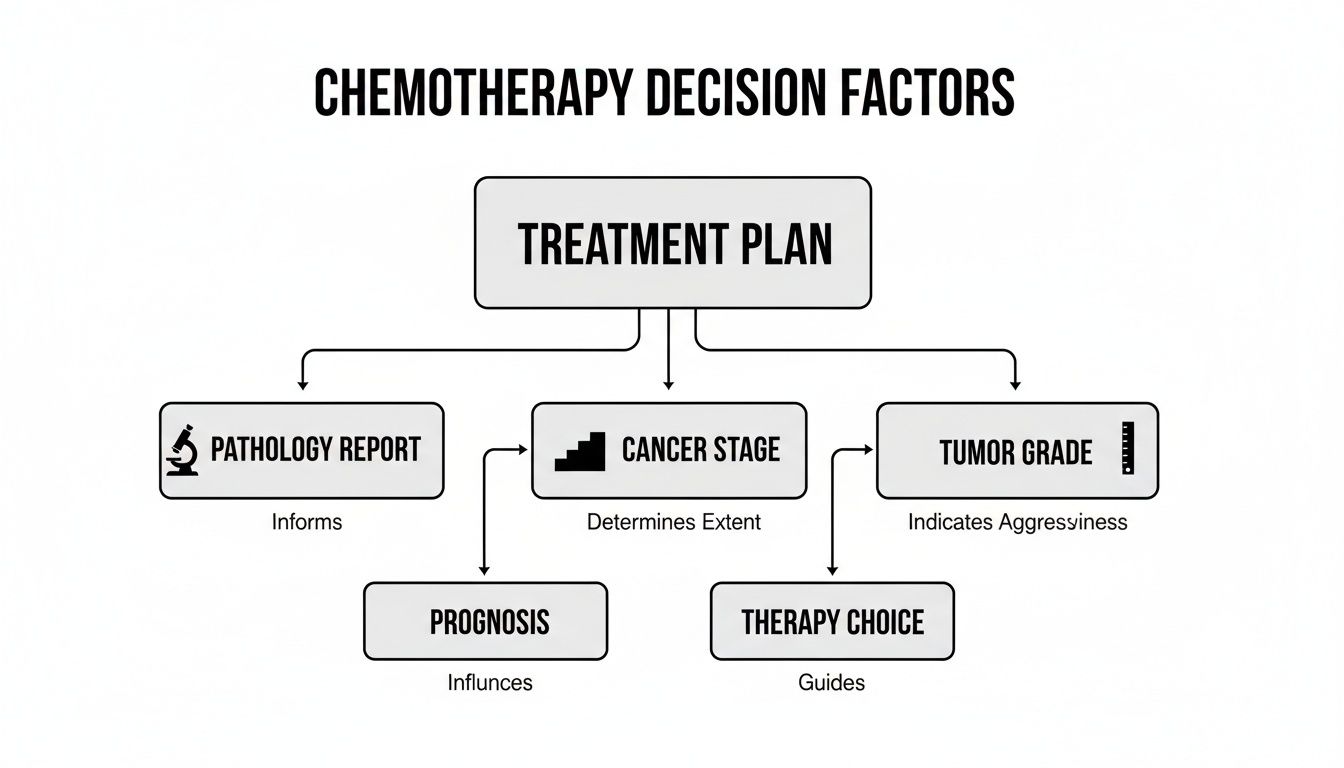
As this flowchart shows, every decision branches out from the foundational details found in your pathology report. The cancer's stage and tumor grade are critical clues that guide us toward the most effective therapy for you.
A Side-by-Side Comparison
Sometimes, the easiest way to understand different concepts is to see them laid out side-by-side. The table below breaks down the key differences between these chemotherapy strategies. To get a better sense of the underlying science, you can also explore our guide explaining how chemotherapy works to attack cancer cells.
Comparing Chemotherapy Types: Adjuvant, Neoadjuvant, and Palliative
Seeing them all together makes it clear that the timing of chemotherapy isn't random. It’s a highly strategic decision designed to give you the maximum benefit at each stage of your treatment.
The timing of chemotherapy is not random; it's a highly strategic decision. Each approach is deployed at the moment it can have the greatest impact on your outcome, whether that's preventing recurrence, enabling a better surgery, or providing comfort.
Personalizing Treatment with Modern Oncology
Cancer care has come a long way from the "one-size-fits-all" model of the past. We've learned that not all cancers are created equal, even if they start in the same part of the body. Today, our focus is on understanding the unique biological signature of your tumor, allowing us to build a much more personalized and effective treatment strategy.
Think of it this way: imagine two people diagnosed with the same type of early-stage breast cancer. A few decades ago, they would have likely received the exact same adjuvant chemotherapy plan after their surgery. Now, we know their tumors could be worlds apart on a molecular level. One might be highly aggressive and prone to coming back, while the other is slow-growing and poses a much lower risk. Giving both the same treatment just doesn't make sense anymore.

Using Genomics to Predict Chemotherapy Benefit
This is where advanced genomic testing has completely changed the game. These incredible tools analyze a small piece of the tumor tissue removed during surgery, looking at the activity of specific genes that control cancer growth. The results give us a "recurrence score"—a number that helps predict the likelihood of the cancer returning and, most importantly, whether adjuvant chemotherapy will meaningfully reduce that risk.
This data-driven approach helps us answer the single most important question you might have: "Will the benefits of chemotherapy outweigh the side effects for me?" It transforms a potentially overwhelming decision into an informed, collaborative conversation between you and your oncology team.
Breast cancer treatment is a fantastic real-world example of this progress. The Oncotype DX Breast Recurrence Score test has been a game-changer for over two decades. It's the only test proven to predict chemotherapy benefit for the 2 million-plus patients worldwide with early-stage, HR+, HER2-negative breast cancer. The results are astounding: an estimated 1.6 million of these patients—a full 80% of those tested—have been able to safely skip chemotherapy, avoiding its harsh side effects without impacting their long-term outcomes. You can learn more about how this genomic test has reshaped breast cancer care worldwide.
This approach is about treating the person, not just the disease. By understanding the specific biology of your tumor, we can make smarter, more targeted decisions that prioritize both your long-term health and your immediate quality of life.
The Shift Toward Precision Medicine
This move toward precision represents a fundamental shift in how we practice oncology. It’s about being smarter with our tools and reserving powerful treatments like chemotherapy for the people we know will truly benefit from them.
This personalized approach delivers several clear advantages:
- Avoiding Overtreatment: If you have a low-risk tumor, you can confidently and safely skip chemotherapy and all its associated side effects.
- Confirming Treatment Need: For those with high-risk scores, the test provides clear, objective evidence that chemotherapy is a crucial step to protect your future health.
- Empowering Patients: It gives you concrete data to understand your situation, helping you feel more confident and in control of your treatment plan.
By weaving these advanced diagnostics into our process, we can design an adjuvant therapy plan that is truly tailored to you. Every step we take is grounded in solid evidence, giving you the best possible chance for a healthy, cancer-free future while minimizing any unnecessary hardship along the way.
Managing Side Effects and Prioritizing Your Wellbeing
Starting adjuvant chemotherapy is a powerful, proactive step toward a cancer-free future. It's also completely normal to wonder how you'll feel during treatment and how you'll manage potential side effects. The good news is that your oncology team is just as focused on your comfort and wellbeing as they are on fighting the cancer.

Think of side effect management not as an afterthought, but as a central part of your treatment plan. It’s a true partnership, and your quality of life is always the top priority.
Common Side Effects and How We Get Ahead of Them
Everyone's body reacts differently to chemotherapy, but there are some common side effects we can anticipate and manage from day one. Staying ahead of them with medication, simple lifestyle adjustments, and open communication is the name of the game.
Here are a few things people often experience:
- Fatigue: This is more than just feeling tired; it can be deep and persistent. We've found that gentle movement, like a daily walk, balanced with good nutrition and prioritizing rest can make a world of difference.
- Nausea and Vomiting: Today's anti-nausea medications are incredibly effective. The key is to take them on schedule, even if you feel fine. This prevents nausea before it ever starts.
- Hair Loss: Not every chemo drug causes hair loss. We’ll talk specifically about what to expect with your regimen and can explore options like scalp cooling systems that can help reduce it.
Your wellbeing is the foundation of successful treatment. By actively managing side effects, you empower your body to handle therapy more effectively and maintain your quality of life.
This focus on patient comfort is a huge area of medical innovation. In fact, the global market for oncology adjuvants—therapies designed to make chemo more tolerable and effective—is expected to hit USD 1.03 billion by 2035. It shows just how committed the medical community is to finding better ways to support patients through treatment.
Staying In Control of Your Comfort
Knowledge is power. Knowing what to expect and having practical tips in your back pocket can make a huge difference in how you feel day-to-day. For a more detailed guide, check out our post on managing side effects of cancer treatment for a better quality of life.
It can also be helpful to be aware of how your environment affects you during this time. Understanding the symptoms of chemical sensitivity can help you create a more comfortable home space by minimizing potential irritants.
Above all, remember that your voice is the most important tool we have. When you tell us exactly how you're feeling, we can fine-tune your supportive care plan. This open dialogue ensures we can help you navigate this phase of your journey with strength and resilience.
Answering Your Questions About Adjuvant Chemotherapy
It's completely normal to have a lot of practical questions when you're facing a cancer treatment plan. Getting clear, direct answers can make a world of difference, helping you feel more prepared and in control. Let's walk through some of the most common concerns we hear from patients and their families about adjuvant chemotherapy.
How Long Does Adjuvant Chemotherapy Last?
There’s no single answer to this one—the timeline is carefully mapped out based on your specific cancer, the drug regimen we choose, and your overall health.
Generally, you can expect a treatment course to last somewhere between three to six months. For instance, a standard plan for colon cancer often runs for six months, whereas some breast cancer treatments might be wrapped up in three or four months.
Your oncologist will lay out a precise schedule for you. This plan details the number of "cycles" you'll have and how often you'll come in for treatment—maybe every two or three weeks. We design these schedules to hit the cancer cells hard while still giving your body the time it needs to recover between rounds.
Will I Definitely Lose My Hair?
Hair loss is probably the most famous side effect of chemo, but here’s the important part: it doesn't happen with every chemotherapy drug. Whether you experience some thinning or complete hair loss depends entirely on the specific medicines in your treatment plan.
Some drugs are very likely to cause it, while others rarely do. Before you even start, your oncology team will sit down with you and be upfront about what you can expect from your specific regimen. We can also talk through options like scalp cooling systems (often called "cold caps"), which can help some people reduce hair loss by limiting blood flow to the hair follicles during infusion.
Remember, everyone’s experience is different. The more you share your concerns—about hair loss or anything else—the better we can tailor our support and management strategies for you right from the start.
This open conversation is key to making sure you feel ready for what's ahead.
Can I Still Work and Live My Normal Life?
Many people successfully continue working and keep up with their daily routines during treatment, though it often requires a few adjustments. Your ability to do so will really depend on a few things:
- Your specific regimen: Some chemo plans are more intense and have stronger side effects than others.
- Your job's demands: A desk job is often easier to manage than one that requires heavy physical labor.
- How you feel: Simply put, every person’s body reacts to treatment in its own way.
Some patients find it helpful to tweak their work schedules. This might mean working from home more often or cutting back on hours, especially in the few days right after a treatment when fatigue can really kick in. Keeping your employer in the loop can make navigating this much easier. Our goal is always to help you maintain as much of your normal life and well-being as possible.
What Happens After My Last Treatment?
Finishing your final round of adjuvant chemotherapy is a huge milestone. It’s a moment to celebrate. From there, you’ll shift into a new phase of care called surveillance or monitoring.
This next chapter involves regular follow-up appointments with your oncologist. These check-ins are essential for keeping an eye on your long-term health. They usually involve a mix of physical exams, blood work, and imaging scans (like CT or PET scans) at set intervals.
This follow-up plan has two main goals:
- To watch for any signs of cancer recurrence, so we can catch it at the earliest possible stage.
- To help you manage any lingering side effects from your treatment.
This marks the start of a long-term partnership with your care team. We'll give you a personalized survivorship care plan that acts as a roadmap for your future health, outlining your treatment history and a clear schedule for future check-ups to ensure you always have our full support.
At Hirschfeld Oncology, we're here to guide you through every question with clarity and compassion. We focus on creating personalized treatment plans that prioritize not just your long-term outcome, but your quality of life right now. Request a consultation today to learn more about our approach.





.png)


.png)
.png)




