When you first hear the term "neoadjuvant chemotherapy," it might sound complicated, but the core idea is actually quite simple and strategic. It’s a course of chemotherapy given before the primary treatment, which is usually surgery.
Think of it as preparing a difficult worksite before starting the main construction project. You’d first clear the area and make the job safer and more manageable. Neoadjuvant chemotherapy does the same thing for your surgeon, aiming to shrink a tumor to make the operation less invasive and more likely to succeed. It's a proactive first step toward a better long-term outcome.
What is Neoadjuvant Chemotherapy?
Instead of jumping straight to surgery to remove a large or tricky tumor, your oncology team might decide that using powerful cancer-fighting drugs first is the smartest play. This isn't a sign that things are worse; in fact, it's a carefully planned strategy to stack the odds in your favor.
By administering chemotherapy upfront, we get to see how the cancer responds to the medication and can potentially downsize the tumor, setting the stage for a more effective and less extensive surgery.
The Primary Goals of This Approach
The decision to use chemotherapy before surgery isn't made lightly. It’s based on a few key objectives, all aimed at improving your overall treatment and giving us valuable information for your ongoing care.
- Shrinking the Tumor: The most immediate goal is to reduce the tumor's size. For someone with breast cancer, for example, this could mean the difference between needing a full mastectomy and being a candidate for a less invasive lumpectomy. A smaller tumor is simply easier for a surgeon to remove completely.
- Targeting Hidden Cancer Cells: Cancers can shed microscopic cells, called micrometastases, that travel to nearby lymph nodes or into the bloodstream. Neoadjuvant therapy attacks these rogue cells early on, long before they have a chance to settle and grow elsewhere, which lowers the risk of the cancer coming back later.
- Testing Treatment Effectiveness: This is a huge benefit. Giving chemo first is like a real-time test run. We can directly observe how well the tumor responds to the drugs. If it shrinks significantly, we know we've chosen a highly effective treatment for your specific cancer.
This early feedback gives us crucial insights into the tumor’s unique biology. It allows your care team to confirm we’re on the right track and using the most powerful medications for your fight.
To give this concept more context, it's helpful to have a general understanding of chemotherapy and how these powerful drugs work. Grasping the basics makes it easier to see why the timing—giving it before surgery—can make such a profound difference.
Here’s a quick overview of the key points.
Neoadjuvant Chemotherapy at a Glance
Ultimately, this approach is all about making the entire treatment process more effective from start to finish.
Neoadjuvant vs. Adjuvant Therapy: Understanding the Timing
To really wrap your head around neoadjuvant chemotherapy, it helps to see how it fits into the bigger picture of a cancer treatment plan. In oncology, timing isn’t just about scheduling appointments—it’s a fundamental part of the strategy. The main difference between neoadjuvant therapy and its counterpart, adjuvant therapy, comes down to one simple thing: when it's given.
Think of it like a strategic mission against a tumor. Neoadjuvant chemotherapy is the first wave of attack, sent in before the main event—which is usually surgery. The goal here is to shrink the tumor, making it easier and safer for the surgeon to remove completely. It’s a preemptive strike designed to set the stage for a more successful operation.
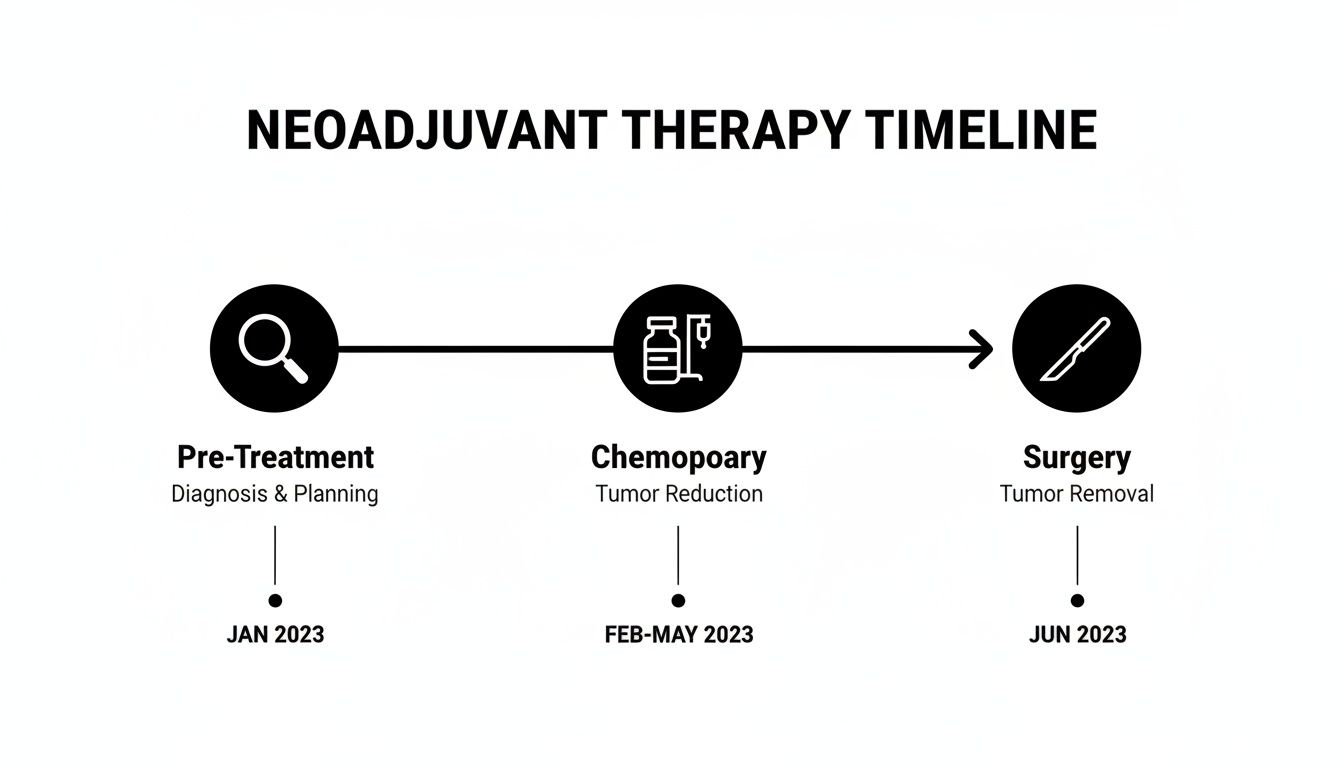
This visual shows that initial planning is followed by chemotherapy aimed at reducing the tumor, which then leads to the surgical procedure.
Adjuvant Therapy: The Follow-Up Mission
On the other hand, adjuvant therapy comes in after surgery. Once the surgeon has removed all visible signs of the tumor, the job of adjuvant chemo is to act as a "mop-up" crew. It seeks out and destroys any microscopic cancer cells that might have been left behind or have strayed to other parts of the body. The whole point is to reduce the risk of the cancer ever coming back.
While both approaches often use the same powerful drugs, their roles are completely different. One clears the path for surgery, while the other secures the area afterward. It's not uncommon for an oncologist to use both, creating a powerful one-two punch that attacks the cancer before and after the surgical procedure. To learn more about how different treatments work together, check out our article on the relationship between chemo and radiation therapy.
It's also critical to distinguish these approaches from palliative therapy. Both neoadjuvant and adjuvant treatments are given with the goal of a cure. Palliative therapy, however, is used when a cure isn't possible. Its focus shifts to managing symptoms, slowing the cancer's progression, and ensuring the best possible quality of life for the patient.
Comparing Chemotherapy Approaches
To put it all into perspective, let's break down the timing and goals of these different treatment strategies.
Understanding which approach your care team is recommending gives you a much clearer picture of your treatment journey. It helps you know exactly what each step is designed to accomplish.
Which Cancers Respond Best to This Approach?
While the idea behind neoadjuvant chemotherapy is pretty flexible, its actual use is highly specific. This strategic, pre-surgical treatment is most effective for certain solid tumors—specifically, those that are either large or have spread to nearby lymph nodes but haven't yet traveled to distant parts of the body.
Think of it as a specialized tool that’s perfect for a particular job. It’s become a go-to strategy for what we call "locally advanced" cancers, where the goal is to make a tough surgical situation much more manageable before the surgeon even picks up a scalpel.
Cancers Where This Strategy Shines
The decision to recommend neoadjuvant chemotherapy always comes down to the tumor's size, location, and its unique biological fingerprint. For some cancers, this upfront treatment isn't just an option; it's become the standard of care because it’s been proven time and again to improve outcomes.
Breast Cancer: This is probably the most well-known use case. For someone with a large or aggressive tumor, neoadjuvant therapy can shrink it enough to make a lumpectomy (which saves the breast) a real possibility instead of a full mastectomy. This can make a world of difference for a patient's quality of life and body image.
Lung Cancer: In certain types of non-small cell lung cancer (NSCLC), tumors can be tricky to remove simply because of their size or how close they are to vital organs. Giving chemotherapy—often now paired with immunotherapy—before surgery can "downstage" the tumor, making a complete and successful removal much more likely.
Colorectal Cancer: This is especially crucial in rectal cancer. Because the pelvis is such a tight space, shrinking a tumor with neoadjuvant therapy (usually with radiation, too) makes the surgeon's job much easier. More importantly, it dramatically increases the odds of preserving sphincter function, which helps patients avoid a permanent colostomy bag.
Pancreatic and Esophageal Cancers: These cancers are notoriously difficult to treat surgically from the get-go. Neoadjuvant therapy can be a true game-changer here. It can potentially turn a tumor once considered inoperable into one that can be safely removed, giving patients a shot at a cure that might not have been on the table otherwise.
The Power of a Pathological Complete Response
One of the best-case scenarios we hope for is achieving what’s called a pathological complete response (pCR). This means that when the surgeon removes the tissue, the pathologist finds zero active cancer cells under the microscope. The treatment wiped them all out.
Being able to see this happen before surgery gives us incredibly valuable information about a patient’s long-term outlook.
For instance, the difference in breast cancer outcomes is striking. One major study revealed that patients who achieved pCR after neoadjuvant therapy had a 41% lower risk of dying from breast cancer compared to those who only received chemotherapy after surgery. You can read more about these findings on breast cancer treatment outcomes.
This really shows how this "treatment first" approach can set the stage for long-term success, turning a difficult diagnosis into a more hopeful and manageable journey.
The Benefits and Potential Risks You Should Know
Like any major medical decision, choosing a treatment plan means carefully weighing the potential upsides against the real-world challenges. When it comes to neoadjuvant chemotherapy, understanding both sides of the coin helps you and your oncology team decide if this "surgery-first" strategy is the right move for you.

Key Advantages of Pre-Surgical Treatment
Giving chemotherapy before surgery is a proactive approach with some powerful benefits. The biggest goal, and often the most impactful one, is to shrink the tumor, which can dramatically change the surgical plan for the better.
Paving the Way for Less Invasive Surgery: A smaller, more manageable tumor is simpler for a surgeon to remove completely. For a breast cancer patient, this could be the difference between needing a full mastectomy and being a candidate for a less extensive lumpectomy.
Getting an Early Look at How Well Treatment Works: This approach acts as a real-time test. We can see how your specific cancer responds to the chosen drugs. If the tumor shrinks dramatically, it’s a great sign that we've found a highly effective weapon for any treatment needed down the road.
Attacking Hidden Cancer Cells Sooner: Cancers can shed microscopic cells that travel through the body but are too tiny to show up on scans. Neoadjuvant therapy gets to work on these micrometastases right away, lowering the risk of the cancer coming back later on.
Acknowledging the Potential Risks
While the benefits are compelling, it’s crucial to have an honest conversation about the potential downsides. Your care team will be watching you like a hawk to manage these risks and keep you on track for surgery.
Every treatment plan is a balance. The goal is to maximize the powerful benefits of neoadjuvant chemotherapy while actively managing side effects and ensuring you remain strong enough for your eventual surgery.
The primary concerns are the side effects that come with chemotherapy, like fatigue and nausea. If these become too severe, they could potentially push back your surgery date. There's also a small chance the tumor won't shrink as much as we hope. This is why close monitoring with regular imaging is so important—it lets your oncologist see what's happening and adjust the plan if needed.
The good news is that the field is constantly improving. For instance, in non-small cell lung cancer, adding immunotherapy to neoadjuvant chemo is producing incredible long-term results. One landmark trial showed this combination cut the risk of the disease returning or death by 32% compared to chemo alone. This highlights not just how effective these treatments can be, but also that their side effects are manageable for most patients. You can read more about these exciting lung cancer trial results.
What to Expect During Your Treatment Journey
Hearing you need chemotherapy before surgery can be a lot to take in. It's natural to feel a bit overwhelmed. Knowing what the process looks like, step by step, can help make everything feel more manageable and put you back in the driver's seat.
Think of this as a team effort. You’ll have a dedicated group of specialists—oncologists, surgeons, radiologists, and nurses—all working together to design a plan that’s built just for you.

It all starts with a detailed consultation. Your care team will walk you through the entire plan: which drugs they recommend, why they chose them, and what the schedule for your infusion sessions will look like. But this plan isn't set in stone. It's designed to be flexible, and you are always an active partner in your own care.
Monitoring Your Progress
One of the most important parts of neoadjuvant therapy is keeping a close eye on how the tumor is responding. This is how we know the treatment is doing its job. It’s like getting real-time updates from the front lines, allowing your care team to make the smartest decisions for your health.
Here's how we typically track your progress:
- Imaging Scans: You'll have regular CT, MRI, or PET scans. These pictures give us a clear view of the tumor, letting us measure any changes in its size and activity.
- Blood Tests: We use routine blood work to keep an eye on tumor markers and your overall health, making sure your body is handling the treatment well.
- Physical Exams: Your oncologist will perform regular physical check-ups to see how you're feeling and help manage any side effects that pop up.
This close monitoring is one of the biggest benefits of neoadjuvant chemotherapy. Take locally advanced colorectal cancer, for example. Giving chemo before surgery has been shown to dramatically improve outcomes. One major study found it lowered the risk of death by 33% compared to doing surgery first. You can read more about these findings on colorectal cancer survival rates.
Your treatment plan is adaptable. If a tumor isn't shrinking as much as we’d like, your team can switch up the drug combination or adjust the timing. The goal is to make sure you're always getting the most effective care possible.
By explaining what to expect and showing you how we track your progress, we hope to ease your anxiety and help you feel confident in your treatment. For a closer look at the infusion process itself, our guide on what to expect during chemotherapy is a great resource.
How Hirschfeld Oncology Personalizes Your Care
It’s one thing to understand the concept of neoadjuvant chemotherapy, but it's another thing entirely to see how that strategy can be shaped to fit you. At Hirschfeld Oncology, this is where we thrive. We specialize in the very cancers where this upfront approach can be life-changing—pancreatic, breast, and colorectal cancers, among others.
Our entire philosophy centers on you, the patient, not just the disease. We don't believe in one-size-fits-all protocols. Instead, we build a treatment plan from the ground up, designed around your specific tumor biology, your overall health, and what matters most to you. This often means thoughtfully combining neoadjuvant chemotherapy with other innovative treatments to give you the best possible shot at a good outcome.
A Focus on Innovation and Quality of Life
Dr. Azriel Hirschfeld is driven by a commitment to finding powerful options that don't force you to sacrifice your quality of life. The goal is to get you to surgery stronger, not weaker.
- Low-Dose Chemotherapy: We frequently use precisely calculated, lower doses of chemotherapy. This approach is gentler on the body, helping you maintain your strength and well-being, but is still tough on the cancer.
- Targeted Therapies: When we find specific genetic drivers in your tumor, we can use drugs that zero in on those cancer cells, leaving your healthy cells alone. It's a much smarter, more focused way to fight.
- Genomic Testing: We don't guess; we test. We use advanced diagnostics to understand your cancer at a molecular level. You can learn more about the role of genomic testing in developing personalized treatment plans and how it helps us choose the right drugs for you from the very beginning.
Our goal is simple: to offer sophisticated, compassionate care that provides hope and preserves the quality of your life. We are here to find a path forward, especially for patients who have been told their options are limited.
If you or someone you care about is facing a tough diagnosis and exploring neoadjuvant chemotherapy, we encourage you to request a consultation. Let’s sit down together and talk about what a truly personalized plan at Hirschfeld Oncology could mean for your journey.
Frequently Asked Questions
A cancer diagnosis can feel overwhelming, and it’s natural to have a lot of questions. We’ve put together some straightforward answers to the things patients most often ask about neoadjuvant chemotherapy, hopefully giving you some clarity as you take the next steps.
How Do We Know If the Treatment Is Working?
This is one of the biggest advantages of getting chemotherapy before surgery. We aren't just hoping it works; we're watching it happen. You can think of it as getting a real-time report card on how the cancer is responding.
We track the tumor’s progress closely using imaging scans, like CTs or MRIs. These scans let us measure the tumor and see if it’s shrinking. This constant feedback is incredibly reassuring and allows your care team to either stick with the plan or, if needed, pivot to a different approach. You're never in the dark.
What Are the Most Common Side Effects?
The side effects really depend on the specific drugs in your regimen, and everyone’s experience is a little different. That said, some of the most common ones are fatigue, nausea, and hair loss. But please know, managing these side effects is a huge part of your treatment plan, not an afterthought.
We work proactively to keep you as comfortable as possible. This often includes:
- Anti-nausea medications given before you feel sick to head off discomfort.
- Nutritional guidance to help you keep your strength up.
- Careful dose adjustments to strike the perfect balance between fighting the cancer and protecting your quality of life.
Our goal is to keep you strong enough to move forward with surgery as planned. We’ll be right there with you, managing any challenges that pop up and making your well-being the top priority every step of the way.
Can This Therapy Make My Tumor Disappear Completely?
It's absolutely possible. In some cases, neoadjuvant chemotherapy works so well that it shrinks the tumor until there are no active cancer cells left. When this happens, it's called a pathological complete response (pCR).
This means that after the surgeon removes the tissue where the tumor was, the pathologist examines it under a microscope and finds zero cancer. Achieving a pCR is a fantastic outcome and often points to a very positive long-term prognosis. It’s a clear sign that the cancer was highly sensitive to the treatment, which is wonderful news.
For more information on patient care and other health topics, you might also find this list of general patient FAQs helpful.
At Hirschfeld Oncology, we know that understanding your treatment is the first step toward feeling in control. If you have more questions or want to discuss a treatment plan designed specifically for you, please reach out to our compassionate team for a consultation. Learn more at https://honcology.com/blog.





.png)


.png)
.png)




