When we see a loved one with cancer losing weight, our first instinct is often to say, "You just need to eat more." While well-intentioned, this advice misses the core of a much more complex problem: cancer cachexia.
This condition isn't simple weight loss. It's a debilitating "wasting syndrome" driven by the cancer itself, marked by severe muscle loss, persistent inflammation, and overwhelming fatigue. It can't be fixed just by increasing calorie intake.
A Deeper Look at Cancer Cachexia

Understanding cancer cachexia means shifting our perspective. It’s not about a lack of appetite or a failure to eat; it's a profound metabolic hijacking of the body.
Think of it this way: your body is like a finely tuned engine, and the food you eat is its fuel. Normally, the engine uses this fuel efficiently to power everything you do. But cancer throws a wrench in the works. It releases inflammatory signals that essentially reprogram your metabolism, forcing the engine to run inefficiently at full throttle, burning through not only the fuel you provide but the engine's own components—your muscle and fat.
No matter how much high-octane fuel you try to pump in, the engine just keeps devouring itself.
Cachexia vs Simple Weight Loss Key Differences
It’s essential to distinguish this syndrome from other forms of weight loss. They are fundamentally different processes with very different implications for a patient's health.
This table highlights why simply encouraging a patient with cachexia to eat more can be ineffective and frustrating for everyone involved. The body is actively breaking itself down, a process that nutrition alone cannot stop.
At Hirschfeld Oncology, we see managing cachexia as a critical part of comprehensive cancer care. Our approach is twofold: aggressively treat the underlying cancer while deploying supportive strategies to preserve strength and function. Helping patients figure out what to eat during chemotherapy is a key part of this, but it’s always within the larger context of fighting this complex syndrome on multiple fronts.
What's Really Happening Inside the Body?
To get a real handle on cancer cachexia, we have to look past the number on the scale and dive into what's happening at a biological level. This isn't just about not eating enough; it's a complicated, systemic problem created by the cancer itself. You can think of the tumor as a hijacker, rewiring the body's control panel and sending out signals that throw everything into disarray.
The core of this problem is systemic inflammation. A tumor doesn't just sit there quietly—it pumps out inflammatory messengers, called cytokines, that flood the bloodstream. Imagine these cytokines as constant, blaring false alarms. They convince the body it's facing a massive, unending crisis, forcing it into a state of emergency that prioritizes short-term survival at a terrible long-term price.
This state of constant high alert is what ignites the profound metabolic shifts that define cachexia.
How Metabolism Gets Hijacked
The body’s reaction to these faulty inflammatory signals is both aggressive and self-destructive. Instead of conserving energy, the metabolism goes into overdrive. It creates a hypermetabolic state, burning through calories at an alarming rate, even when you're just resting. This forces the body to start scavenging for fuel from its own tissues.
It doesn’t just stop with burning fat, either. The cytokines specifically target and break down muscle tissue in a process known as proteolysis.
"This isn't a passive wasting away. It's an active, inflammatory-driven process of self-consumption. The body is chemically instructed to dismantle its own muscle and fat tissue to feed the tumor and the very inflammatory response it creates."
This command to break down muscle is relentless. It means that no matter how much protein a patient manages to eat, their body is actively blocked from using it to build or even hang onto the muscle they have. It's like trying to fill a bucket with a giant hole in the bottom—the resources just keep pouring out.
The Key Drivers of the Wasting Process
Several factors work in concert to cause the devastating spiral of cancer cachexia. Seeing how they connect makes it clear why simply "eating more" isn't a fix.
- Inflammatory Cytokines: Molecules like TNF-alpha and IL-6 are the main instigators. They are directly responsible for triggering muscle breakdown, killing appetite, and disrupting how the body uses nutrients.
- Altered Protein Metabolism: The body’s natural balance shifts dramatically. It moves away from building muscle (anabolism) and gets locked into a state of breaking it down (catabolism). The scales are tipped heavily toward wasting.
- Hormonal Disruption: These inflammatory signals also mess with critical hormones that regulate appetite and help maintain muscle, making a bad situation even worse.
This destructive biological cascade is especially common in certain cancers we treat here at Hirschfeld Oncology. Pancreatic and gastric cancers, for instance, are notorious for being highly metabolically active and producing huge amounts of these inflammatory cytokines. It's why up to 80% of patients with these cancers develop some degree of cachexia, which makes managing it a critical part of their overall treatment from day one.
When you look at the hidden causes, it becomes clear that cachexia is a direct, physiological consequence of the cancer. It's a systemic response to the disease, not a personal failure of willpower or diet. Understanding that fact is the first and most important step toward managing it with compassion and effective medical care.
Recognizing the Signs and Stages of Cachexia
Spotting cancer cachexia early on is one of the most powerful things we can do, but its first hints are tricky. They often masquerade as the usual side effects of cancer or its treatment, making them easy to dismiss. But this is far more than just a number dropping on the scale; it's a collection of symptoms pointing to a deep-seated metabolic crisis.
The most glaring sign is, of course, unintentional weight loss, particularly the loss of muscle. This isn’t the kind of weight you lose from a diet. It’s an involuntary wasting away that leaves clothes baggy and the body feeling frail. You might notice it in the mirror or feel it when trying to lift something you used to handle with ease.
Beyond the physical changes, there's the fatigue. This isn't just feeling tired—it's a profound, bone-deep exhaustion that sleep can't fix. Simple tasks, like walking to the mailbox, can suddenly feel like climbing a mountain. This happens because the body, in a state of alarm, has started to cannibalize its own energy reserves.
The Diagnostic Criteria Explained
To turn a suspicion into a diagnosis, we rely on internationally recognized criteria. These guidelines create a clear, measurable standard, ensuring that cachexia isn't overlooked until it becomes severe.
A formal diagnosis isn't based on one single factor. Instead, we look for a specific combination of signs:
- Significant Weight Loss: An involuntary loss of more than 5% of body weight over the last six months.
- Low Body Mass: A Body Mass Index (BMI) under 20, paired with continued weight loss of more than 2%.
- Evidence of Muscle Loss: Clinical proof of sarcopenia (advanced muscle loss) happening alongside more than 2% weight loss.
We also look for other clues, like a persistent loss of appetite (anorexia) and elevated inflammatory markers showing up in blood work. The problem is, even with these clear benchmarks, cachexia is often missed. One study found that while 27.5% of cancer patients clearly met the criteria, a formal diagnosis often lagged months behind the appearance of symptoms, delaying critical support. You can read more about these diagnostic challenges in this 2023 study.
This timeline shows exactly how a tumor can hijack the body's metabolism.
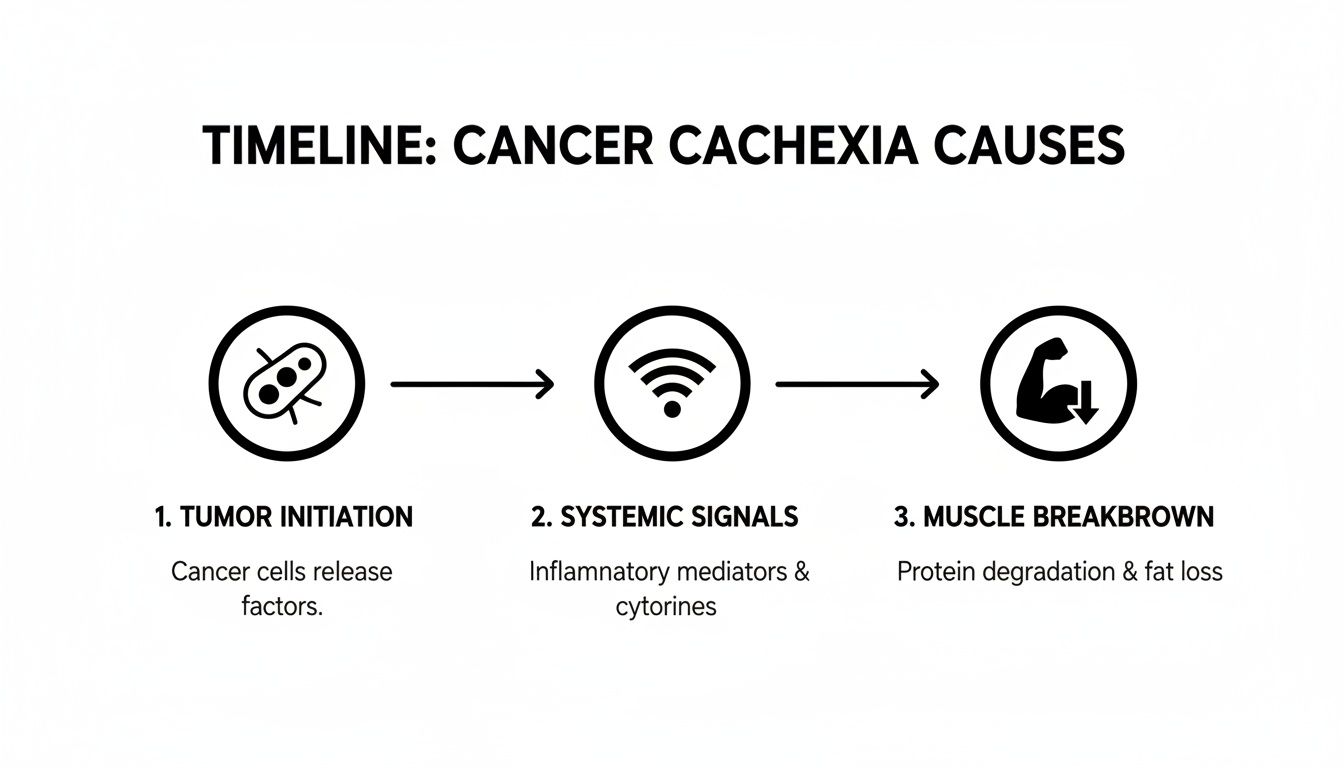
It’s a chain reaction: the tumor sends out signals that trigger a system-wide inflammatory response, which in turn forces the body to break down its own muscle and fat for fuel.
The Three Stages of Cachexia
It helps to think about cachexia not as a single event, but as a process with distinct stages. Knowing where a patient is on this spectrum allows us to customize our approach and set realistic goals for their care.
- Pre-cachexia: This is the earliest warning sign. We might see minor weight loss (less than 5%), a dip in appetite, and subtle metabolic changes. Acting now gives us the best shot at preserving strength and function.
- Cachexia: This is the stage where a formal diagnosis is typically made. Weight loss now exceeds 5%, and it's usually accompanied by poor food intake and systemic inflammation. Symptoms like fatigue and muscle weakness become much more obvious.
- Refractory Cachexia: In this advanced stage, the cancer is often progressing and isn't responding well to anti-cancer treatments. The goal of care shifts from reversing the process to managing symptoms and maximizing comfort, as aggressive nutritional fixes are unlikely to help.
Recognizing these stages isn't about marking a path of decline—it's about creating a roadmap for intervention. The sooner we identify the signs of pre-cachexia, the more tools we have to slow its progression and help patients hold onto the strength they need for the fight ahead.
This is where patients and caregivers become crucial members of the care team. Keeping a simple log of weight, appetite, energy levels, and physical abilities can provide your oncologist with the hard data needed for an early diagnosis. Don't wait. Bringing up these changes right away ensures that a management plan can start when it will do the most good.
How Cachexia Affects Cancer Treatment and Outcomes
Cancer cachexia isn’t just a side effect of the disease; it's a direct threat to the success of the treatment itself. The severe muscle wasting and malnutrition it triggers fundamentally weaken the body, creating a dangerous ripple effect that can undermine even the most promising therapies.
When the body loses its strength, its ability to handle treatments like chemotherapy, radiation, or immunotherapy plummets. I often tell patients to think of their physical strength as a shield. A strong body can withstand the rigors of treatment, but as cachexia chips away at muscle and energy reserves, that shield gets thinner, leaving them vulnerable.
This puts oncologists in a very tough spot. We're often forced to make difficult calls to protect a patient from the very treatments that are meant to save them, simply because their body can no longer handle the toxicity.
Treatment Compromises and Their Consequences
When a patient becomes too frail, the entire treatment plan is jeopardized. This often forces us into several necessary but deeply frustrating adjustments that can hurt the chances of a good long-term outcome.
- Dose Reductions: The planned chemotherapy dose might be too harsh for a body that has lost significant muscle, forcing the oncologist to dial it back.
- Treatment Delays: If a patient is too weak or their blood counts won't recover, treatment cycles get postponed. This gives the cancer precious time to grow and adapt.
- Stopping Treatment Altogether: In the most severe cases, the body simply can't take any more. We may have to stop a potentially curative treatment and shift to less aggressive or purely palliative options.
Every one of these compromises directly impacts the odds of success. That’s why managing cachexia isn't just about comfort—it's about keeping the patient strong enough to stay in the fight and stick to their treatment schedule. To see how we measure this, you can learn more about the ECOG Performance Status scale in our article.
The Sobering Impact on Survival
The link between cachexia and a patient's prognosis is stark and undeniable. This isn't just a complication of cancer; it is a primary cause of death. The profound metabolic chaos it unleashes can simply become too much for the body to handle.
Cachexia is the direct cause of death in a staggering 20-30% of all cancer patients. The syndrome creates such extreme depletion that vital organs can no longer function, ultimately leading to organ failure.
The danger is particularly acute in certain cancers. For patients with pancreatic or lung cancer, the prevalence of cachexia can be as high as 60-90%. The data is clear: mortality rates climb dramatically as weight loss gets worse. A major analysis showed that patients with cachexia had a risk of death that was more than ten times higher than those without it. You can explore more about these cachexia mortality findings on EurekAlert.
This highlights a critical truth: fighting cachexia is fighting cancer. By preserving muscle, supporting nutrition, and managing symptoms, we give patients the strength they need to tolerate treatment, improve their quality of life, and give their cancer therapy the best possible chance to work. It’s an active, essential part of any effective cancer care plan.
Modern Strategies for Managing Cancer Cachexia

Tackling cancer cachexia is not a one-shot deal. It demands a coordinated, multi-front attack because we're fighting a complex metabolic syndrome, not just a simple lack of appetite. Simply telling a patient to “eat more” just doesn’t work.
The most effective approach integrates nutritional support, medication, physical activity, and supportive care to fight the wasting process from every possible angle. Think of it as a team effort where each player has a critical role. Nutrition provides the building blocks, medications help manage appetite and inflammation, and exercise signals the body to hold onto precious muscle.
The Cornerstone of Nutritional Support
While nutrition alone can't reverse cachexia, it is the absolute foundation of any management plan. The goal isn't just about cramming in calories; it's about providing the right kind of calories and protein to push back against the body's catabolic state. This is where an oncology dietitian becomes an indispensable part of the care team.
They go far beyond the frustrating advice of "just eat" by creating a personalized plan focused on:
- Calorie Density: Prioritizing foods that pack a lot of energy into small servings, such as avocados, olive oil, nuts, and full-fat dairy.
- High-Quality Protein: Focusing on easily digestible proteins from sources like eggs, fish, poultry, and specialized supplements to give the body the raw materials it needs for muscle repair.
- Small, Frequent Meals: Shifting from three large meals to five or six smaller, nutrient-rich mini-meals or snacks to navigate poor appetite and early feelings of fullness.
This strategy helps make eating less of a chore and more of a manageable, therapeutic part of the day.
Pharmacologic Interventions to Aid the Fight
Alongside dietary changes, certain medications can help address the underlying biological drivers of cachexia. These aren't cures, but they are powerful tools that can help tip the metabolic scales back in the patient’s favor. They create a crucial window of opportunity for nutritional and physical therapies to have a greater impact.
Your oncologist might consider several options based on your unique situation. These could include appetite stimulants to improve food intake or anti-inflammatory agents to cool down the systemic inflammation that fuels muscle breakdown. This is a highly individualized decision, as what works for one person may not be right for another.
It's important to view these medications as part of a larger strategy. They work best when combined with dedicated nutritional support and a safe exercise regimen, creating a synergistic effect that gives the body a better chance to fight back against the wasting process.
The Critical Role of Physical Activity
The idea of exercising when you feel profoundly weak and fatigued can seem completely backward, but it's one of the most vital components of managing cachexia. The key is gentle, targeted movement—not a punishing workout at the gym.
Physical therapy and light resistance training send a powerful signal to the body: "This muscle is needed—don't break it down." Even minimal activity can help preserve muscle mass, improve physical function, and surprisingly, even reduce fatigue. A physical therapist specializing in oncology can design a safe and effective program that might include:
- Light resistance exercises using bands or small weights.
- Gentle walking or stationary cycling.
- Simple stretching and flexibility movements.
This proactive approach helps patients maintain independence and the physical strength required to better tolerate their cancer treatments.
Comprehensive Cachexia Management Strategies
A successful management plan requires a multi-faceted approach. The table below summarizes the key pillars of care, their goals, and practical interventions.
By combining these strategies, we can create a more robust and personalized plan to help patients feel stronger and live better during treatment.
Palliative and Supportive Care for Quality of Life
Finally, managing the symptoms that make cachexia so debilitating is absolutely essential. This often requires a dedicated focus on pain and symptom management to address issues like nausea, shortness of breath, and pain that can make eating and daily life incredibly difficult. Palliative care is all about improving comfort and quality of life, no matter the stage of illness.
The impact of cachexia varies dramatically by cancer type. For example, pancreatic cancer has a 60-90% incidence rate, and for gastric cancer, it's around 80-90%. By controlling symptoms, we empower patients to engage more fully with their families and the activities they enjoy, making this holistic focus a central part of a compassionate and effective management plan.
Hope and Innovation in Cachexia Care
Grasping the science, symptoms, and serious impact of cancer cachexia can be incredibly overwhelming. It’s a condition that doesn’t just weaken the body; it can erode a person’s spirit and sense of hope. But that’s not where the story has to end.
At Hirschfeld Oncology, our entire philosophy is built on rewriting that narrative. We focus on proactive management, truly personalized care, and fighting to preserve quality of life, even when dealing with advanced cancer.
For many of our patients, especially those with pancreatic, gastric, or other GI cancers where cachexia is a constant threat, aggressive, high-dose treatments just aren't a viable option. Their bodies are simply too frail to handle the toxicity. This is exactly where our approach can make all the difference. We specialize in crafting treatment plans that attack the cancer without overwhelming the patient.
A Different Approach to Treatment
Dr. Azriel Hirschfeld’s expertise is in designing treatment regimens that find the crucial balance between effectiveness and tolerability. It’s about moving past a rigid, one-size-fits-all protocol and embracing strategies that work with the patient, not against them.
For someone weakened by cachexia, this often looks like:
- Low-Dose, Metronomic Chemotherapy: This approach uses smaller, more frequent doses of chemotherapy. The goal is to keep constant pressure on the cancer cells without the debilitating side effects of a high-dose infusion.
- Targeted Therapies: We use advanced treatments designed to attack specific weaknesses in cancer cells, which often means fewer side effects for the rest of the body compared to traditional chemo.
- Continuous Monitoring and Adjustment: A treatment plan should never be set in stone. We watch closely how a patient is feeling and responding, making immediate adjustments to doses and schedules to manage side effects and help them maintain their strength.
This careful, adaptive method is essential. It allows us to keep fighting the cancer while also bringing in the supportive care needed to manage cachexia head-on. By lightening the treatment burden, we help our patients hold onto the energy they need for their daily lives.
At its core, managing what is cancer cachexia is inseparable from managing the cancer itself. A successful plan addresses both simultaneously, recognizing that a patient’s strength and well-being are the foundation upon which effective cancer treatment is built.
Taking the Next Step with Hirschfeld Oncology
Navigating a complex diagnosis like advanced cancer complicated by cachexia requires a dedicated, experienced team. You can learn more about our specific strategies for this condition in our guide on advances in managing GI cancer-related cachexia.
If you or a loved one are facing this dual battle, you are not alone. We encourage patients, families, and referring physicians to schedule a consultation with our team. Together, we can explore a personalized path forward—one that combines medical expertise with a deep commitment to restoring strength, hope, and quality of life.
Your Questions About Cancer Cachexia, Answered
A cancer diagnosis is overwhelming enough. When a complex condition like cachexia enters the picture, it’s natural to feel lost and have a million questions. We've gathered some of the most common ones we hear from patients and their families, offering clear, straightforward answers to help you understand what's happening.
Can I Reverse Cancer Cachexia by Just Eating More?
This is one of the toughest, yet most important, things to understand: unfortunately, no. It’s a common misconception. Cancer cachexia isn't just a nutritional issue; it's a deep-seated metabolic problem sparked by the body's inflammatory response to the cancer itself.
Your body's entire energy-management system goes haywire. It starts breaking down muscle and fat for fuel, no matter how many calories you're taking in. Think of it like trying to fill a bucket with a massive hole in the bottom. You can keep pouring water in (calories), but you can't fix the leak without patching the hole. That's why simply eating more, while a critical piece of the puzzle, can't solve the problem alone. We have to tackle it from multiple angles—with medication, specialized nutrition, gentle exercise, and, most importantly, treating the cancer.
When Should I Talk to My Doctor About Potential Cachexia?
The moment you notice something is off. Talk to your oncologist as soon as you experience any unexplained weight loss, a nagging lack of appetite, or a deep fatigue that rest just doesn't seem to touch. The earlier we can intervene, the better.
Even if you're in the very early "pre-cachexia" stage with only minor weight loss (less than 5%), taking action now can help you hold onto vital muscle mass and strength, which makes a world of difference in how well you tolerate treatment.
Don't ever dismiss these symptoms as just "normal" side effects of cancer. Bring them up at your very next appointment. Giving your care team a heads-up allows them to step in when it counts the most.
As a Caregiver, What’s the Most Important Thing I Can Do?
Your most powerful role is to be a source of comfort and to take the pressure off mealtimes. The loss of appetite (anorexia) that comes with cachexia is real and physical. Pushing food can backfire, creating a cycle of stress, anxiety, and guilt for someone who already feels unwell.
Instead, shift your focus from quantity to support. Here’s how:
- Think small and often: Offer nutrient-packed snacks or mini-meals throughout the day. A few bites every couple of hours are far less intimidating than three large plates.
- Be their eyes and ears: Help them keep a simple log of their weight, what they're able to eat, and how they're feeling. Sharing these concrete details with the oncology team is incredibly helpful.
- Create a peaceful space: Your ability to provide a calm, supportive, and low-stress environment is more valuable than you can imagine. It has a huge impact on their quality of life through this journey.
Are There Specific Treatments Just for Cachexia?
While getting the cancer under control is the number one way to fight cachexia, we absolutely have supportive treatments that can manage the symptoms directly. These aren't cures for cachexia, but they are essential tools that help us push back against its effects and give your body a fighting chance.
These might include appetite stimulants, medications to reduce inflammation, or other agents that help counteract the body's metabolic chaos. At a practice like Hirschfeld Oncology, these options are woven into a personalized plan that also includes one-on-one nutritional counseling and physical therapy. It's a comprehensive approach. On top of that, research into new, targeted therapies for cachexia is a very active and promising field, giving us real hope for even better tools in the near future.
At Hirschfeld Oncology, we believe that managing the effects of cancer is just as important as treating the disease itself. If you or a loved one are struggling with the challenges of cancer cachexia, our team is here to provide expert, compassionate care. Explore our blog for more insights or contact us to schedule a consultation. Learn more at https://honcology.com/blog.





.png)


.png)
.png)




