When you hear the term dose-dense chemotherapy, you might assume it means stronger, more toxic drugs. But it's actually about being smarter with the timing, not harsher with the dose.
It’s a treatment strategy where we give the standard dose of chemotherapy, but we shorten the time between cycles—usually from every three weeks to every two weeks.
What Is Dose Dense Chemotherapy
At its heart, dose-dense chemotherapy is a powerful shift in the rhythm of treatment. Think of it like dealing with a stubborn patch of weeds in your garden. With a standard approach, you might spray them every three weeks. That works for a while, but it gives the hardiest weeds just enough time to start sprouting again before you hit them with the next round.
Dose-dense therapy is like coming back with that same weed killer every two weeks instead. You're hitting the weeds just as they’re trying to recover, never giving them a chance to regain their footing. We apply that exact same principle to fighting cancer cells.
The Science Of Smarter Timing
This strategy is built on a solid biological foundation known as the Norton-Simon hypothesis. This model showed us something crucial: cancer cells tend to regrow fastest right after a chemotherapy treatment has shrunk the tumor. It’s their moment of greatest vulnerability.
By shortening the interval between treatments, we strike again precisely during that vulnerable regrowth phase. This increases what we call dose intensity—the amount of drug the tumor is exposed to over time—without ever increasing the toxicity of any single dose. The goal is to apply relentless pressure that overwhelms the cancer's ability to repair and multiply.
A Visual Comparison
The difference in scheduling is subtle but makes a world of difference in the treatment's impact.
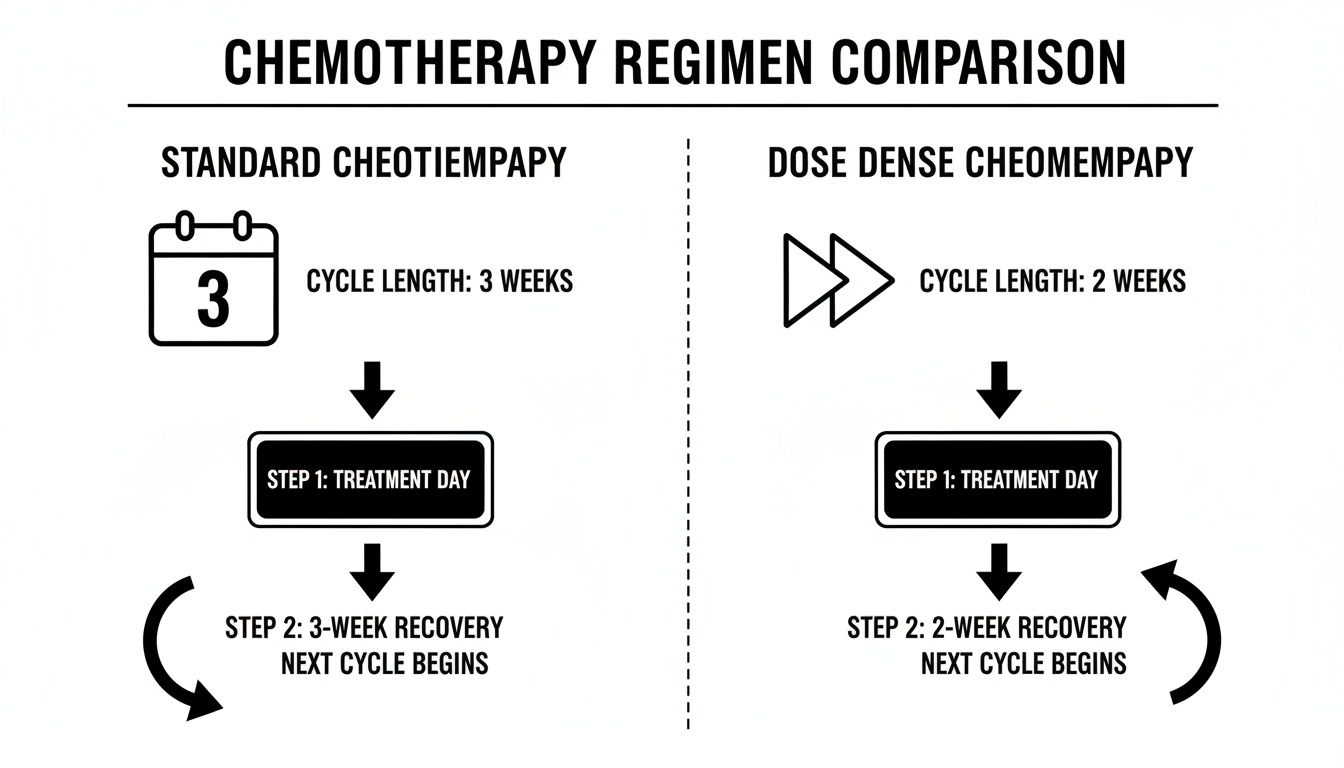
As the diagram shows, the only thing that changes is the time between infusions. By compressing the schedule, we intensify the therapeutic pressure on the cancer cells.
How Does It Work In Practice?
Let's break down the core principles behind each approach to see exactly how they differ.
While the changes seem minor on paper, switching from a 3-week to a 2-week cycle fundamentally alters the pressure we put on a tumor. This is a deliberate, evidence-based strategy designed to prevent cancer cells from bouncing back.
By delivering the same doses more frequently, we exploit a key weakness in tumor biology. For more on the clinical evidence behind this approach, you can explore detailed research from sources like The ASCO Post.
The Science Behind a Faster Treatment Rhythm
To really understand why a quicker chemotherapy schedule works, it helps to think about how tumors behave. Cancer cells, particularly the aggressive ones, don't just grow at a steady pace. After a round of chemotherapy damages a tumor, the surviving cells often try to regrow—and they do it fast.
This rapid regrowth phase is the tumor’s most vulnerable moment. A standard chemotherapy schedule, often every three weeks, leaves a pretty big gap for those cancer cells to recover, repair the damage we just did, and start multiplying again. Dose-dense chemo is designed to slam that window shut.
Capitalizing on Cancer's Rebound
The whole idea behind dose-dense chemotherapy is to hit the cancer cells again before they've had a chance to fully recover. By giving the next treatment sooner—usually every two weeks instead of three—we interrupt that repair cycle. It’s a strategy of applying relentless pressure to overwhelm the tumor’s ability to bounce back.
This approach increases the dose intensity, which is just a technical way of saying the tumor is exposed to more drug over a shorter period. It's crucial to understand this doesn't mean we're giving a larger, harsher dose each time. The individual dose of the medication is the same; it's the frequency that's different. That small change in timing can make a world of difference in the outcome.
By interrupting the cancer cell recovery process, dose-dense therapy prevents the tumor from regaining momentum. The goal is to keep it constantly off-balance, making it more difficult for it to survive and spread.
This strategic timing isn't just a theory. It's a proven concept in oncology that comes from decades of observing how tumors respond to treatment. We are essentially using the tumor's own biology against it.
Maximizing Impact Without Increasing Toxicity
Naturally, one of the first questions people ask is whether this faster schedule is harder on the body. While it presents its own set of challenges, the goal is to maximize the anti-cancer effect, not just ramp up toxicity. The schedule is meticulously planned to give healthy cells just enough time to recover while cancer cells are still down for the count.
For a deeper look into treatment schedules, our guide explores how often chemotherapy is given and the factors that shape these crucial decisions.
The key benefits of this scientific approach include:
- Preventing Tumor Regrowth: It directly targets the period when cancer cells are working hardest to repopulate.
- Increasing Cumulative Pressure: Over the entire course of treatment, the tumor faces a more sustained and intense therapeutic assault.
- Improving Outcomes: In many cancers, this strategy has been shown to reduce the risk of recurrence and improve long-term survival rates.
Ultimately, the science behind dose-dense chemotherapy is all about smart timing. By understanding and exploiting the growth patterns of cancer cells, we can gain a powerful upper hand in the fight.
Real-World Evidence That Supports This Approach
The theory behind dose-dense chemotherapy is promising, but what really matters is how it performs for actual patients. The evidence backing this approach isn't just a hypothesis; it's the result of decades of clinical research that has fundamentally changed the standard of care for many cancers.
This strategy has been put to the test in major clinical trials, and the results have consistently shown its power to improve patient outcomes. These studies give us the hard proof that a faster treatment rhythm can lead to better, more durable results.
The Landmark CALGB 9741 Trial
One of the most important studies in this field was the Cancer and Leukemia Group B (CALGB) 9741 trial. This was a massive study that looked at women with early-stage breast cancer, directly comparing a dose-dense schedule to the standard three-week cycle. The results were so clear that they helped establish this method as a superior strategy.
The trial discovered that patients who received chemotherapy every two weeks had dramatically better outcomes. To be specific, the dose-dense group saw a 26% improvement in disease-free survival. That means they lived longer without their cancer coming back—a powerful signal that the timing of chemotherapy is a critical piece of the puzzle.
Even more impressive, the study showed a remarkable 31% improvement in overall survival for those on the dose-dense schedule. This wasn't just about delaying a recurrence; it was about saving lives. These findings confirmed that increasing the intensity by shrinking the treatment interval is a highly effective way to fight breast cancer. You can dig into the specifics of how this trial shaped modern oncology in the research published by the National Institutes of Health.
What This Evidence Means for You
It's one thing to read about clinical data, but it's another to understand what it means for you personally. A percentage in a study represents real people who gained more time with their families and a better shot at a future without cancer. The success seen in these trials is why dose-dense chemotherapy has become such a trusted and effective standard of care.
For many patients, particularly those with certain types of breast or ovarian cancer, the evidence shows that a dose-dense schedule offers a clear advantage over traditional timing, significantly reducing the risk of cancer coming back.
When you boil down years of clinical evidence, a few key takeaways emerge:
- Reduced Recurrence: By keeping relentless pressure on cancer cells, this approach makes it much less likely that the disease will return after the initial treatment is over.
- Improved Survival: Landmark trials have shown time and again that patients on a dose-dense schedule often live longer.
- A Proven Strategy: This isn't some new, experimental idea. It's a well-established treatment protocol backed by solid scientific data.
This mountain of evidence gives us a strong foundation for using dose-dense chemotherapy in the right situations. It’s a powerful tool for oncologists and a source of real hope for patients, proving that a smarter schedule can lead to profoundly better outcomes.
Which Cancers Respond Best to Dose Dense Therapy

While the logic behind a faster treatment rhythm is sound, dose-dense chemotherapy isn’t a one-size-fits-all solution. Its effectiveness really shines in specific cancers whose biology makes them particularly vulnerable to this accelerated schedule.
The main areas where we’ve seen this strategy become a cornerstone of care are breast cancer, ovarian cancer, and certain lymphomas. These cancers share a common trait: they tend to have a high growth fraction, meaning a large percentage of their cells are actively dividing at any given time. This rapid cell turnover is exactly what we target. Hitting them with chemotherapy more frequently disrupts that constant cycle of replication before the tumor can recover and regroup.
Breast Cancer: A Prime Candidate
Nowhere has dose-dense therapy made a bigger impact than in breast cancer, especially in the adjuvant setting (treatment after surgery). It has become a well-established standard of care for patients with high-risk, early-stage disease—think node-positive tumors or those with other aggressive features. The benefits are particularly clear for premenopausal women, whose cancers often grow more quickly.
We're constantly refining our understanding of who benefits most. For instance, recent research underscores just how much dose-dense chemotherapy improves outcomes in hormone receptor-positive (HR+) breast cancer. One pivotal study showed a 23% improvement in disease-free survival and a 20% gain in overall survival for patients on this regimen, especially when their tumors showed low endocrine activity. You can learn more about these important findings from the Journal of Clinical Oncology.
For a deeper dive into treatment options, you can also explore our guide on breast cancer chemotherapy.
Ovarian Cancer and Lymphomas
Beyond breast cancer, this approach shows significant promise in other aggressive cancers.
- Ovarian Cancer: This cancer type often responds well to platinum and taxane-based chemotherapy. Dose-dense regimens, like giving paclitaxel every week instead of every three weeks, have proven to improve both progression-free and overall survival in several major clinical trials.
- Lymphomas: Certain fast-growing lymphomas, such as diffuse large B-cell lymphoma (DLBCL), are also ideal candidates. Their rapid proliferation makes them highly sensitive to chemotherapy, and shortening the treatment interval helps us achieve deeper, more durable remissions.
A faster treatment schedule is most effective against cancers that grow and divide rapidly. By hitting these aggressive cells more frequently, we exploit their biological impatience and disrupt their ability to multiply unchecked.
Oncologists are also exploring its potential in other tough-to-treat cancers, like pancreatic and colorectal, often as part of a more personalized strategy. The key is always to match the treatment’s rhythm to the tumor’s specific biology, turning its own aggressive nature into its greatest weakness. This careful alignment of cancer type and treatment timing is central to modern, effective oncology care.
Staying Strong and Well During Treatment
Your health and comfort are our absolute priorities, especially when you're on a dose-dense chemotherapy schedule. Because the treatments are closer together, we need to be smart and proactive about managing your well-being. The faster rhythm simply means your body has less downtime to bounce back, which can dial up the risk of certain side effects.
The usual suspects are fatigue, a dip in red blood cells (anemia), and a drop in your infection-fighting white blood cells (neutropenia). While those terms can sound intimidating, we have a whole playbook of modern, highly effective ways to manage them. We don't wait for problems to arise; we get ahead of them.
Growth Factors: Your Immune System's Reinforcements
One of the keys to making a dose-dense schedule work safely is using a class of medications called growth factors. These aren't chemotherapy. Instead, think of them as a support crew for your bone marrow, sending a signal to ramp up production of new white blood cells.
The most common one we use is G-CSF (Granulocyte-Colony Stimulating Factor). It’s like calling in reinforcements for your immune system. By helping your body replenish its defenses quickly, we can keep your treatment on schedule and significantly lower your risk of picking up an infection.
Getting ahead of side effects is the secret to a successful dose-dense regimen. By using tools like growth factors, we can stick to the aggressive treatment plan your cancer demands while fiercely protecting your body's strength.
This proactive approach lets us deliver the full power of the faster schedule without ever putting your safety on the back burner.
A Plan to Protect Your Quality of Life
Keeping you feeling as good as possible is a team effort, and it involves more than just medication. We’ll build a complete supportive care plan tailored specifically to you.
Here’s what that looks like in practice:
- Keeping a Close Watch: We'll do frequent blood tests to monitor your cell counts like a hawk. This lets us see a potential issue developing and step in long before it becomes a real problem.
- The Power of Hydration: Staying hydrated is non-negotiable. We often recommend IV fluids to help your body process the chemo drugs efficiently and ease the strain on your kidneys.
- Managing Symptoms Head-On: Whether it's nausea, fatigue, or something else, we have targeted medications and practical strategies to help you manage it and feel more like yourself.
The goal here is to empower you. With the right supportive care, diligent monitoring, and a proactive mindset, navigating dose-dense chemotherapy is absolutely achievable. It's all about fighting the cancer aggressively while supporting you compassionately every step of the way.
Personalizing Your Dose-Dense Treatment Plan

Standard protocols are a good starting point, but the best cancer treatment is always the one designed specifically for you. At Hirschfeld Oncology, we specialize in going beyond the standard playbook, particularly for patients facing complex, advanced, or treatment-resistant cancers.
A dose-dense strategy is a powerful tool in our arsenal, but how we apply it is what truly sets our approach apart. This is never a one-size-fits-all decision. Your unique cancer biology, previous treatments, and personal health goals inform every step we take.
Crafting a Custom Strategy
Our entire process is built around tailoring this potent approach to your individual situation. We don't just apply a faster schedule; we adapt the core principles of dose-dense therapy to maximize its impact while carefully protecting your quality of life.
What does this look like in practice? It might involve:
- Integrating Therapies: We often combine a dose-dense schedule with other advanced treatments, like targeted therapy or immunotherapy, to create a multi-pronged attack on the cancer.
- Adapting Schedules: Your plan isn't rigid. We continuously monitor how you're responding and may adjust the timing or supportive care to ensure the treatment is both effective and manageable for you.
- A Tool for Tough Cases: For patients whose cancer has progressed despite standard treatments, a dose-dense approach can provide a vital new strategy to regain control over the disease.
The heart of our philosophy is partnership. We work closely with you to map out a path that treats the cancer aggressively while preserving your strength and well-being.
Our goal is to pair leading-edge science with compassionate, patient-first care. By getting to know your cancer on a deeper level, we can design a plan that offers the best possible chance for a positive outcome. Exciting advances in genomic testing are also starting to shape these decisions, pushing us toward a future of optimizing chemotherapy dose scheduling using genomic data.
Common Questions About Dose-Dense Chemotherapy
Whenever you're exploring a new treatment, it's completely normal to have a lot of practical questions. Let's walk through some of the most common things patients ask us about dose-dense chemotherapy.
Does "Dose-Dense" Mean A Higher Dose of Chemo?
No, and this is a really important distinction. The term "dose-dense" refers to the frequency of your treatments, not the strength of any single dose.
Think of it this way: you receive the same standard amount of medication you'd get on a traditional schedule. The key difference is we give it to you more often—usually every two weeks instead of every three. This strategy is all about keeping consistent, relentless pressure on the cancer cells.
Is This Treatment Harder To Tolerate?
Because of the faster pace, there can be a higher chance of certain side effects, like fatigue or a drop in your white blood cell count. However, modern supportive care has made this approach very manageable for most people.
We get ahead of potential issues by proactively using medications called growth factors. These help your body ramp up its production of white blood cells, which are your primary defense against infection. By monitoring you closely, we can catch and manage any side effects early, helping you get through treatment as safely and comfortably as possible.
The key to tolerating a dose-dense schedule is proactive support. We don't wait for problems to arise; we get ahead of them to keep you strong.
How Do I Know if It Is Right for Me?
That’s a conversation you’ll have in-depth with your oncologist, as it’s a very personal decision. It hinges on several factors, including:
- Your specific type and stage of cancer
- Your overall health and fitness
- Your previous treatment history
Dose-dense therapy has become a standard of care for certain cancers, like early-stage breast cancer, and remains a powerful option for others. A detailed consultation is the only way to truly figure out if this is the right path for your unique situation.
At Hirschfeld Oncology, we specialize in creating personalized treatment plans that align with your specific needs and goals. Learn more about our approach by visiting us at https://honcology.com/blog.





.png)


.png)
.png)




