Receiving a cancer diagnosis is a life-altering moment, and the thought of a first oncology appointment often brings a wave of new questions and anxieties. This initial meeting is really just a detailed conversation—a chance for your oncologist to understand your unique situation, confirm the diagnosis, and start laying out the possible roads ahead.
Think of it as the first step in building your game plan and your partnership with your new medical team.
Your First Oncology Visit: A Step-by-Step Guide
Walking into your first meeting with an oncologist is a major step, moving you from the uncertainty of diagnosis toward a concrete plan of action. It's completely normal to feel a mix of nerves and hope. Knowing what to expect can help turn that anxiety into a sense of control.
This first consultation is intentionally thorough. Your oncologist’s main goal is to get a complete picture of you—not just your cancer. It’s about piecing together your medical history, test results, and personal health goals. You are the most important person in the room, and this is a collaborative discussion to figure out the best path forward, together.
What Is the Purpose of This Appointment?
The goals for this first visit are clear and centered around you. Your doctor wants to make sure you walk out with a solid understanding and a sense of direction.
Here’s what we’ll focus on:
- Confirming Your Diagnosis: We will carefully review all of your pathology reports, imaging scans (like CTs or MRIs), and lab work to be certain about the exact type and stage of the cancer.
- Assessing Your Overall Health: A physical exam and a deep dive into your medical history give us a baseline. This helps us understand how your body might handle different treatments.
- Educating and Informing: We’ll break down what your diagnosis means in plain language and explain the thinking behind the treatment strategies we might recommend.
- Establishing a Partnership: This is the beginning of a relationship. It needs to be built on trust, open communication, and making decisions as a team.
To give you a clearer picture, your appointment will generally follow three main phases.
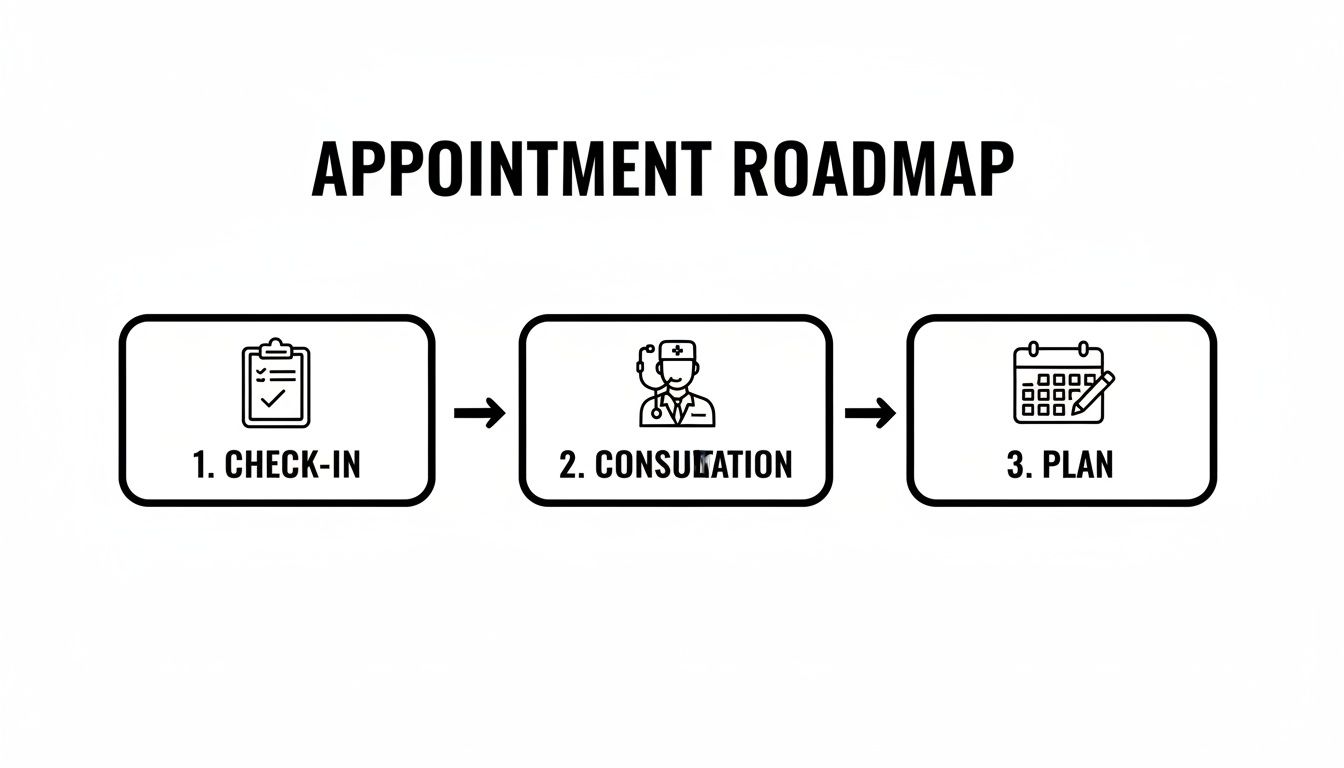
This simple roadmap helps you see how each part of the visit logically leads to the next, all aimed at creating a clear and understandable strategy for your care.
We can break down the flow of the appointment into a simple table to help you visualize the journey.
Your Appointment Roadmap
This structure ensures that we cover all the bases efficiently while giving you plenty of time and space to be heard.
Your first visit is a dialogue, not a lecture. It’s your time to ask every question you have, share your fears, and make sure the path we’re considering feels right for you and your life.
By the end of this appointment, you should feel like you have a dedicated team in your corner. You’ll have a much clearer picture of your diagnosis and a preliminary roadmap for what comes next, even if the final treatment plan depends on a few more tests. This visit is your first big step in taking charge of your health journey.
Getting Ready For Your First Appointment

Walking into your first oncology appointment can feel overwhelming, but a little preparation can make all the difference. Think of it less as a stressful event and more as the first step in building a powerful partnership with your care team. Being organized is your best strategy for clarity and confidence.
Your time with the doctor is incredibly valuable, but it's also limited. The average outpatient oncology visit in the U.S. is a focused 22-23 minutes. Coming prepared helps you make every single one of those minutes count, ensuring you get your questions answered and leave with a clear understanding of what’s next.
Gather Your Medical Records
Your medical history is the blueprint for your treatment plan. Your oncologist is like a detective, and these documents are the essential clues needed to see the full picture right from the start.
Before you head to our office, pull together a folder with these key items:
- Pathology and Biopsy Reports: These are crucial. They confirm the exact type of cancer, including cell types and any specific markers that guide treatment.
- Imaging Scans and Reports: It’s best to bring the actual CDs of your CT, PET, or MRI scans. The images themselves provide visual details that the written reports can't fully capture.
- Recent Lab Work: These numbers give us a snapshot of your overall health and how well your organs are functioning, which helps us tailor a treatment that you can tolerate.
- Operative Reports: If you’ve had any cancer-related surgery, the surgeon’s detailed report is a vital piece of your history.
Having these documents ready to go prevents frustrating delays and gives your oncologist the precise information they need to start building your personalized strategy.
Compile Your Personal Health Story
Your cancer diagnosis is just one part of your story. Your overall health, lifestyle, and medical background play a huge role in how we'll approach your care.
We find it helpful if you can create a simple one-page summary that includes:
- A Full Medication List: Write down everything you take—prescriptions, over-the-counter drugs, vitamins, and even herbal supplements. Don't forget the dosages! A great shortcut is to just take a quick picture of each bottle with your phone.
- A List of Allergies: Make a note of any known allergies to medications, foods, or anything else.
- Your Personal and Family Medical History: Let us know about other chronic conditions you're managing (like diabetes or heart disease) and if there's any history of cancer in your family.
This information helps us avoid potential drug interactions and understand your unique health profile, making your treatment plan as safe and effective as possible.
Prepare Your Questions and Bring Support
This appointment is just as much for you to gather information as it is for the doctor. Coming in with a list of questions ensures that your biggest concerns get the attention they deserve. Seriously, no question is too small or silly.
Your questions are your roadmap. They guide the conversation, ensuring it covers what matters most to you, from treatment specifics and side effects to how it will impact your daily life.
We strongly encourage you to bring a trusted friend or family member along. They can act as a second set of ears, take notes so you don't have to, and offer much-needed emotional support. This frees you up to simply listen and engage in the conversation. For some extra help, check out our guide on essential questions to ask your oncologist. It’s a great resource to help you organize your thoughts and feel more in control.
Understanding Your Diagnosis and Staging

This is the moment in your first appointment where all the pieces of your medical story start to click into place. After gathering all your information, your oncologist will shift gears and begin explaining exactly what it all means. It’s a thoughtful, detailed process where they take your records, lab results, and personal history and weave them together into a clear diagnostic picture.
The main goal here is to replace uncertainty with understanding. You’re going to hear some technical terms, but a good doctor’s job is to act as your translator, breaking it all down into plain English. Think of this as a collaborative review, where we make sure you’re seeing the same picture we are before we talk about what comes next.
Connecting the Dots: Your Medical Evidence
Your oncologist will carefully walk you through the key evidence that built your diagnosis. This isn't just a matter of reading reports aloud; it’s about interpreting them in the context of you. We pull together information from a few different places to create that full picture.
These sources usually include:
- Pathology Reports: This is the bedrock of any cancer diagnosis, the definitive document from your biopsy. It confirms the type of cancer cells and can reveal other critical details. We have a whole guide on how to read a pathology report if you want to dive deeper.
- Imaging Scans: We’ll pull up the actual images from your CTs, MRIs, or PET scans. These are our eyes inside your body, showing us the size and location of any tumors and, crucially, whether the cancer has spread.
- Lab Results: Simple blood tests can give us a surprising amount of information about how your organs are functioning. They sometimes include tumor markers—substances that can point to the presence of cancer.
Alongside all this data, your oncologist will perform a focused physical examination. This hands-on assessment is still incredibly important. It helps us evaluate your overall health, check lymph nodes, and spot any physical signs related to the diagnosis. It’s a vital piece of the puzzle that complements everything we see in the scans and reports.
Demystifying Cancer Staging
One of the most important—and often intimidating—concepts we’ll discuss is staging. It sounds scary, but staging is simply a standardized system doctors use to describe the extent of the cancer. It boils down to answering two main questions: where is the cancer, and how much of it is there?
Think of it like a map. A Stage 1 cancer is like a small, contained campfire in one specific spot. A Stage 4 cancer, on the other hand, is like that fire has sent embers flying, starting new fires in distant parts of the forest. This is what you might hear called metastatic cancer.
The staging process is critical because it helps your oncologist:
- Understand the Prognosis: Staging provides a general idea of the expected outcome, though every single person's journey is unique.
- Determine Treatment Strategy: The cancer's stage is a primary factor in deciding which treatments—like surgery, chemotherapy, or immunotherapy—make the most sense.
- Establish a Baseline: Knowing the stage at diagnosis gives your whole team a starting point to track how well your treatment is working over time.
Staging is not a judgment on your health; it's a clinical tool. It provides a common language for your entire care team to understand the cancer’s status and plan the most effective strategy.
Uncovering Clues with Biomarkers
Beyond staging, your oncologist might bring up biomarkers. These are specific molecules, like genes or proteins, that we can find in your blood, tissue, or other body fluids. They offer powerful clues about what makes your cancer tick.
Imagine your cancer is a locked door. A biomarker test is like finding the right key. It tells us something unique about the cancer cells that we can then target with very specific treatments. For example, certain biomarkers tell us that a cancer will respond incredibly well to a particular targeted therapy or immunotherapy.
Finding these markers is a cornerstone of modern, personalized cancer care. It allows us to move beyond one-size-fits-all approaches and use treatments that are more precise and often have fewer side effects than traditional chemotherapy. This part of the conversation is essential, as it lays the groundwork for a treatment plan designed specifically for you.
Discussing Your Personalized Treatment Options

Once we’ve pieced together the puzzle of your diagnosis and staging, the conversation naturally turns to the most important question on your mind: "So, what do we do now?" This is where a clear plan starts to take shape. It’s not about me telling you what to do; it’s about us figuring it out together.
We'll move from understanding the "what" to building a strategy for the "how." Our goal is to walk through all the tools in our medical toolbox, explaining how each one works and why it might be a good fit for you. Your voice, your values, and your vision for your quality of life are the most important part of this entire process.
You Are a Partner in Your Care
At its heart, modern cancer care is a partnership. We call this shared decision-making, but it’s a simple idea: you and your oncologist are a team. I bring the medical expertise—the knowledge of cancer biology, clinical trial data, and treatment side effects. You bring the most critical expertise of all: you know yourself.
You are the expert on your life, your priorities, and what you’re willing to do to achieve your goals. This conversation is where we merge those two perspectives to create a plan that you can feel truly confident about.
A treatment plan is only as good as its ability to align with a patient's personal goals. Our role is to present the best medical options, explain the risks and benefits clearly, and then listen to what matters most to you.
This way, we ensure the final plan respects your wishes and actually fits into your life.
Exploring Modern Treatment Approaches
The world of cancer treatment has changed dramatically. We now have a whole range of sophisticated therapies that go far beyond what most people imagine when they hear the word "chemo." Each one is designed to fight cancer in a smarter, more precise way.
We'll talk through the options that make the most sense for your specific diagnosis, using simple analogies to make the science easier to grasp.
Here are a few of the key approaches we might discuss:
- Immunotherapy: Think of this as training your body's own immune system to be a cancer-fighting machine. We use medications to take the "disguise" off cancer cells, allowing your natural defenses to finally see them and attack.
- Targeted Therapy: If your cancer has a specific genetic quirk—like a keyhole on its surface—targeted therapy is the custom-made key. These drugs are engineered to find and block the exact pathways that cancer cells use to grow.
- Low-Dose Chemotherapy: This isn't your parents' chemo. We use smaller, more frequent doses to keep the cancer in check while dramatically reducing the harsh side effects you might be worried about. The goal is to help you maintain a high quality of life during treatment.
Understanding your unique genetic test results is often the key that unlocks which of these advanced therapies is right for you.
Tailoring a Plan Just for You
Building your treatment plan is like having a suit custom-tailored. It has to be designed to fit your specific measurements perfectly. A strategy that works wonders for one person might not be the right choice for another, even if they have the same type of cancer.
Your final plan will be a thoughtful blend of several key factors:
- Your Cancer's Biology: The specific type, stage, and any genetic markers we find are the foundation of our strategy.
- Your Overall Health: We'll consider your age, any other medical conditions, and your general fitness to determine which treatments you can handle safely.
- Your Personal Goals: What does success look like to you? Is it aiming for a cure at all costs? Is it managing symptoms so you can keep working? Is it preserving your energy for your family?
Putting this all together takes focus and collaboration. Here in New York City, we're fortunate. While across the United States there is roughly 1 oncologist for every 256 new cancer cases each year, the ratios here allow us to give you the dedicated, unhurried time needed to build such a detailed plan.
You will leave this first appointment not just with answers, but with a clear, actionable roadmap. This plan is designed with a single purpose: to give you the best possible outcome while honoring what matters most in your life. It’s the first step toward taking back control.
Navigating the Next Steps After Your Visit
Your first visit doesn't really end when you leave our office. In many ways, that’s when the next chapter begins. The last part of our conversation is dedicated to creating a clear, actionable plan so you walk out the door with a roadmap, not more confusion.
We shift from talking about the “what” and “why” of your diagnosis to the “how” and “when” of your treatment. This is all about logistics—turning our discussion into a concrete schedule and making sure your path forward is as smooth as possible.
Setting Your Treatment Timeline in Motion
Once we've settled on a treatment plan together, the next step is getting it on the calendar. This doesn't happen instantly; there's a lot of careful coordination that our team handles behind the scenes to get everything lined up perfectly for you.
Here’s what that logistical phase usually looks like:
- Insurance Authorization: We immediately get to work on obtaining prior authorization from your insurance provider. This is a mandatory green light we need before starting treatments like chemotherapy or immunotherapy.
- Scheduling Your First Infusion: As soon as we have all the medical and administrative clearances, we'll schedule your first treatment session and give you a specific date and time.
- Coordinating Additional Tests: If your plan requires any other scans or specific blood work before you can start, we'll get those appointments booked for you right away.
You won't leave empty-handed. We'll give you a clear sense of the expected timeline and the name of a direct contact on our team you can call with any scheduling questions that pop up.
What to Expect at Your First Infusion Appointment
Walking in for your first treatment can bring on a whole mix of feelings, and that’s completely normal. Knowing what the day will look like can make a world of difference. These appointments are very different from your initial consultation; they are entirely focused on delivering your treatment safely and keeping you comfortable.
A typical infusion visit moves through a few key stages:
- Check-In and Vitals: You'll start with a simple check-in at the front desk. Then, a nurse will take your vital signs (like blood pressure and temperature) and your weight.
- Blood Work: In most cases, we'll draw a small blood sample to check your cell counts. This is a critical safety check to make sure your body is ready for treatment that day.
- Meeting with Your Oncologist: Dr. Hirschfeld will sit down with you to go over your lab results, check in on how you're feeling, and answer any last-minute questions before giving the final okay to proceed.
- Receiving Your Infusion: From there, you'll get settled in a comfortable chair in our infusion suite. One of our specialized oncology nurses will take it from there, expertly administering your medication.
The infusion itself can last anywhere from 30 minutes to several hours, depending on your specific treatment. Our team is right there with you the whole time, monitoring everything and making sure you have what you need.
Supportive care isn't an afterthought; it's a core component of your treatment plan. We actively manage side effects to help you maintain strength, comfort, and a high quality of life throughout your journey.
This proactive approach is key to helping you tolerate treatment as well as possible.
Supportive Care and Managing Symptoms
Modern cancer care is as much about managing the treatment as it is about fighting the cancer itself. We build your supportive care plan right alongside your medical one, aiming to get ahead of potential side effects before they become a problem.
We'll connect you with resources for everything from nutritional guidance to managing fatigue or nausea. Our goal is to treat you as a whole person, not just a diagnosis. By weaving symptom management into your care from day one, we help you navigate this process with far more comfort and resilience.
Answering Your Lingering Questions
No matter how much you prepare, it's completely normal for a few worries to pop up as your first oncology appointment gets closer. We find that many of our patients have the same questions, but sometimes they feel hesitant to ask them. We want to tackle those concerns head-on right here.
Think of this as one last conversation to help quiet your mind and make sure you feel as comfortable as possible before you even walk through our doors.
Is It Normal to Feel Totally Overwhelmed and Forget My Questions?
Yes, absolutely. In fact, it might be the single most common feeling people have during their first visit. You’re being asked to process a huge amount of new, deeply personal information, all at once. It’s no wonder your mind might feel flooded, making it hard to remember the questions you so carefully wrote down.
This is precisely why we can't stress this enough: bring a trusted friend or family member with you. They can be your second set of ears and your designated note-taker. They’re the person who can gently jump in and say, “Didn’t you want to ask about the side effects?” Having them there takes the pressure off, allowing you to just focus on the conversation.
Feeling overwhelmed isn't a sign of weakness—it's a sign that you're human. We expect it, and our team is here to guide you through it with all the patience in the world.
And even with a helper, you might get home and a question you forgot will suddenly pop into your head. That’s okay, too. The conversation doesn't end when you leave our office. You can always call our team or send a secure message through the patient portal. No question is ever too small.
Will I Have to Start Treatment on the Very First Day?
It’s extremely rare for anyone to start active treatment—like an infusion—on the same day as their first consultation. That initial appointment is all about something just as critical: gathering information, doing a thorough evaluation, and building your personalized game plan together. It's the strategic huddle before the game begins.
Before any treatment can actually start, a few important things need to happen behind the scenes:
- Finalizing the Plan: Dr. Hirschfeld needs time to put all the pieces together—your records, the exam, imaging results, and your personal goals for treatment.
- Insurance Authorization: Most advanced cancer treatments require prior authorization from your insurance company. This can take a little time, and our administrative team handles all of it for you.
- Scheduling and Prep: Sometimes we need to schedule a few more preparatory tests or line things up with other specialists before your first infusion.
You will leave your first visit with a clear roadmap of what comes next. We’ll give you a realistic timeline for when treatment will likely start, including a scheduled date for your first session, so you are never left in the dark.
What’s the Role of My Caregiver During This First Visit?
Your caregiver—whether it's your spouse, a sibling, or a close friend—plays a huge, active role during this first appointment. Their job goes way beyond just offering a hand to hold. They are a key part of the team.
We see their role breaking down into three important jobs:
- The Scribe: They can take detailed notes on everything, from how the diagnosis is explained to the proposed treatment schedule. This frees you up to simply listen, absorb, and ask what’s on your mind.
- The Second Listener: With so much complex information being discussed, having a second person hearing it all is invaluable. They often catch details you might miss while you’re processing the bigger picture.
- The Advocate: In the moment, it can be hard to speak up for yourself. The person who knows you best can help voice questions or concerns you might forget or feel too shy to bring up.
We truly see caregivers as an extension of your support system and a valued partner in your care. We welcome them to jump in, ask their own questions, and be fully engaged. Their involvement from day one helps build a much stronger foundation for the road ahead.
At Hirschfeld Oncology, we know your first appointment is a major step. Our entire team is dedicated to giving you the time, information, and compassionate support you need to face your diagnosis with confidence. To learn more or to schedule a consultation, please explore our patient resources.





.png)


.png)
.png)




