When we talk about treating prostate cancer, one of the most precise and effective tools in our arsenal is a type of internal radiation called brachytherapy. Think of it as an "inside-out" approach. Instead of sending radiation beams from outside the body, we place the radiation source directly inside or right next to the tumor.
This method allows us to deliver a very high, targeted dose of radiation to the cancer cells while doing a much better job of protecting nearby healthy tissues, like the bladder and rectum. It’s an incredibly effective treatment, especially for cancer that hasn't spread beyond the prostate gland.
A Targeted Approach to Treating Prostate Cancer

Here’s an analogy I often use with my patients: imagine you have a few stubborn weeds in a prized flowerbed. You could use a wide-spray weed killer that hits everything—the flowers, the good soil, and the weeds. Or, you could carefully place a tiny, potent treatment directly at the root of each weed. Brachytherapy for prostate cancer is like that second, more precise method. It avoids the broad-spray approach of external radiation and concentrates its power exactly where it needs to be.
This technique has become a pillar of modern radiation oncology for a reason: it offers excellent long-term success. For many men with localized disease, the cure rates are right on par with those of major surgery (radical prostatectomy), but the recovery and side effect profile can be very different.
How Brachytherapy Works
At its core, the procedure involves placing tiny radioactive sources—we often call them "seeds"—inside the prostate gland. These seeds give off radiation over a very short distance, which means a high dose can saturate the tumor cells. Because the radiation doesn't have to travel through healthy organs to get to the prostate, the risk of collateral damage is significantly lower.
This precision is what helps us preserve a man's quality of life. The main goals are simple but powerful:
- Deliver a potent, curative dose of radiation right to the tumor.
- Minimize radiation hitting the bladder and rectum to reduce side effects.
- Provide a much shorter overall treatment course compared to traditional external beam radiation therapy.
This treatment is a testament to medical precision. By focusing radiation internally, we can often increase the dose to the tumor significantly while simultaneously decreasing exposure to critical organs like the rectum by 30-50%, a crucial factor in maintaining long-term function and well-being.
My goal with this guide is to give you a clear, straightforward overview of this treatment from a patient's perspective. We’ll break down the different types, talk about who makes a good candidate, and walk through what you can expect before, during, and after the procedure. It's all about giving you the knowledge to have a confident, informed conversation with your care team.
Understanding LDR and HDR Brachytherapy

While all brachytherapy for prostate cancer works from the inside out, it comes in two distinct forms. Think of it like this: you can either slowly nourish a plant over time or give it a few quick, potent doses of nutrients. Both can get the job done, but the strategy is completely different.
The two main types are Low-Dose-Rate (LDR) and High-Dose-Rate (HDR) brachytherapy. Getting a feel for how they differ is the first step in understanding which path might be the right one for your specific diagnosis.
LDR Brachytherapy: The Slow-Release Method
LDR brachytherapy is the most common form, often called a "seed implant." In a single outpatient procedure, we permanently place dozens of tiny radioactive seeds—each about the size of a grain of rice—directly into your prostate gland.
You can think of these seeds as tiny, slow-release capsules of medicine. They don't deliver their full dose at once. Instead, they emit a low, steady stream of radiation over several months, which is incredibly effective at destroying cancer cells from within.
Because the radiation only travels a few millimeters, this approach is excellent at protecting nearby healthy tissues like the bladder and rectum. The seeds do their work and gradually become inert over about a year, remaining safely in place for life.
LDR brachytherapy is often an ideal choice for men with:
- Lower-risk cancer that is well-contained within the prostate.
- A preference for a one-and-done procedure, avoiding daily trips for treatment.
- The desire for a powerful, standalone therapy that gets the job done with minimal disruption to their daily routine after a brief recovery.
HDR Brachytherapy: The High-Intensity Approach
Now, let's look at the other side of the coin: HDR brachytherapy. This technique operates on a completely different principle and timeline. Instead of leaving permanent seeds, we temporarily place a single, highly powerful radioactive source inside the prostate for a very short time.
With HDR, we first insert thin, hollow catheters into the prostate under anesthesia. A computer-guided machine then sends the tiny, potent radiation source through each catheter for just a few minutes. After the treatment is complete, we remove both the source and the catheters. Nothing is left behind in your body.
With HDR brachytherapy, we have exceptional control. By adjusting how long the radiation source stays in different positions, we can shape the dose with incredible precision, effectively "painting" the radiation onto the tumor while sculpting it away from the rectum and urethra. This level of dose control is one of HDR's greatest strengths.
Because the dose is so high, the treatment sessions are very brief. An entire course of HDR therapy typically involves just 1 to 4 sessions scheduled over a couple of days or weeks.
This powerful approach is often used in two key situations:
- As a "boost" for more aggressive cancers: We frequently combine HDR with a shorter course of external beam radiation to deliver a knockout punch to the tumor.
- As a standalone treatment (monotherapy): For certain men with intermediate-risk cancer, a few HDR sessions can serve as the entire course of radiation therapy.
Comparing LDR and HDR Brachytherapy at a Glance
To make sense of these two powerful tools, it helps to see them side-by-side. Both LDR and HDR are excellent treatments, but they are designed for different clinical scenarios. The right choice for you will depend on your cancer’s specific characteristics, your prostate anatomy, and your personal treatment goals.
This table breaks down the key differences to help clarify how each approach works.
Ultimately, whether LDR, HDR, or a combination approach is recommended is a decision that comes after a thorough evaluation and a detailed discussion between you and your radiation oncology team.
Who Is a Good Candidate for Brachytherapy?
Figuring out if brachytherapy is the right path for you is a highly personal decision, made hand-in-hand with your oncology team. It’s a fantastic treatment, but it’s not a one-size-fits-all solution for every man diagnosed with prostate cancer. The whole idea is to match your specific cancer, your anatomy, and your overall health to what this therapy does best.
First and foremost, brachytherapy for prostate cancer shines when the cancer is still confined to the prostate gland. That's the critical starting point. If scans show the cancer has already spread to distant places, like the bones, our focus shifts to other treatments that can address cancer throughout the body. We go into more detail about how we check for this in our guide on the bone scan for prostate cancer.
Key Clinical Factors We Look At
Once we've confirmed the cancer is localized, we zoom in on a few key numbers from your diagnostic reports. Think of these as the vital stats that give us a clear picture of the cancer's personality—how aggressive it is and how it’s likely to behave. This is what truly guides the conversation.
We primarily focus on three things:
- Prostate-Specific Antigen (PSA) Level: This is a simple blood test. For a man to be a strong candidate, especially for a seed implant alone, we generally like to see a PSA level less than 10 ng/mL.
- Gleason Score: This comes from your biopsy and tells us how aggressive the cancer cells look under a microscope. A Gleason score of 6 or 7 is often the sweet spot for brachytherapy.
- Tumor Stage: This is the clinical assessment of the tumor's size and if it’s breaking out of the prostate. The best candidates have early-stage disease (like T1c or T2a), where everything is neatly contained inside the prostate capsule.
So, who’s the textbook candidate? It's often a man with low- or favorable intermediate-risk prostate cancer. That usually translates to a Gleason score of 6, a PSA under 10, and a tumor that's not big enough to be felt during a rectal exam.
When these factors line up, it tells us the cancer is serious enough to warrant treatment but hasn't started venturing out. That makes it a perfect target for the precise, focused radiation of brachytherapy.
When Brachytherapy Might Not Be the Best Fit
Just as important as knowing who’s a great fit is understanding when another approach might be better. Sometimes, a man’s specific anatomy or health history can make the procedure tricky or raise the risk of side effects down the line.
We might steer you toward a different treatment if you have one of these conditions:
- A Very Large Prostate Gland: If the prostate is simply too big, it becomes a real challenge to get the radioactive seeds placed perfectly. You can end up with cold spots that don't get enough radiation or hot spots that cause more side effects. Sometimes, we can use hormone therapy for a few months to shrink the prostate first.
- Significant Pre-Existing Urinary Symptoms: If you’re already getting up multiple times a night or have trouble with a weak stream (often from BPH), the temporary swelling from brachytherapy can make those problems much worse. We need to be careful not to trade one problem for another.
- Previous Prostate Surgery: If you've had a procedure like a TURP for an enlarged prostate, the anatomy is changed. This can make seed placement much more difficult and, frankly, it raises the risk of urinary incontinence.
In the end, this is a collaborative decision. A good, long talk with your radiation oncologist is essential to weigh all these factors. The goal is always the same: to choose the treatment that gives you the best shot at a cure while preserving your quality of life.
The Brachytherapy Procedure Step-by-Step
Knowing what’s coming can make any medical procedure feel less intimidating. Prostate brachytherapy is a highly methodical process, and your care team will be there to guide you every step of the way. Let's walk through the entire timeline, from the initial planning to the day of treatment itself, so you have a clear picture of what to expect.
It all starts with a detailed planning phase. Think of it as creating a custom architectural blueprint for your treatment. Before any radioactive sources are placed, your team needs to map out your prostate gland with incredible precision. This ensures the radiation dose covers the entire tumor while carefully avoiding healthy surrounding tissue.
Creating Your Personalized Treatment Map
This critical mapping is done using advanced imaging. A few weeks before the procedure, you'll come in for a specialized ultrasound, CT scan, or MRI. This scan generates a detailed 3D model of your prostate, which becomes the roadmap for your radiation oncologist and physicist.
With this model, they run sophisticated computer simulations to figure out the exact number of radioactive seeds (for LDR) or catheter positions (for HDR) you'll need. The goal is to calculate the perfect placement pattern—a grid that delivers a powerful, curative dose of radiation that conforms precisely to the unique shape of your gland. This meticulous pre-planning is truly the key to the treatment's success.
The flowchart below shows how we use key diagnostic factors—like whether the cancer is localized, your PSA levels, and your Gleason score—to determine if you're a good candidate for this carefully planned procedure.
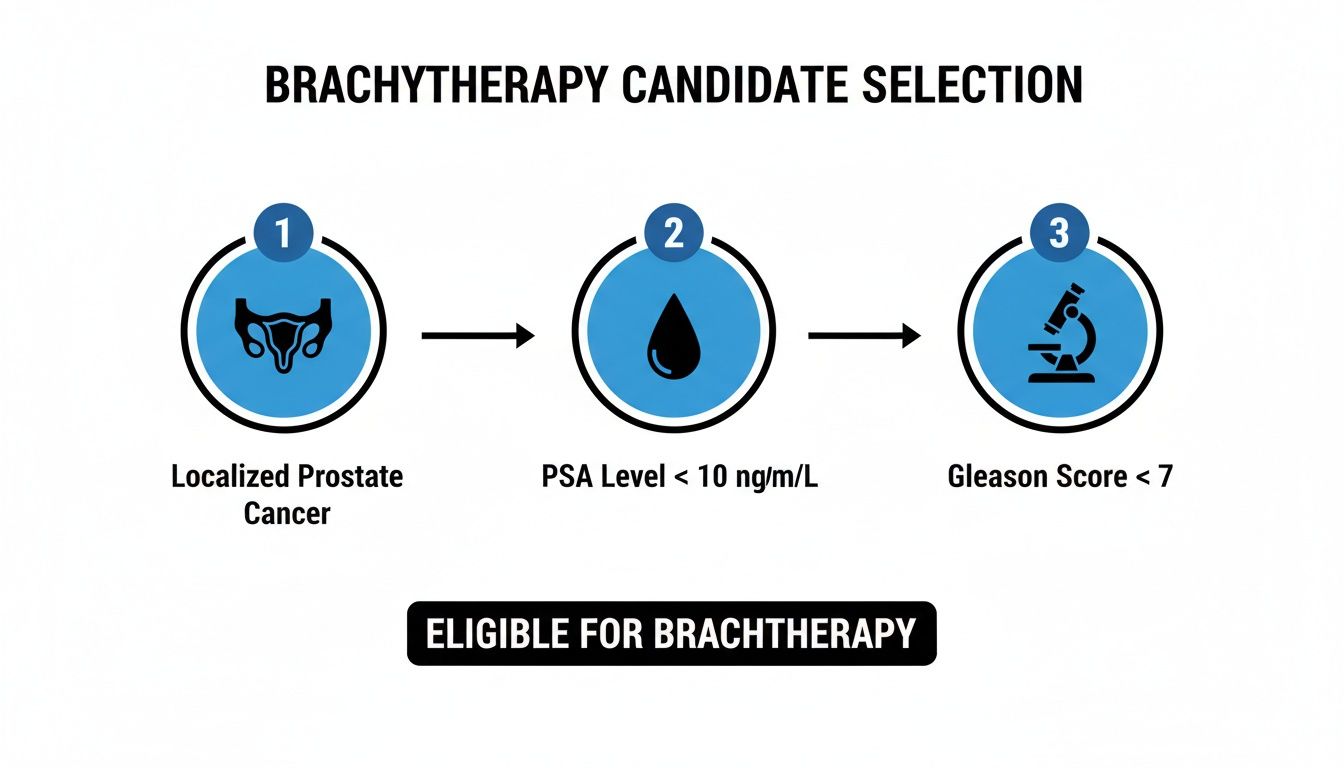
As the graphic illustrates, brachytherapy is most effective when all the data points to a cancer that is still contained within the prostate itself.
What Happens on Procedure Day
On the day of your brachytherapy, you’ll be brought into a specialized operating suite. We perform the procedure under either general or spinal anesthesia, so you’ll be comfortable and won't feel any pain.
Once the anesthesia takes effect, your radiation oncologist will use a transrectal ultrasound probe to get a live, real-time view of your prostate. This image allows them to see exactly where they are guiding the treatment needles, which are inserted through the perineum (the small area of skin between the scrotum and anus).
This isn't a "blind" procedure. Every single step is guided by live imaging to ensure each seed or catheter is placed exactly according to the detailed map we created during your planning session. This visual confirmation is what makes the treatment so safe and accurate.
To guarantee this accuracy, the team often uses real-time imaging techniques like fluoroscopy. It works like a live X-ray movie, confirming that every element is positioned perfectly before we proceed.
- For LDR Brachytherapy: The needles are used to deposit the tiny radioactive seeds, one by one, into the prostate according to that pre-planned grid. The entire procedure is surprisingly quick, usually taking about one hour.
- For HDR Brachytherapy: In this case, the needles are actually hollow catheters. Once they're in position, we connect them to a machine that sends a single, high-activity radiation source into each catheter for a few minutes before retracting it.
After the Procedure and Initial Recovery
Once the treatment is complete, the needles are removed, and you’ll be moved to a recovery area to rest. Most men go home the very same day. It's normal to feel some soreness, bruising, and swelling in the perineal area, but this is easily managed with mild pain relievers.
Your team will give you specific instructions on how to manage any temporary urinary symptoms, like needing to go more often or having a slower stream. These are common as the prostate heals from the procedure.
The precision and effectiveness of this treatment have fueled its growth as a preferred option for many men. The prostate brachytherapy market, valued at USD 367.5 million in 2025, is projected to hit USD 654.4 million by 2033, driven by its excellent outcomes and patient-friendly approach.
Weighing the Pros, Cons, and Potential Side Effects
Every treatment decision is a balance. It's about carefully considering the potential upsides against the possible challenges. When it comes to brachytherapy for prostate cancer, having a clear and honest view of both sides is essential. This treatment packs a powerful punch, especially for men with localized disease, but like any medical procedure, it has potential side effects you need to understand.
The biggest advantage of brachytherapy is its incredible precision. By placing the radiation source right inside the prostate, we can deliver a potent, cancer-killing dose that’s highly focused on the tumor. This "inside-out" strategy is fantastic at protecting the healthy organs that sit right next door—namely, the bladder and the rectum.
The Major Benefits of Brachytherapy
For many men, one of the most attractive benefits is the short-and-sweet treatment timeline. Traditional external beam radiation often means daily trips to the hospital for seven to nine weeks. Brachytherapy is a world apart. An LDR seed implant is a one-and-done procedure, and an HDR course is typically just a handful of sessions.
This targeted approach leads to excellent clinical results. Brachytherapy really shines in a few key areas:
- High Cure Rates: For men with low- or intermediate-risk prostate cancer, long-term success rates are outstanding—right on par with what we see from radical prostatectomy (surgery).
- Convenience: The treatment is over quickly, letting you get back to your normal life with minimal disruption.
- Reduced Collateral Damage: By concentrating the radiation internally, we drastically limit the dose to surrounding tissues, which is crucial for preserving your long-term function.
The precision of brachytherapy gives us a distinct edge. We can deliver a much higher radiation dose to the tumor while simultaneously shielding sensitive areas. For example, some advanced techniques allow us to boost the tumor dose by up to 145% while cutting rectal exposure by 30-50%. That’s a huge factor in minimizing bowel-related side effects. The effectiveness of this approach is one reason why brachytherapy continues to be a leading treatment, a trend noted by industry analysts at Mordor Intelligence.
Understanding the Short-Term Side Effects
After the procedure, it’s normal to have some temporary side effects as your body heals. They’re usually most noticeable in the first few weeks or months and then slowly get better. Think of it as your body's reaction to both the procedure and the initial work of the radiation.
You might experience:
- Urinary Symptoms: This is the most common one. You may feel a stronger urge to urinate, need to go more often (especially at night), or notice a weaker stream.
- Discomfort or Bruising: Some soreness or bruising in the perineal area (the spot between the scrotum and anus) is normal. This usually clears up in a week or two.
- Minor Rectal Irritation: A few men might experience temporary bowel frequency or a sense of urgency, but this is less common.
These short-term effects are an expected part of the healing process. Your care team will be right there with you, providing medications and strategies to manage everything and keep you comfortable as you recover.
It's helpful to think of these initial side effects as a sign that the treatment is working. The temporary inflammation is just a response to the powerful, targeted radiation doing its job to wipe out cancer cells. The vast majority of these issues fade significantly over time.
What About Long-Term Side Effects?
While most side effects don't stick around, it’s just as important to talk about the potential for long-term changes. The entire goal of your oncology team is to minimize these risks through meticulous planning and precise execution.
The two main long-term considerations are erectile function and bowel health. The nerves and blood vessels controlling erections run right alongside the prostate, as does the rectum. Even though brachytherapy is specifically designed to spare these structures, some men may experience changes over time.
The risk of long-term erectile dysfunction (ED) after brachytherapy varies a lot, depending on your function before treatment, your age, and other health factors. Many men preserve their function just fine, while others may need medications or other therapies for support. In the same vein, while it’s rare, a small percentage of men may have lasting changes in their bowel habits. We take a broader look at how different radiation treatments can impact the body in our guide on the general effects of radiation therapy.
Your doctor will have a very open conversation with you about these risks, tailored to your specific case. This ensures you can make a fully informed decision that aligns with your personal priorities for both cancer control and your quality of life.
Life After Brachytherapy Recovery and Follow Up Care
Finishing your brachytherapy procedure is a huge step, but it's not the end of the road. The next phase is all about healing, monitoring your progress, and getting back to your life. Think of it as a partnership between you and your oncology team, focused on ensuring the best possible long-term outcome.
Right after the procedure, it's normal to experience some temporary side effects as your body heals. You might notice you need to urinate more frequently or with more urgency, but this almost always gets better within a few weeks. Most men are back to light activities and desk work in just a couple of days, though we'll ask you to hold off on heavy lifting or strenuous exercise for at least two to three weeks.
Managing Your Recovery at Home
We'll send you home with a detailed set of personal instructions, but a few general tips can make the initial recovery period much smoother. Drinking plenty of water helps keep your urinary system clear, and simple over-the-counter anti-inflammatory medication is usually all that’s needed for any discomfort.
If you had the permanent LDR seeds, you’ll need to follow a few straightforward, temporary safety precautions. It’s important to remember that the radiation from these seeds is very low-energy and doesn't travel far—just a few millimeters.
- Small children and pregnant women: For the first two months, it’s best to avoid holding small children directly on your lap or having very close, prolonged contact with anyone who is pregnant. This is purely a precaution.
- Other adults: You can carry on as usual with other adults. There's no risk to them, so you don't need to sleep in a separate bed, use different bathrooms, or wash your clothes separately.
The Importance of Long-Term Follow Up
Your follow-up care is where we confirm the treatment’s success and safeguard your health for the future. The most important tool we have for this is a simple blood test that measures your Prostate-Specific Antigen (PSA).
After brachytherapy, your PSA level is the key metric we watch. We expect it to drop steadily over time, eventually reaching a very low and stable point called the "PSA nadir." This gradual decline, which can take a year or more, is a fantastic sign that the treatment worked exactly as planned.
We’ll map out a clear follow-up schedule for you, which generally looks like this:
- First Year: PSA tests every 3 to 4 months.
- Years Two and Three: PSA tests every 6 months.
- Beyond Three Years: Annual PSA tests are usually sufficient.
This regular monitoring allows us to track your progress with precision and catch any potential issues early. It’s this diligent follow-up that helps secure the excellent long-term results brachytherapy is known for. In fact, studies show that for men with low-risk disease, the rate of biochemical recurrence-free survival can be 90% or higher ten years later, often with erectile function well-preserved. You can find more statistics on the effectiveness of prostate brachytherapy on grandviewresearch.com. Sticking to this follow-up plan is the most important thing you can do for your continued health.
Common Questions About Prostate Brachytherapy
Thinking about a new treatment like brachytherapy naturally brings up a lot of questions. Getting clear, straightforward answers is one of the most important steps in feeling confident about your decision. Let’s walk through some of the things our patients ask most often.
Is the Brachytherapy Procedure Painful?
No, you won't feel anything during the actual procedure. We always perform it under either general or spinal anesthesia, so your comfort is completely managed.
Afterward, it's normal to have some temporary soreness, bruising, or swelling in the perineum (the area between the scrotum and anus). This is usually mild and easily handled with standard over-the-counter pain relievers. Most men find they can return to light activities and desk work within just a few days.
Will I Be Radioactive After LDR Brachytherapy?
This is a very common and understandable concern. With Low-Dose-Rate (LDR) brachytherapy, the permanent seeds do emit a very low level of radiation for a few months. But here’s the key: that radiation is almost entirely contained right within your prostate.
It’s powerful where it needs to be, but it doesn't travel far. For this reason, it poses no real risk to others. As a simple precaution, we'll advise you to avoid prolonged close contact with young children and pregnant women for about two months—this just means not having a small child sit on your lap for long periods. Everyday interactions with family, friends, and coworkers are perfectly safe.
Think of the radiation from LDR seeds like a tiny, self-contained lightbulb. It's bright enough to illuminate the immediate area (your prostate), but its light is too weak to travel very far outside your body.
How Does Brachytherapy Compare to Surgery?
When it comes to treating localized prostate cancer, both brachytherapy and a radical prostatectomy (surgery) have excellent and very similar long-term cure rates. The best path for you often depends on your personal priorities regarding potential side effects and recovery.
Here’s a quick rundown of the main differences:
- Urinary Incontinence: Surgery carries a higher risk of long-term urinary leakage.
- Urinary Irritation: Brachytherapy is more likely to cause temporary urinary or bowel irritation, which almost always resolves over time.
- Recovery: The recovery from brachytherapy is significantly faster and less demanding than what follows major surgery.
An open, honest conversation with your entire care team is the best way to weigh these factors and see which approach fits your life and goals.
Can I Have Other Treatments if Cancer Returns Later?
Absolutely. A good treatment plan always keeps future options on the table. Choosing brachytherapy now does not typically close the door to other effective treatments if the cancer were to come back down the road.
Should you ever need it, future treatments could include hormone therapy, external beam radiation, or other targeted therapies. We'll monitor you closely with regular PSA tests to catch any hint of a recurrence early, ensuring you always have access to the full spectrum of care. Part of that long-term planning can also involve exploring new treatments, which you can learn about in our guide to clinical trials for prostate cancer.
At Hirschfeld Oncology, we believe that clear communication is the foundation of excellent cancer care. If you have more questions about your diagnosis or potential treatment paths, our team is here to provide the detailed, compassionate answers you deserve. Visit our blog to learn more.





.png)


.png)
.png)




