A diagnosis of stage 4 breast cancer is a heavy, life-changing moment. It’s natural to feel overwhelmed by uncertainty and fear. When you hear "stage 4," it simply means that cancer cells that started in the breast have traveled to other, more distant parts of the body.
This is the most advanced stage, yes, but it’s crucial to know that it is absolutely treatable. For many people, it becomes a chronic condition they live with and manage for years.
What a Stage 4 Breast Cancer Diagnosis Really Means

When an oncologist confirms a diagnosis of stage 4 breast cancer—often called metastatic breast cancer—it changes the entire conversation around treatment and management. The key difference between this stage and earlier ones isn't about the size of the original tumor; it’s about where the cancer cells are now. They are no longer just in the breast or nearby lymph nodes.
I often use an analogy of a dandelion in a garden. In the early stages, the dandelion is just one plant in one spot. But when the wind catches its seeds, they can float across the yard and start new plants far away. In stage 4, cancer cells act like those seeds, traveling through the bloodstream or lymphatic system to form new tumors in distant organs.
Key Characteristics of Stage 4 Cancer
Getting a handle on what this diagnosis truly means can help you feel more in control and better prepared for discussions with your care team. Here’s what it boils down to:
- Metastasis is the defining feature. The cancer has spread to distant places, most often the bones, lungs, liver, or brain.
- It’s still breast cancer. This is a critical point. Even if a new tumor is found in your liver, it's made of breast cancer cells and will be treated with breast cancer therapies.
- The treatment goal shifts. Because the cancer is widespread, the goal isn't a one-time cure. Instead, the focus shifts to controlling the cancer's growth, managing symptoms, and preserving your quality of life for as long as possible.
This table gives a quick summary of what a Stage 4 diagnosis means in practical terms.
Stage 4 Breast Cancer At A Glance
This move toward long-term management is one of the most important concepts to grasp. Modern oncology, especially at patient-first practices like Hirschfeld Oncology, treats stage 4 breast cancer as a manageable chronic disease, not an immediate crisis.
A diagnosis of metastatic breast cancer is not the end of the story. Instead, it marks the beginning of a new chapter—one focused on managing the disease with advanced therapies, hope, and a dedicated care team committed to your well-being.
In the United States, more than 168,000 people are currently living with metastatic breast cancer. This number is a testament to both the reality of the disease and the incredible progress we've made in treatments that help people live longer, fuller lives. You can learn more about these breast cancer facts and figures to understand the bigger picture.
How Doctors Confirm a Stage 4 Diagnosis

Pinpointing a stage 4 breast cancer diagnosis isn't a single event but a careful process of gathering evidence. Your oncology team acts like investigators, using a combination of sophisticated imaging, blood work, and tissue analysis to build a complete and accurate picture of what’s happening inside your body.
This process is absolutely vital. It tells us exactly where the cancer has traveled and, just as importantly, what makes it tick. This detailed understanding is the foundation for creating a treatment plan that's precisely aimed at your specific cancer.
The diagnostic journey usually starts when new symptoms arise that might suggest the cancer has spread, or sometimes during routine follow-up care after an earlier diagnosis.
Creating a Map with Imaging Scans
The first step is almost always to get a clear visual of the situation. Think of imaging scans as your body’s internal GPS, creating a detailed map that highlights any areas of concern. Your doctor will select the right tools for the job based on your specific situation.
These powerful technologies give us different views of what's going on:
- CT (Computed Tomography) Scan: Using a series of X-rays, a CT scan creates detailed, cross-sectional pictures of your organs and tissues. It’s incredibly useful for spotting potential tumors in the chest, abdomen, and pelvis.
- PET (Positron Emission Tomography) Scan: A PET scan is different—it looks for activity. Cancer cells are busy and consume a lot of energy, so they "light up" on a PET scan, showing us where the most metabolically active spots are.
- MRI (Magnetic Resonance Imaging): An MRI uses powerful magnets instead of radiation to create remarkably clear images of soft tissues. This makes it the go-to scan for getting a detailed look at the brain and spinal cord.
- Bone Scan: This scan is designed for one purpose: to find cancer that has moved into the skeleton. A safe, radioactive tracer is injected, and it naturally gathers in areas of high bone activity, which can signal the presence of metastases.
Each scan tells a part of the story. If you're curious about the specifics, you can explore the key differences between CT scans and MRIs in our guide.
The Importance of a Biopsy
Imaging can show us where a suspicious spot is, but it can’t tell us for sure what it is. To get that definitive answer, a biopsy is essential. This procedure involves taking a very small tissue sample from one of the suspected new tumors.
A biopsy is critical for two main reasons. First, it confirms beyond a doubt that the cells in the new location are, in fact, breast cancer. Second, and perhaps most importantly, that tiny piece of tissue holds the genetic keys to your cancer.
Unlocking the Cancer's Genetic Code
The tissue sample from the biopsy is sent to a specialized lab for what we call biomarker testing. This is where we learn the unique "personality" of your cancer, which is the single most important factor in choosing the right treatment.
Understanding your cancer’s biomarkers is like finding the right key for a specific lock. It allows your care team to move beyond general treatments and select therapies designed to target your cancer's specific vulnerabilities.
We analyze the tissue for a few key things:
- Hormone Receptors (ER/PR): We check if the cancer cells have receptors for estrogen (ER-positive) and progesterone (PR-positive). If they do, it means these hormones are fueling the cancer's growth, which opens the door to highly effective hormone-blocking therapies.
- HER2 Status: This test looks for a protein called HER2. If the cells are making too much of this protein (HER2-positive), the cancer can be more aggressive. The good news is that we have incredible drugs that specifically target the HER2 protein.
If the cancer cells don't have any of these three receptors, we classify it as triple-negative breast cancer. Knowing these molecular details isn't just a technicality—it is the cornerstone of the personalized, effective treatment strategy we build for you at Hirschfeld Oncology.
Making Sense of Prognosis and Survival Rates
Let's talk about one of the toughest parts of a stage 4 diagnosis: the numbers. When you see statistics about prognosis and survival, they can feel cold, impersonal, and frankly, terrifying. It's crucial to understand what those numbers really mean—and, more importantly, what they don't mean for you.
Survival rates, like the 5-year survival rate you often see quoted, are just broad averages. They're calculated from data on thousands of people, collected over many years. Think of it like a weather forecast for an entire state. It might predict a 30% chance of rain, but it can’t tell you for sure if a single drop will fall on your house.
These numbers are also a look in the rearview mirror. They reflect the outcomes of treatments from years ago, not the breakthroughs that became available last month. Your journey is not a statistic; it's your own story, and it’s still being written.
Looking Beyond the Averages
While statistics paint a wide-angle picture, your personal prognosis is built from a very specific set of details. Your oncology team isn't looking at those broad averages; they are focused entirely on the unique biology of your cancer and your individual health.
This is what creates a much clearer picture of your outlook:
- Your Cancer's Subtype: Is it fueled by hormones (ER/PR-positive)? Does it overproduce the HER2 protein (HER2-positive)? Or is it triple-negative? Each type acts differently and responds to different therapies.
- Where the Cancer Has Spread: Metastasis to the bones often carries a different outlook than spread to major organs like the liver or brain.
- Your Overall Health: Your age, fitness level, and any other health conditions play a huge role in determining the best treatment plan for you.
- Response to Treatment: How well the cancer responds to the first round of therapy is one of the most important indicators. A good initial response is always a very encouraging sign.
Your prognosis isn't a destiny set in stone by old data. It’s a dynamic path that changes based on your cancer’s biology, your health, and the incredible pace of medical science.
The reality of metastatic disease is serious. Stage 4 breast cancer is a significant contributor to the projected 42,140 breast cancer deaths among U.S. women in 2026. And while overall breast cancer death rates have dropped dramatically since 1989 thanks to better screening and treatments, stage 4 cases remain the most challenging. For a deeper dive into these trends, you can explore more detailed breast cancer statistics.
A New Goal for Stage 4 Breast Cancer
This brings us to a fundamental shift in how we approach stage 4 breast cancer today. The primary goal is no longer a one-time "cure" but something more sustainable: turning an aggressive disease into a manageable, chronic condition.
We aim to control the cancer's growth, relieve symptoms, and protect your quality of life for as long as possible. Many people now live for years—sometimes even decades—with metastatic breast cancer, managing it with ongoing treatment much like someone would for diabetes or heart disease. At Hirschfeld Oncology, this is the philosophy that guides every single treatment plan, focusing on you as a whole person, not just a diagnosis.
Modern Treatments For Stage 4 Breast Cancer
When we talk about treating stage 4 breast cancer today, the conversation is fundamentally different than it was a decade ago. We've moved past a one-size-fits-all approach and into an era of highly personalized medicine. The goal is no longer just about fighting the cancer, but managing it as a long-term, chronic condition, with a sharp focus on preserving your quality of life.
This evolution comes from a much deeper understanding of the biology behind cancer. We can now pinpoint the specific drivers of different breast cancers, which lets us use smarter, more precise therapies. Instead of relying solely on broad-spectrum chemotherapy, we can select treatments that outmaneuver cancer cells while minimizing the impact on your day-to-day life.
The Pillars Of Modern Systemic Therapy
Systemic therapies are the foundation of managing metastatic breast cancer. These are treatments that travel through your entire body, hunting down and fighting cancer cells wherever they've spread. The options available today are more sophisticated and varied than ever.
- Hormonal (Endocrine) Therapy: For the nearly 70% of patients whose cancer is hormone receptor-positive (ER+ or PR+), this is often the first line of defense. These treatments work by cutting off the estrogen supply that these specific cancer cells need to grow and thrive.
- Targeted Therapy: Think of these drugs as sharpshooters. They are designed to identify and attack specific proteins or pathways that cancer cells rely on to multiply. They are frequently paired with hormonal therapy or chemotherapy to boost their overall effectiveness.
- Immunotherapy: This is an exciting approach that essentially unleashes your own immune system to fight cancer. Certain drugs can "unmask" cancer cells, making them visible to your body's natural defenses, which can then recognize and destroy them.
- Chemotherapy: While it remains a vital tool, chemotherapy is used much more strategically now. Innovative methods, like the metronomic (low-dose) chemotherapy we often use at Hirschfeld Oncology, deliver a continuous, low-level dose. This approach aims to halt cancer growth without the severe side effects, making it a sustainable option for long-term management.
Every treatment decision is guided by a combination of factors, including your specific cancer subtype, where it has spread, and how it responds to different therapies. This ensures the plan is tailored directly to you.
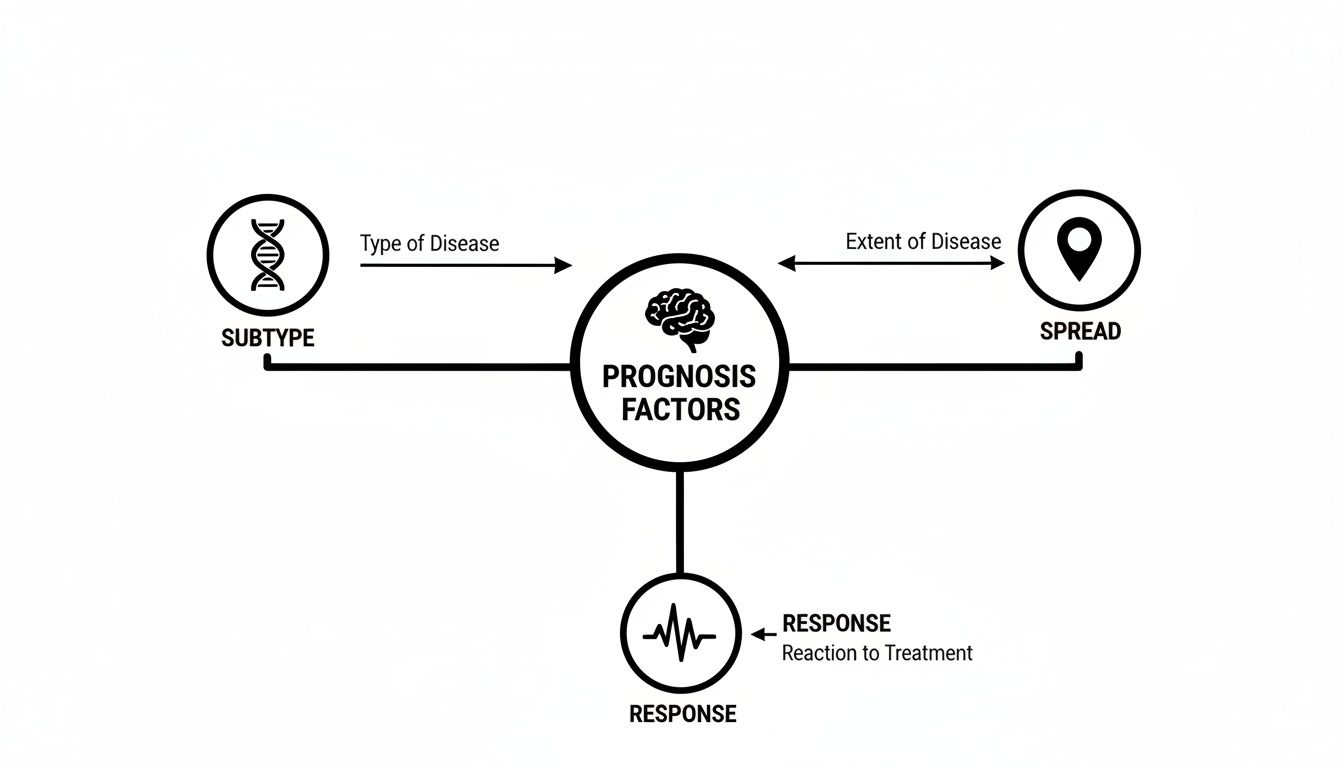
This diagram helps visualize how your oncologist pieces together your unique cancer biology to select the most effective and precise path forward.
Game-Changing Targeted Therapies
The development of targeted drugs has completely changed the game for treating stage 4 breast cancer. These treatments are engineered for patients whose tumors have specific biomarkers, which is why that initial diagnostic workup is so critical.
Comparing Modern Therapies For Stage 4 Breast Cancer
To make sense of the different approaches, it helps to see how they stack up. This table breaks down the main therapy types, how they work, and which cancer subtypes they're best suited for.
This variety of mechanisms allows us to choose a therapy that exploits a specific vulnerability in your cancer, leading to better outcomes and often, fewer side effects.
CDK4/6 Inhibitors
For women with ER-positive, HER2-negative breast cancer, CDK4/6 inhibitors have become a standard of care. These are oral medications that block two key proteins—CDK4 and CDK6—that tell cells to divide. When used with hormonal therapy, they have been shown to significantly delay cancer progression and help people live longer.
These drugs have truly transformed the treatment landscape. They've allowed many women to manage their metastatic disease for years, sometimes even decades, with a good quality of life. This is a huge step toward treating stage 4 breast cancer like a manageable chronic illness.
PARP Inhibitors
For patients who carry a BRCA1 or BRCA2 gene mutation, PARP inhibitors provide another powerful, targeted option. These drugs take advantage of a weakness in cancer cells that have this mutation. They block the cells' ability to repair their own DNA, which ultimately causes them to self-destruct.
Antibody-Drug Conjugates (ADCs)
ADCs are essentially "smart bombs" for fighting cancer. They combine a targeted antibody that seeks out a specific protein on the cancer cell's surface with a potent chemotherapy drug. This design allows for the direct delivery of chemotherapy to the tumor while largely sparing healthy cells. This method has produced incredible results in HER2-positive and even some triple-negative breast cancers. To go deeper on this, you can learn more about breast cancer targeted therapy in our detailed guide.
The Role Of Clinical Trials
It's important to remember that every single treatment we use today was once evaluated in a clinical trial. Participating in a trial can provide access to the next generation of therapies long before they become widely available. For anyone with stage 4 breast cancer, a clinical trial isn't a last resort; it's an excellent treatment option to consider at any point in your journey.
These studies are carefully designed to test the safety and effectiveness of new drugs or new combinations. Your oncology team can help you find trials that are a good match for your cancer subtype and treatment history, opening up another avenue of hope that's grounded in cutting-edge science. Here at Hirschfeld Oncology, we are dedicated to helping our patients explore these important opportunities.
Managing Your Symptoms and Quality of Life

When you're living with stage 4 breast cancer, the focus isn't just on treating the disease—it’s about living as fully and comfortably as possible. While powerful therapies work to control the cancer, an equally vital part of your care involves managing the symptoms and treatment side effects you experience day-to-day.
Your quality of life isn't an afterthought; it's at the very heart of your treatment plan. Taking a proactive approach to these challenges is what helps you maintain your strength, your independence, and your sense of self. It’s why we integrate symptom management from day one here at Hirschfeld Oncology.
The Essential Role of Palliative Care
Let's clear up one of the biggest myths in cancer care. When people hear "palliative care," they often jump to conclusions about hospice or end-of-life. That couldn't be further from the truth.
Think of palliative care as a specialized support system that should start the moment you're diagnosed. Its entire purpose is to provide relief from the symptoms, pain, and stress of a serious illness. Your oncology team focuses on the cancer; your palliative care team focuses on you and how you feel.
Palliative care isn't about giving up—it's about gaining control. It’s an extra layer of support that works in tandem with your cancer treatment to make every day better.
This is a true team effort. Palliative care brings together doctors, nurses, and other specialists who listen to your needs and goals. They then work right alongside you, your family, and your oncologist to build a plan that improves your daily comfort.
Common Symptoms and How to Manage Them
Living with metastatic breast cancer can bring physical challenges, but you don't have to simply endure them. There are so many effective strategies—both medical and lifestyle-based—that can help you feel much better.
Here are a few common issues we help patients navigate:
- Pain Management: This is our top priority. From targeted radiation that shrinks a painful tumor to carefully prescribed medications, we have many tools to keep pain under control.
- Fatigue: This isn't just being tired; it's a profound, whole-body exhaustion. We find that gentle movement like walking, learning to conserve energy, and focusing on nutrition can make a world of difference.
- Nausea and Appetite Loss: Thankfully, modern anti-nausea drugs are incredibly effective. A nutritionist can also be your best ally, helping you find foods that appeal to you and give your body the strength it needs.
Integrating Complementary Therapies
Beyond medicine, many people find tremendous comfort and relief from what we call complementary therapies. These approaches don't fight the cancer itself, but they are fantastic at easing symptoms and boosting your overall well-being.
It's all about finding what works for you. Some options to consider include:
- Acupuncture: Many patients report significant relief from chemotherapy-induced nausea and certain types of pain.
- Massage Therapy: A gentle, oncology-informed massage can be wonderful for reducing stress, anxiety, and muscle aches.
- Mindfulness and Meditation: These practices can be powerful tools for managing the emotional weight of a diagnosis, calming anxiety, and improving sleep.
As you focus on your physical symptoms, it’s just as important to acknowledge the emotional journey, including navigating the fear of losing someone you love. The key is to talk to your care team before trying anything new so we can make sure it’s safe and a good fit for your situation. At Hirschfeld Oncology, we are committed to a comprehensive plan that supports all of you—body, mind, and spirit.
Finding Your Partner in Advanced Cancer Care
When you're navigating a stage 4 breast cancer diagnosis, one of the most important steps is building a medical team you genuinely trust. You need a partner who sees you as a whole person, understands your life goals, and has the deep expertise to offer the most advanced solutions available. This journey is a true partnership, one that must be grounded in both compassion and leading-edge science.
This is especially true when you're seeking a second opinion or feel like you need options that go beyond the standard protocols you've been offered.
For patients in the New York City area, Hirschfeld Oncology is a dedicated resource for people living with advanced cancers. Our practice, led by Dr. Azriel Hirschfeld, was founded on the principle of providing personalized, hopeful, and effective care. We specialize in creating treatment plans that are as unique as the individuals we serve, always making sure every decision aligns with your quality of life.
A Different Approach to Stage 4 Care
At Hirschfeld Oncology, we think differently about managing advanced disease. We focus on innovative strategies that can turn it into a long-term, manageable condition. Our commitment is to find the most effective path forward with the least possible disruption to your daily life—a crucial part of living well with metastatic cancer.
This approach becomes vital for patients who feel they might be running out of options. We offer specialized therapies that aren't always widely available, including:
- Tailored Low-Dose Chemotherapy: This method, sometimes called metronomic therapy, works to control cancer growth while producing fewer of the disruptive side effects common with traditional chemo.
- Emerging Immunotherapies: We work to harness the power of your own immune system, helping it recognize and fight cancer cells more effectively.
- Targeted Agents: By understanding the specific genetic makeup of your tumor, we can select treatments that are precisely aimed at the cancer's vulnerabilities.
As you build your comprehensive care team, it's also helpful to think about practical support systems. This can include services like home medical equipment rentals that can significantly improve your comfort and daily living at home.
For those living with advanced cancer, practices like Hirschfeld Oncology in Brooklyn offer a different kind of support. With over 20 years of expertise, Dr. Azriel Hirschfeld delivers specialized regimens for stage 4 breast cancer patients, including immunotherapy, targeted therapy against specific mutations like PIK3CA, and low-dose chemotherapy. These plans are tailored to minimize toxicity and are well-suited for NYC's diverse communities, offering outpatient infusions and robust symptom control.
It's also vital to understand your full range of support options, like the key differences between palliative and hospice care. We've put together a guide where you can learn more about palliative care vs. hospice care to help clarify these choices.
If you are in Brooklyn, Williamsburg, or the surrounding areas and want to explore a collaborative and hopeful path forward, we invite you to request a consultation with our team.
Navigating Life with Stage 4 Breast Cancer: Your Questions Answered
When you hear the words "stage 4 breast cancer," it’s natural for your mind to race with questions—not just about treatments, but about your life. How will this affect my job? How do I tell my kids? What does the future look like? These are the real, human concerns that come with a diagnosis, and you deserve clear, compassionate answers.
Let's walk through some of the most common questions we hear from patients and their families. Our goal is to replace uncertainty with understanding, giving you the clarity you need to move forward.
Can I Keep Working During Treatment?
For many people, the answer is a resounding yes. Continuing to work, whether full-time or with some adjustments, can provide a much-needed sense of routine and purpose. It’s all about finding a balance that works for you.
The key is open communication. Talk with your employer about what you might need—perhaps a more flexible schedule or the ability to work from home on days you don't feel well. Just as importantly, keep your oncology team in the loop. We can help you anticipate side effects and schedule treatments in a way that minimizes disruption to your professional life. At Hirschfeld Oncology, we see this as a partnership to help you live your life as fully as possible.
How Should I Talk to My Family and Children About This?
There’s no perfect script for this conversation, and it’s one of the hardest parts of the journey. The best approach is usually one that is honest and tailored to who you're talking to. With kids, being age-appropriate is crucial.
What often helps is reassuring your loved ones that you have a plan. Let them know you have a team of doctors and nurses who are dedicated to taking care of you. Focusing on the support system you have in place—including them—can ease their fears and make them feel like part of the team. We can also connect you with social workers and support groups who specialize in helping families navigate these tough but essential conversations.
A diagnosis of stage 4 breast cancer doesn't just happen to one person; it happens to a family. Open, honest communication, grounded in hope, is the bedrock of the support system everyone will rely on.
What's the Difference Between Palliative Care and Hospice?
This is a really important question, and one that's widely misunderstood. Think of it this way: palliative care is an extra layer of support that focuses on improving your quality of life. It’s about managing symptoms, pain, and the stress that comes with a serious illness. It can—and should—start from the moment of diagnosis and happen right alongside your cancer treatments.
Hospice care is a specific type of care that begins when the decision has been made to stop treatments aimed at curing the cancer. The focus shifts entirely to comfort and ensuring the best possible quality of life during the final chapter. They are not the same thing, and embracing palliative care early can make a world of difference in your day-to-day well-being.
Is It Okay to Get a Second Opinion?
Absolutely. In fact, we encourage it. Getting a second opinion for a diagnosis as serious as stage 4 breast cancer is a smart and proactive step. It’s your health, and you need to feel completely confident in your treatment plan and the team delivering it.
A second opinion can confirm you’re on the right track, which brings incredible peace of mind. Or, it might open the door to a new clinical trial or a different therapeutic approach you hadn't considered. Any good oncologist will support your desire to be fully informed. It's why many patients come to a specialized practice like Hirschfeld Oncology—to gain new perspectives from a team focused on complex and advanced cancers.
At Hirschfeld Oncology, we know that hope is fueled by clarity. If you're looking for a second opinion or want to understand all the available treatment options for stage 4 breast cancer, our compassionate team is here to help.
You can learn more and request a consultation on our website: https://honcology.com/blog





.png)


.png)
.png)




